Hyperspectral Imaging for Biofluorescence Characterization: Advanced Techniques and Applications in Biomedical Research
This article explores the transformative role of hyperspectral imaging (HSI) in biofluorescence characterization for biomedical research and drug development.
Hyperspectral Imaging for Biofluorescence Characterization: Advanced Techniques and Applications in Biomedical Research
Abstract
This article explores the transformative role of hyperspectral imaging (HSI) in biofluorescence characterization for biomedical research and drug development. It covers the foundational principles of HSI, which captures both spatial and spectral information to create a detailed chemical fingerprint of samples. The scope extends to methodological advances, including excitation-scanning HSI to overcome signal strength limitations in fluorescence microscopy and the application of algorithms like linear unmixing for sensitive cellular signal detection. It addresses critical troubleshooting aspects, such as managing variable illumination in surgical settings and optimizing preprocessing pipelines for deep learning. Finally, the article provides a rigorous validation of HSI against established techniques like fluorescence angiography in clinical perfusion assessment and surgical microscopy for glioma detection, demonstrating its superior sensitivity and quantification capabilities. This comprehensive resource is tailored for researchers, scientists, and drug development professionals seeking to implement and optimize HSI in their work.
Unlocking Spectral Fingerprints: Core Principles and Advantages of Hyperspectral Biofluorescence Imaging
Hyperspectral imaging (HSI) is an advanced optical sensing technique that integrates the principles of spectroscopy and digital photography into a single system [1]. This integration enables the simultaneous acquisition of spatial and spectral data, capturing images of a scene across numerous contiguous spectral bands. The result is a three-dimensional dataset known as a hyperspectral data cube, which combines two spatial dimensions (x, y) with one spectral dimension (λ) [1]. Each pixel within this cube contains a continuous spectrum, often referred to as a spectral "fingerprint," that enables precise identification and characterization of materials based on their chemical composition [1].
The fundamental advantage of HSI over conventional imaging modalities lies in its exceptional spectral resolution. While standard RGB cameras capture only three broad spectral bands (red, green, and blue), and multispectral systems typically capture fewer than 20 discrete bands, hyperspectral imaging routinely captures over hundreds of spectral channels at high spectral resolution (commonly 5-10 nm) [1]. This extensive spectral coverage allows researchers to identify subtle yet diagnostically significant features, including molecular absorption bands and pigment-related transitions, which are often invisible or indistinct in conventional imaging [1].
In the context of biofluorescence characterization, HSI has demonstrated particular value due to its inherently non-destructive and label-free nature [1]. Unlike invasive biochemical assays or staining-based microscopy, HSI does not require physical contact or chemical labeling of samples, making it highly suitable for in situ and in vivo applications, continuous monitoring, and real-time diagnostics [2]. This Primer explores the underlying principles, methodological considerations, and practical applications of HSI, with emphasis on its growing role in biomedicine and drug development research.
Fundamental Principles and Technical Implementation
Physical Basis of Hyperspectral Imaging
The high-dimensional nature of hyperspectral data stems from fundamental physical interactions between incident radiation and target materials. When light interacts with matter, several processes occur including electronic transitions, molecular vibrations, scattering, and fluorescence [1]. These interactions, which vary according to the imaging modality and spectral domain, underpin the unique capability of HSI to provide non-destructive, label-free analyses of biological and material samples [1].
Hyperspectral imaging focuses primarily on the optical window of the electromagnetic spectrum, typically covering wavelengths from 380 to 2500 nm [1]. This range encompasses the visible light (400-700 nm), near-infrared (NIR), and short-wave infrared (SWIR) regions. The inclusion of the NIR region (800-2500 nm) is particularly valuable for biofluorescence applications as it corresponds to overtone and combinational vibrational modes of molecular bonds such as O─H, N─H, and C─H [2]. Furthermore, the NIR region offers significant benefits for biomedical applications due to the existence of "optical windows" from 650 to 1350 nm and above 1450 nm, where absorption and scattering are reduced, allowing light to penetrate deeper into biological tissues [2].
Hyperspectral Data Cube Structure and Acquisition
The primary data structure in HSI is the three-dimensional hyperspectral cube, which contains both spatial and spectral information [2]. As illustrated in Figure 1, this cube is formed by stacking images captured across contiguous wavelength bands, assigning a complete spectrum to each spatial pixel [2].
Figure 1. Hyperspectral data cube structure. The cube combines two spatial dimensions with one spectral dimension, capturing a complete spectrum for each pixel.
Two primary approaches exist for hyperspectral data acquisition in fluorescence microscopy: emission-scanning and excitation-scanning HSI [3]. Each method offers distinct advantages and trade-offs for biofluorescence characterization, as summarized in Table 1 and illustrated in Figure 2.
Table 1: Comparison of HSI Acquisition Modalities for Fluorescence Imaging
| Parameter | Emission-Scanning HSI | Excitation-Scanning HSI |
|---|---|---|
| Spectral Separation Method | Filters emission light across bands | Scans excitation wavelength |
| Excitation Source | Broad-band with band-pass filter | Tunable narrow-band illumination |
| Eission Detection | Broad-band or long-pass filter | Tunable filter or dispersive element |
| Signal Strength | Lower (signal divided across bands) | Higher (minimal emission filtering) |
| Photobleaching Risk | Higher | Lower |
| Best Suited For | Bright samples, fixed cells | Live-cell imaging, weak signals |
| Spectral Information | Emission spectrum | Excitation spectrum |
Figure 2. HSI acquisition modalities for fluorescence microscopy. Comparison of emission-scanning and excitation-scanning approaches for hyperspectral imaging.
For dynamic cell signaling studies, excitation-scanning HSI provides significant advantages due to its higher signal strength [3]. This approach utilizes the wavelength-dependent properties of the excitation spectrum of each fluorophore to perform spectral separation, while minimally processing the emission in the spectral dimension, resulting in stronger signals reaching the detector [3]. This enables increased imaging speeds and decreased photobleaching, crucial factors for live-cell imaging and kinetic studies [3].
Experimental Protocols for Biofluorescence Characterization
This protocol describes the implementation of excitation-scanning HSI for kinetic measurements of intracellular Ca²⁺ signals in human airway smooth muscle cells (HASMCs), based on the methodology reported by PMC [3].
Research Reagent Solutions
Table 2: Essential Materials for Excitation-Scanning HSI
| Reagent/Equipment | Specification | Function | Supplier Example |
|---|---|---|---|
| Human Airway Smooth Muscle Cells | Primary culture, passages 3-8 | Model system for Ca²⁺ signaling studies | N/A |
| Cal 520-AM | 5 µM in DMSO | Fluorescent Ca²⁺ indicator | AAT Bioquest |
| NucBlue Live ReadyProbes | 2 drops/mL | Nuclear counterstain | ThermoFisher Scientific |
| Laminin-coated Coverslips | 20 mm round | Cell adhesion substrate | Various |
| Dulbecco's Modified Eagle Medium | With 5% FBS and growth factors | Cell culture maintenance | GIBCO |
| Extracellular Buffer | 145 mM NaCl, 4 mM KCl, 1 mM MgCl₂, 10 mM HEPES, 10 mM glucose, 2 mM CaCl₂ | Physiological imaging solution | N/A |
| Excitation-Scanning HSI Microscope | Tunable excitation source, broad-band emission filter | Hyperspectral image acquisition | Custom or commercial |
Step-by-Step Procedure
Cell Culture and Preparation
- Culture HASMCs in Dulbecco's Modified Eagles Medium (DMEM) supplemented with 5% fetal bovine serum, basic fibroblast growth factor, epidermal growth factor, 100 U/mL penicillin, and 100 μg/mL streptomycin at pH 7.0 [3].
- Seed cells onto 20 mm laminin-coated round glass coverslips and incubate at 37°C and 5% CO₂ for 48 hours or until 70-80% confluency [3].
Fluorescent Labeling
- Prepare single-label control samples for system validation:
- For experimental samples: Prepare mixed-label samples using both Cal 520-AM and NucBlue labeling with identical concentrations and incubation times as single-label controls [3].
Hyperspectral Image Acquisition
- Transfer labeled coverslips to an appropriate imaging chamber (e.g., attoflour holder) covered with extracellular buffer [3].
- Configure excitation-scanning HSI system parameters:
- Set excitation wavelength range to cover absorption peaks of all fluorophores (typically 350-500 nm for Cal 520 and DAPI-channel dyes).
- Set emission detection using a broad-band or long-pass emission filter.
- Define spectral sampling interval (typically 5-10 nm) and exposure time per wavelength.
- Acquire time-lapse excitation-scanning HSI data with appropriate temporal resolution for the kinetic process being studied (e.g., 30-second intervals for Ca²⁺ oscillations).
Spectral Data Analysis
- Process raw HSI data using one of the following algorithms:
- Linear Unmixing (LU): Separates signals based on reference spectra [3].
- Constrained Energy Minimization (CEM): Minimizes energy from background while maintaining target response [3].
- Matched Filter (MF): Enhances response of target spectrum while suppressing background [3].
- Spectral Angle Mapper (SAM): Compares angles between spectral vectors [3].
- Apply theoretical sensitivity framework to filter pixels below minimum detectable limit.
- Extract quantitative Ca²⁺ signal traces from regions of interest.
- Process raw HSI data using one of the following algorithms:
Protocol 2: HyperNIR Spectral Phasor Imaging for Biofluorescence
This protocol describes the implementation of a fast NIR hyperspectral imaging approach using spectral phasor transformation (HyperNIR) for distinguishing NIR fluorophores with emission peaks less than 5 nm apart [2].
Research Reagent Solutions
Table 3: Essential Materials for HyperNIR Imaging
| Reagent/Equipment | Specification | Function | Notes |
|---|---|---|---|
| NIR Fluorophores | Single-walled carbon nanotubes (SWCNTs) or other NIR fluorophores | Biofluorescence labels | Tailorable as biosensors |
| Liquid Crystal Variable Retarder | Electrically tunable retardance | Spectral filtering element | Core component of HyperNIR |
| Linear Polarizers | High extinction ratio, NIR compatible | Polarization control | Two units required |
| NIR-Sensitive Camera | InGaAs detector or similar | NIR light detection | Typically 0.1 MP resolution |
| Optical Mounting Hardware | Cage system or custom mount | System alignment | Precision positioning required |
Step-by-Step Procedure
HyperNIR System Configuration
- Assemble optical module with two parallel linear polarizers (set at 45° with respect to the fast axis of the variable retarder) and a liquid crystal variable retarder (LCVR) placed between them [2].
- Align optical components to ensure collimated light path through the entire system.
- Connect LCVR to appropriate control electronics for rapid retardance adjustment.
Spectral Calibration
- Characterize the wavelength-dependent transmission of the system using known light sources.
- Determine the relationship between applied voltage to the LCVR and resulting retardance.
- Tune the retardance to cover the desired spectral range (900-1600 nm, adjustable in windows from 50 to 700 nm) [2].
- Optimize system for specific spectral region of interest by minimizing phasor calculation error.
Image Acquisition
- For each sample, acquire three key images:
- Cosine-filtered image: Set LCVR to create cosine-shaped spectral transmission.
- Sine-filtered image: Adjust LCVR to sine-shaped spectral transmission.
- Normalization image: Set retardance to zero for wavelength-independent transmission [2].
- Maintain consistent illumination and exposure settings across all three acquisitions.
- For each sample, acquire three key images:
Spectral Phasor Analysis
- Transform optical signals into 2D spectral phasor space using the acquired sine, cosine, and normalization images.
- Map each pixel into phasor space where position contains spectral information.
- Identify and separate distinct fluorophores based on their clustering in phasor space.
- Apply phasor analysis to distinguish fluorophores with emission peaks separated by less than 5 nm [2].
Data Processing and Analysis Methods
Preprocessing Strategies for Hyperspectral Data
Effective preprocessing of hyperspectral data is essential for optimal analysis results, particularly in biomedical applications. A recent comprehensive study compared various preprocessing techniques for hyperspectral deep learning-based cancer diagnostics, with findings relevant to biofluorescence characterization [4].
Table 4: Comparison of HSI Preprocessing Techniques for Biomedical Applications
| Preprocessing Step | Options | Performance Findings | Recommendations |
|---|---|---|---|
| Scaling | Normalization, Standardization | Standardization significantly improves both sensitivity and specificity compared to Normalization [4] | Use Z-score standardization for enhanced convergence |
| Spatial Context | Patch size 3, Patch size 5 | Larger input patch sizes enhance performance by capturing more spatial context [4] | Use larger patches (e.g., 5×5) when computational resources allow |
| Noise Reduction | 1D, 2D, 3D smoothing with Median, Gaussian, or Savitsky-Golay filters | Noise reduction unexpectedly degrades performance [4] | Apply smoothing cautiously; validate performance impact |
| Artifact Filtering | Blood filtering, Light reflection filtering | Blood filtering is more effective than filtering reflected light pixels [4] | Prioritize blood absorption artifact removal |
| Dataset Imbalance | Class weighting, Sample weighting | Addresses underrepresentation of target features [4] | Implement weighting strategies for imbalanced datasets |
Spectral Analysis Algorithms
For quantitative analysis of hyperspectral biofluorescence data, several algorithms have been compared for their effectiveness in dynamic cell signaling studies [3]:
Linear Unmixing (LU): Separates mixed fluorescence signals based on reference spectra of pure fluorophores. Demonstrates linear response to increasing Ca²⁺ concentrations and effective signal separation from autofluorescence [3].
Constrained Energy Minimization (CEM): Minimizes energy from background components while maintaining a strong response to the target signature. Effective for detecting weak signals in high-background environments [3].
Matched Filter (MF): Enhances the response of a target spectrum while suppressing the background. Shows similar linear response to LU for quantitative Ca²⁺ measurements [3].
Spectral Angle Mapper (SAM): Compares the angles between spectral vectors rather than their magnitudes. Less sensitive to illumination variations but may be less effective for quantitative measurements [3].
The selection of an appropriate algorithm should be guided by the specific application requirements, with LU and MF recommended for quantitative kinetic studies based on their demonstrated linear response to increasing analyte concentrations [3].
Applications in Biomedical Research and Drug Development
Hyperspectral imaging has shown significant potential across various domains of biomedical research and drug development. In cancer diagnostics, HSI has been applied for discrimination of pathological tissues in colorectal cancer [4], skin cancer [4], breast cancer [4], head and neck cancer [4], brain cancer [4], oral cancer [4], and gastric cancer [4]. The technology enables non-invasive, label-free identification of cancerous tissues based on their spectral characteristics, providing valuable intraoperative guidance and margin assessment [4].
In drug development, HSI facilitates high-content screening and mechanistic studies of drug effects through several approaches:
- Receptor Trafficking Studies: Monitoring of GPCR internalization and recycling using labeled ligands or fluorescent protein tags.
- Second Messenger Assays: Quantitative measurement of intracellular Ca²⁺, cAMP, IP₃, and other signaling molecules.
- Metabolic Activity Profiling: Label-free assessment of cellular metabolism through autofluorescence imaging of NADH, FAD, and other intrinsic fluorophores.
- Cytotoxicity and Viability Screening: Multiparametric assessment of drug effects using multiple fluorescent indicators simultaneously.
The non-destructive nature of HSI makes it particularly valuable for longitudinal studies where the same cells or tissues need to be monitored over extended periods, such as in time-course experiments of drug response or stem cell differentiation.
Emerging Trends and Future Perspectives
The field of hyperspectral imaging for biofluorescence characterization is rapidly evolving, with several emerging trends shaping its future development:
AI-Driven Analysis: Deep learning approaches, particularly convolutional neural networks (CNNs), are transforming HSI data processing by enabling automatic extraction of nonlinear spectral features without manual preprocessing [5]. Lightweight CNN architectures are being developed for resource-constrained applications, facilitating real-time analysis onboard satellite platforms or portable devices [5].
Miniaturization and Portability: Advances in optics and detector technologies are driving the development of compact, portable HSI systems suitable for point-of-care diagnostics and field applications [1].
High-Speed Acquisition: New approaches such as the HyperNIR spectral phasor method are addressing the intrinsic speed limitations of traditional HSI, enabling hyperspectral frame rates of 0.2 s⁻¹ [2].
Cross-Modal Fusion: Integration of HSI with other imaging modalities (e.g., MRI, CT, photoacoustic imaging) provides complementary information and enhances diagnostic capability.
Foundation Models: Development of large-scale pretrained models for HSI analysis promises to improve generalizability across tasks, domains, and sensor types [1].
As these trends continue, hyperspectral imaging is poised to become an increasingly accessible and powerful tool for biofluorescence characterization in basic research, drug development, and clinical applications.
Biofluorescence hyperspectral imaging (HSI) represents a transformative approach in analytical science, enabling non-destructive, label-free chemical characterization across diverse research domains. This technique captures both spatial and spectral information from autofluorescent samples or those labeled with exogenous fluorophores, providing a comprehensive molecular fingerprint without the need for destructive sample preparation. The integration of advanced chemometric algorithms and computational imaging approaches has significantly enhanced our ability to extract meaningful chemical information from complex biological and material systems. This application note details the fundamental principles, experimental protocols, and key applications of hyperspectral biofluorescence imaging, providing researchers with practical frameworks for implementation in pharmaceutical development, biomedical research, and agricultural science.
Hyperspectral biofluorescence imaging merges the molecular specificity of fluorescence spectroscopy with spatial mapping capabilities, creating a powerful tool for non-destructive material characterization. Unlike conventional fluorescence microscopy that relies on measurements at single excitation and emission bands, HSI acquires the complete emission spectrum at each spatial location within a sample, generating a three-dimensional dataset (x, y, λ) often called a "hypercube" [6]. This comprehensive spectral data enables researchers to distinguish between multiple fluorescent signals even when they significantly overlap, providing unprecedented capability for analyzing complex chemical compositions without damaging samples [7].
The "biofluorescence advantage" stems from several key benefits: non-destructive operation that preserves sample integrity, label-free detection that leverages intrinsic fluorescent properties, high molecular specificity through unique spectral signatures, and exceptional sensitivity capable of detecting fluorescent signals as low as 15% of the autofluorescence intensity in highly autofluorescent tissues [6]. These characteristics make the technology particularly valuable for applications where sample preservation is critical, such as forensic evidence analysis [8], pharmaceutical tablet characterization [9], and longitudinal biological studies [7].
Key Applications and Performance Metrics
Application Domains
Table 1: Key Application Areas of Hyperspectral Biofluorescence Imaging
| Application Domain | Specific Use Cases | Key Advantages |
|---|---|---|
| Pharmaceutical Analysis | Characterization of active pharmaceutical ingredients (APIs) in tablets [9] | Non-destructive quality control; rapid in-line analysis |
| Forensic Science | Identification of bio-fluids (blood, urine, saliva, sperm) on cotton supports [8] | Non-destructive evidence preservation; minimal sample preparation |
| Biomedical Research | Detection of GFP-expressing cells in highly autofluorescent lung tissue [6] | High sensitivity in challenging environments; accurate cell quantification |
| Agricultural Science | Chlorophyll content monitoring in rice leaves [10] | Non-destructive plant health assessment; precision agriculture enablement |
| Food Safety | Prediction of microbial growth in chicken breasts [11] | Rapid contamination assessment; non-invasive quality monitoring |
Quantitative Performance Metrics
Table 2: Performance Metrics of Hyperspectral Biofluorescence Imaging Across Applications
| Application | Detection Sensitivity | Accuracy/Performance Metrics | Reference |
|---|---|---|---|
| GFP Detection in Lung Tissue | GFP intensity as low as 15% of autofluorescence | Zero false positives detected; substantially better than single-band thresholding [6] | |
| Chlorophyll Detection in Rice | N/A | RMSE-Train: 0.26, RMSE-Test: 0.29, RPD: 2.64 (CNN+LSTM model with fluorescence data) [10] | |
| Bio-fluid Identification | N/A | Successful discrimination of blood, urine, saliva, and sperm spots on cotton using SIMCA, PCA, and PLS-DA [8] | |
| Pharmaceutical API Characterization | N/A | Complete separation of ibuprofen, acetylsalicylic acid, and paracetamol using first two principal components [9] |
Experimental Protocols
General Workflow for Hyperspectral Fluorescence Imaging
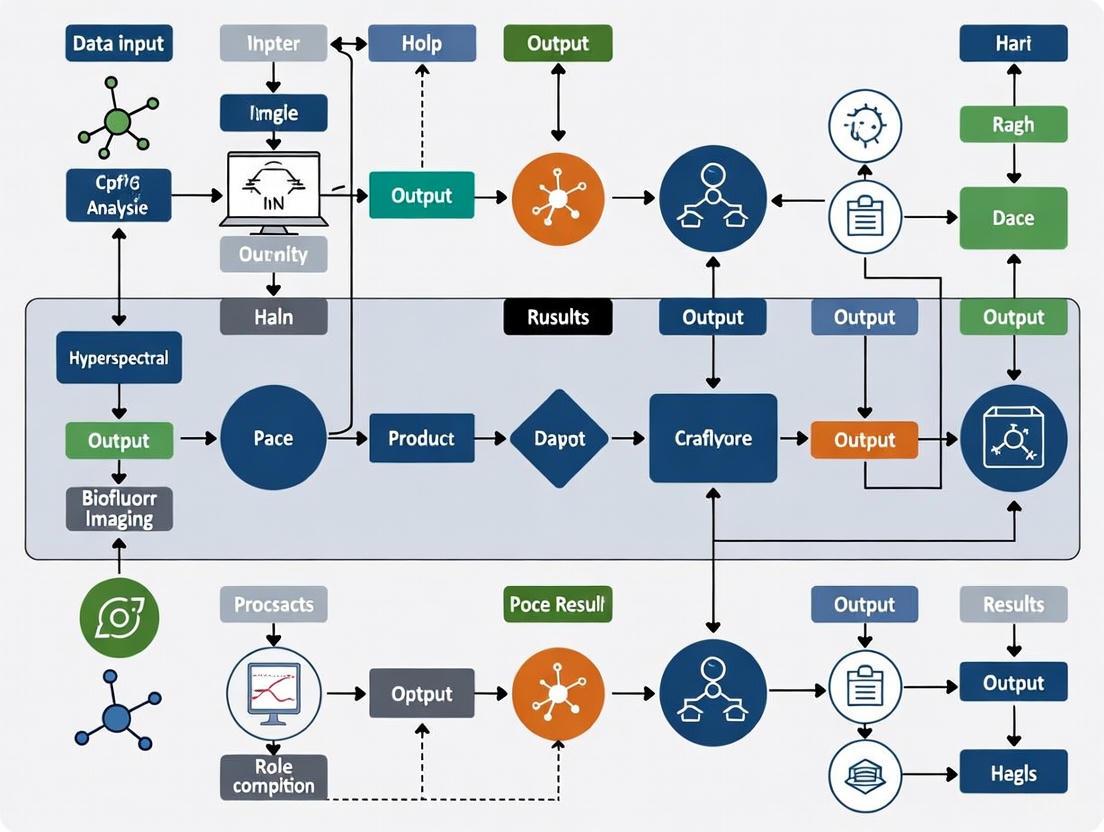
The following diagram illustrates the comprehensive workflow for hyperspectral fluorescence imaging experiments, from sample preparation through data analysis:
Protocol 1: Detection of Bio-fluids on Forensic Substrates
Application: Identification of blood, urine, saliva, and sperm spots on cotton fabric for forensic analysis [8]
Materials and Reagents:
- White cotton fabric substrates
- Reference bio-fluids (blood, urine, saliva, sperm)
- Raman hyperspectral imaging system
- MATLAB or similar analytical software with chemometric tools
Procedure:
- Sample Preparation:
- Deposit controlled volumes (2-10 µL) of bio-fluids onto white cotton fabric
- Allow samples to air-dry under controlled conditions (temperature, humidity)
- Prepare replicate samples for validation
Instrument Configuration:
- Configure Raman hyperspectral imaging system with appropriate laser wavelengths
- Set spatial resolution to capture fiber-level details
- Calibrate instrument using standard reference materials
Data Acquisition:
- Acquire hyperspectral images across appropriate spectral range (e.g., 500-1800 cm⁻¹ Raman shift)
- Ensure sufficient spectral resolution (typically 4-8 cm⁻¹) for molecular discrimination
- Include control samples (pure cotton substrate) in each imaging session
Data Analysis:
- Apply preprocessing: cosmic ray removal, fluorescence background subtraction, vector normalization
- Implement SIMCA for initial pixel classification and detection of bio-fluid regions
- Use PCA to explore spectral variance within and between bio-fluid classes
- Apply PLS-DA to build predictive models for bio-fluid identification
- Validate models using cross-validation and independent test sets
Technical Notes: This methodology enables non-destructive analysis of forensic evidence, preserving samples for subsequent DNA analysis or other confirmatory tests. The approach successfully discriminates between forensically relevant bio-fluids based on their intrinsic molecular signatures without chemical pretreatment [8].
Protocol 2: Detection of GFP-expressing Cells in Autofluorescent Tissues
Application: Identification and quantification of GFP-labeled pulmonary microvascular endothelial cells in highly autofluorescent lung tissue [6] [12]
Materials and Reagents:
- Lung tissue sections (10 μm cryoslices)
- GFP-expressing PMVECs and vector control cells
- Hoechst 33342 nuclear stain (5 μg/mL)
- Fluorescent mounting medium
- Custom hyperspectral imaging fluorescence microscope with AOTF
- MATLAB with custom analysis scripts
Procedure:
- Sample Preparation:
- Perfuse GFP+ or vector control PMVECs into pulmonary circulation of CD rats
- Fix perfused lungs in OCT compound
- Prepare 10 μm cryosections using cryostat
- Stain with Hoechst 33342 (0.225 μM) for nuclear visualization
- Mount with fluorescent mounting medium
Instrument Configuration:
- Configure hyperspectral microscope with 40X oil immersion objective
- Set excitation wavelength to 430 nm for GFP imaging
- Set AOTF to acquire emission from 450-700 nm in 5 nm increments
- Use 8.5 nm FWHM bandwidth and 2 second exposure per spectral band
Data Acquisition:
- Acquire hyperspectral image stacks from multiple tissue regions
- Include control samples: GFP+ cell monolayers, vector control tissues, blank slides
- Acquire Hoechst images using 360 nm excitation and 450 nm emission for nuclear reference
Data Analysis:
- Perform background subtraction and flat-field spectral correction
- Extract pure spectra from control samples for spectral library development
- Apply non-negative least squares linear unmixing to resolve GFP signal from autofluorescence
- Validate detection sensitivity using "what-if" scenarios with artificially added GFP signals
- Establish detection thresholds based on histogram analysis of unmixed signal distributions
Technical Notes: This approach enables accurate detection of GFP-expressing cells even when GFP intensity is as little as 15% of the autofluorescence intensity. The method achieves zero false positives compared to standard thresholding approaches, which produce substantial false positives [6].
Protocol 3: Chlorophyll Monitoring in Rice Leaves
Application: Non-destructive assessment of chlorophyll content in rice leaves using hyperspectral and fluorescence imaging [10]
Materials and Reagents:
- Rice leaf samples (Ya5You5217 cultivar)
- GaiaSorter Hyperspectral Sorter or equivalent system
- SPAD device for reference measurements
- MATLAB or Python with machine learning libraries
Procedure:
- Sample Collection:
- Collect rice leaf samples from experimental fields (minimum 90 samples for robust models)
- Include leaves representing various health states and growth stages
- Perform reference chlorophyll measurements using SPAD device or chemical analysis
Spectral Data Acquisition:
- Acquire hyperspectral images using GaiaSorter Hyperspectral Sorter
- Collect fluorescence spectral data using appropriate excitation/emission settings
- Ensure consistent illumination and measurement geometry across samples
Feature Extraction:
- Apply IVSO-IVISSA (Iteratively Variable Subset Optimization–Interval Variable Iterative Space Shrinkage Approach) for feature selection
- Identify characteristic spectral bands correlated with chlorophyll content
- Extract both hyperspectral and fluorescence spectral features
Model Development:
- Implement CNN+LSTM (Convolutional Neural Network + Long Short-Term Memory) architecture
- Train models to predict chlorophyll content from spectral features
- Validate models using cross-validation and independent test sets
- Compare performance with traditional machine learning algorithms (PLS, SVM)
Technical Notes: The combined CNN+LSTM model with fluorescence spectrum data demonstrates superior prediction performance (RMSE-Test: 0.29, RPD: 2.64) compared to hyperspectral data alone, enabling rapid, non-destructive crop health monitoring for precision agriculture applications [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Hyperspectral Biofluorescence Studies
| Reagent/Material | Function/Application | Example Usage |
|---|---|---|
| Hoechst 33342 | Nuclear counterstain | Cell nucleus identification in tissue sections [6] [12] |
| Green Fluorescent Protein (GFP) | Cellular labeling | Tracking and quantification of specific cell populations [6] [12] |
| Optimal Cutting Temperature (OCT) Compound | Tissue embedding medium | Cryosection preparation for tissue imaging [6] |
| Fluorescent Mounting Medium | Slide mounting | Preservation of fluorescence and reduction of photobleaching [6] |
| Polytetrafluoroethylene (PTFE) | Reflection standard | UV illumination homogenization in pharmaceutical applications [9] |
| Active Pharmaceutical Ingredients (APIs) | Target analytes | Pharmaceutical tablet characterization [9] |
Data Processing and Analysis Approaches
Spectral Analysis Workflow
The following diagram illustrates the spectral data processing pathway from raw acquisition to final interpretation:
Advanced Analysis Methods
Spectrally Encoded Enhanced Representations (SEER): This approach, based on the phasor method, transforms wavelength space into information-rich color maps for intuitive RGB visualization. SEER enables rapid visualization of subtle spectral differences during data acquisition and pre-processing, significantly enhancing interpretability of complex hyperspectral datasets [7]. The method involves five key steps: (1) Fourier transformation of spectral data, (2) histogram representation of phasor plot, (3) spatially lossless spectral denoising, (4) assignment of RGB colors based on phasor position, and (5) remapping of original dataset colors based on SEER results.
Compressive Fluorescence Microscopy (CFM): This innovative approach implements compressed sensing theory to reduce data acquisition requirements in fluorescence microscopy. By using patterned illumination and computational reconstruction, CFM enables image acquisition with undersampling ratios up to 32 for standard imaging and 64 for hyperspectral imaging, dramatically reducing acquisition time and data storage requirements while maintaining image quality [13].
Hyperspectral biofluorescence imaging represents a powerful paradigm for non-destructive, label-free chemical characterization across diverse scientific domains. The methodologies outlined in this application note provide researchers with robust frameworks for implementing these techniques in fields ranging from pharmaceutical development to agricultural science and biomedical research. The continuous advancement of computational analysis methods, including machine learning approaches and innovative visualization techniques like SEER, continues to expand the capabilities and applications of this technology.
As hyperspectral imaging systems become more accessible and computational methods more sophisticated, the "biofluorescence advantage" of non-destructive, label-free chemical characterization is poised to become increasingly integral to research and quality control workflows where sample preservation and comprehensive molecular information are paramount.
Hyperspectral imaging (HSI) has emerged as a transformative tool for biofluorescence characterization, enabling the non-invasive, label-free analysis of biological samples by simultaneously capturing spatial and spectral information. This capability is crucial for advanced research in drug development, where understanding subtle biochemical interactions and cellular responses is paramount. The performance of a hyperspectral system is fundamentally dictated by its core hardware components: the detector camera, the spectral dispersion mechanism, and the illumination sources. This article provides detailed application notes and protocols for these key components, framed within the context of configuring a hyperspectral imaging system for biofluorescence research. We summarize critical performance data in structured tables and provide explicit experimental methodologies to guide researchers and scientists in optimizing their systems for high-fidelity, reproducible results.
The Hyperspectral Imaging Pipeline and Component Integration
The process of generating a hyperspectral data cube—a three-dimensional dataset comprising two spatial dimensions and one spectral dimension—relies on a specific sequence of hardware components. The following diagram illustrates this integrated workflow and the role of each key component.
Core Hardware Components: Specifications and Selection Criteria
Scientific Detectors: sCMOS vs. EMCCD
The detector is a critical element that converts incoming photons into a quantifiable electronic signal. For biofluorescence characterization, where signals can be weak, the choice between sCMOS and EMCCD technology is fundamental [14] [15] [16].
Table 1: Performance Comparison of sCMOS and EMCCD Detectors
| Parameter | sCMOS | EMCCD | Implication for Biofluorescence Imaging |
|---|---|---|---|
| Read Noise | ~1.0–1.9 electrons (rms) [15] | <1 electron (with EM gain) [15] [16] | EMCCD superior for ultra-low-light, single-photon detection. |
| Quantum Efficiency (QE) | Up to 95% (back-illuminated) [16] | >95% (back-illuminated) [15] | Both high; EMCCD has a slight edge in photon collection. |
| Frame Rate | >100 fps (at full frame) [16] | ~26 fps (1024x1024 sensor) [15] | sCMOS is ideal for high-speed dynamic processes. |
| Dynamic Range | 16-bit, up to 53,000:1 [16] | High, but limited by EM gain noise [15] | sCMOS better for capturing both bright and dim features in one image. |
| Spatial Resolution | Multi-megapixel (e.g., 5.5 MP) [15] | Typically ~1 MP or less [15] [16] | sCMOS provides a larger field of view and finer spatial detail. |
| Multiplicative Noise | None [15] | Present (factor of √2) [15] | sCMOS provides superior signal-to-noise at medium-high light levels. |
| Typical Cost | \$5,000–\$20,000 [16] | \$20,000–\$30,000 [16] | sCMOS is more cost-effective for most non-single-molecule applications. |
Application Note: The decision between sCMOS and EMCCD should be driven by the specific photon flux of the experiment. sCMOS cameras are the preferred choice for the majority of biofluorescence applications due to their excellent balance of speed, resolution, dynamic range, and sensitivity [14] [15]. They are particularly suited for live-cell imaging, spectral imaging, and high-speed kinetics where photon counts are not limiting. EMCCD cameras remain the gold standard for the most demanding low-light applications, such as single-molecule localization microscopy (e.g., STORM, PALM) or tracking low-copy-number biomarkers, where their single-photon sensitivity is critical [15] [16].
Spectral Dispersion Components: Tunable Filters and Gratings
The imaging spectrometer, housing the spectral dispersion element, is the core component that distinguishes HSI from conventional imaging [1].
Table 2: Comparison of Spectral Dispersion Technologies
| Technology | Mechanism | Spectral Resolution | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Diffraction Grating | Wavelength separation via diffraction angles. | High (e.g., 5-10 nm) [1] | High light throughput, mechanical stability, fast spectral acquisition. | Complex data cube reconstruction (scanning). |
| Liquid Crystal Tunable Filter (LCTF) | Electrically controlled birefringence [1]. | Moderate to High | Flexible, random wavelength access, no moving parts. | Lower light throughput compared to gratings. |
| Acousto-Optic Tunable Filter (AOTF) | Radiofrequency-controlled diffraction in a crystal [1]. | High | Very fast wavelength switching (microseconds). | Higher cost, more complex electronics. |
| Prism | Wavelength-dependent refraction [1]. | Moderate (non-linear dispersion) | Robustness and stability. | Non-linear dispersion complicates spectral calibration. |
Application Note: For high-speed, bright-field hyperspectral imaging (e.g., in transmitted light modes), grating-based spectrometers coupled with sCMOS cameras are often optimal due to their high throughput and speed. For fluorescence hyperspectral imaging, where light levels may be lower and out-of-band rejection is critical, LCTFs or AOTFs provide excellent performance by selectively isolating specific emission bands without the need for physical movement [1].
Precise illumination is vital, especially for fluorescence excitation-emission matrix (EEM) approaches, which map fluorescence characteristics across multiple excitation and emission wavelengths [17] [18].
Table 3: Illumination Sources for Biofluorescence HSI
| Source Type | Spectral Range | Key Features | Application Context |
|---|---|---|---|
| Tunable LEDs | Discrete wavelengths from UV to NIR. | Long lifetime, stable output, compact, cost-effective. | Ideal for EEM-based systems; allows programmable excitation [18]. |
| Xenon Arc Lamps | Broadband (UV-Vis-NIR). | High intensity, continuous spectrum. | Requires external bandpass filters for specific excitation. |
| Laser Sources | Discrete, high-intensity lines. | Very high power density, monochromatic. | Best for techniques like CARS; requires safety precautions [14]. |
Application Note: The trend in modern HSI system design is toward LED-based illumination due to its stability, longevity, and the ease with which multiple discrete wavelengths can be integrated and controlled electronically. This is particularly suited for building optimized Fluorescence Imaging Systems (FIS) guided by EEM data, as it allows for the precise selection of excitation wavelengths that target specific fluorescent compounds (e.g., chlorophyll, flavonoids, NADH) [18].
Experimental Protocols for System Characterization
Protocol: Detector Performance Validation for Low-Light Fluorescence
This protocol assesses whether a detector (sCMOS or EMCCD) meets the sensitivity requirements for a given biofluorescence application.
Sample Preparation:
- Prepare a dilution series of a stable fluorophore (e.g., Fluorescein, Rhodamine) spanning a concentration range expected in your biological samples.
- Spot 1 µL of each dilution onto a clean glass slide and create a sealed preparation.
Image Acquisition:
- Mount the slide on the HSI microscope stage.
- Set the illumination intensity to a low, non-saturating level and keep it constant for all acquisitions.
- For sCMOS: Set the camera to its lowest read noise mode and a 16-bit dynamic range. Acquire images at a fixed exposure time (e.g., 100 ms, 500 ms, 1 s).
- For EMCCD: Start with EM gain at 1 (off) to characterize baseline performance. Then, incrementally increase the EM gain until the signal from the dimmest detectable sample is sufficiently above the background. Record the corresponding EM gain setting.
Data Analysis:
- Signal-to-Noise Ratio (SNR): For each fluorophore spot and each camera setting, measure the mean signal intensity in a Region of Interest (ROI) and the standard deviation of the signal in a background ROI. Calculate SNR as (MeanSignal - MeanBackground) / Std_Background.
- Dynamic Range: Image a sample with both very bright and very dim features. Confirm that the detector can resolve the dimmest feature without noise saturation while the brightest feature is not pixel-saturated.
- Validation Criterion: The detector is suitable if the SNR for the target signal intensity is ≥ 5-10 under the intended experimental acquisition conditions.
Protocol: Spectral Calibration and Illumination Optimization
This protocol ensures accurate wavelength assignment and selects optimal excitation wavelengths for a target fluorophore.
Spectral Calibration:
- Use a calibration lamp with known emission lines (e.g., Mercury-Argon lamp).
- Acquire spectra of the lamp using your HSI system.
- Plot the known peak wavelengths against the corresponding pixel positions on the detector. Fit a polynomial function (linear or quadratic) to create a wavelength-pixel mapping model.
Excitation-Emission Matrix (EEM) Profiling:
- Place a sample of the pure target fluorophore (e.g., a key cellular metabolite) in the system.
- Using a tunable excitation source (e.g., a tunable laser or LED array), systematically step through a range of excitation wavelengths (λ_ex).
- At each λex, acquire the full emission spectrum (λem).
- Construct a 3D EEM plot (Excitation Wavelength vs. Emission Wavelength vs. Fluorescence Intensity) [18].
Illumination Selection:
- Analyze the EEM to identify the peak excitation wavelength (λexmax) for the target fluorophore.
- For multi-fluorophore imaging, analyze the EEMs of all targets to select 2-3 excitation wavelengths that provide the best spectral separation (discriminatory power) between them, minimizing cross-talk [19] [18]. Studies show that transitioning from single to dual illumination significantly enhances performance with diminishing returns beyond two illuminations [19].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Materials for Hyperspectral Biofluorescence Experiments
| Item | Specification/Example | Function in the Experiment |
|---|---|---|
| Standard Fluorophores | Fluorescein, Rhodamine B, Nile Blue | System calibration, sensitivity validation, and positive controls. |
| Reference Standards | Wavelength calibration lamp (Hg/Ar), Spectralon reflectance tile | Spectral calibration and radiometric correction of the HSI system. |
| Biological Stains | DAPI, Hoechst (nucleus); MitoTracker (mitochondria); FM dyes (membrane) | Labeling specific cellular compartments for spatial-spectral analysis. |
| Metabolic Co-factors | NADH, FAD (autofluorescent) | Label-free monitoring of cellular metabolism and redox state. |
| Cell Culture Reagents | Phenol-red free medium, Fetal Bovine Serum (FBS), PBS buffer | Maintaining cell health and minimizing background fluorescence during live-cell HSI. |
| Microplates/Slides | Glass-bottom dishes, Black-walled 96-well plates | Sample mounting; black walls reduce cross-well fluorescence. |
The successful implementation of hyperspectral imaging for biofluorescence characterization hinges on a deliberate and informed selection of hardware components. As detailed in these application notes, sCMOS detectors generally offer the best balance of performance for most dynamic, live-cell imaging applications, while EMCCDs remain indispensable for single-photon-counting experiments. The choice of spectral dispersion technology should align with the required speed and light throughput, with tunable filters like LCTFs and AOTFs offering significant flexibility for fluorescence EEM studies. Finally, the move toward programmable, multi-wavelength LED illumination enables the precise excitation control needed to dissect complex biochemical environments. By following the provided protocols for system validation and calibration, researchers in drug development can establish robust, reliable, and highly informative HSI platforms to advance their characterization of biological systems.
Hyperspectral imaging (HSI) is an advanced optical sensing technique that captures both spatial and spectral information from a sample, generating a three-dimensional data cube often referred to as a hyperspectral cube [1]. This cube contains detailed spectral information obtained by measuring reflectance or radiance across finely resolved spectral intervals, enabling precise identification and characterization of materials, biological tissues, and environmental surfaces [1]. Unlike conventional imaging modalities, HSI typically captures hundreds of narrow spectral channels within and beyond the visual spectral range, providing a continuous spectrum for each pixel that allows identification based on chemical composition [20].
Despite its powerful capabilities, traditional HSI faces significant limitations. Conventional methods rely on spatial or spectral scanning, which makes the technique intrinsically slow and limits its application in dynamic biological systems [2] [21]. The near-infrared (NIR) range (800-2500 nm) is particularly advantageous for biomedical and environmental applications because it falls into the tissue transparency window and contains vibrational overtone and combination modes useful for molecular fingerprinting [2]. However, standard HSI approaches struggle to capture rapid biological processes in this spectrum.
The spectral phasor approach transforms this landscape by providing a fit-free, high-speed method for hyperspectral imaging. This approach maps complex spectral information from each pixel into a 2D polar plot (phasor plot), where the angular position represents the center of mass of the emission spectrum, and the distance from the center indicates the spectral width [22] [21]. By performing this transformation directly in hardware using specialized optical filters, the method achieves dramatic improvements in imaging speed while maintaining high spectral resolution [2] [21].
The HyperNIR system implements a tunable phasor-based approach to NIR hyperspectral imaging using polarization optics to generate wavelength-dependent sine- and cosine-filtering [2]. The core optical module consists of two parallel linear polarizers and a liquid crystal variable retarder (LCVR) that transforms optical signals directly into a 2D spectral phasor space with just three images [2].
Optical Configuration and Working Principle
The HyperNIR module features two linear polarizers oriented at 45° with respect to the fast axis of the variable retarder [2]. NIR light from fluorescence, reflected, or transmitted signals first passes through the initial polarizer, which filters the 45° component. The LCVR then imposes a variable retardation, creating an elliptically polarized beam dependent on wavelength. The second polarizer filters the 45° component of this elliptically polarized light, resulting in a wavelength-dependent transmission described by the equation:
[ T(R, \lambda) = \frac{I}{I_0} = \frac{1}{2} \left[ 1 + \cos \left( \frac{2\pi R}{\lambda} \right) \right] ]
where (R) represents the retardance and (\lambda) the wavelength [2]. This configuration generates sine- and cosine-shaped spectral transmissions that can be spectrally shifted by modulating the retardance, enabling the system to cover spectral ranges from 900 to 1600 nm in windows tunable from 50 to 700 nm [2].
Key Advantages Over Conventional HSI
The HyperNIR system addresses several critical limitations of conventional hyperspectral imaging:
- Speed: Achieves hyperspectral frame rates of 0.2 s⁻¹, limited only by the switching rate of the LCVR, compared to much slower scanning approaches [2]
- Spectral Resolution: Can distinguish NIR fluorophores with emission peaks less than 5 nm apart [2]
- Hardware Efficiency: Uses full camera resolution without the spatial compromise of mosaic-pattern or light-field snapshot cameras [2]
- Cost-Effectiveness: Components start at approximately 2000 €, significantly less than custom-built interference filters [2]
- Adaptability: The LCVR can be electronically switched between sine, cosine, and no spectral filtering modes, enabling flexible experimental designs [2]
Experimental Protocols
Protocol 1: HyperNIR System Calibration and Operation
Purpose: To calibrate the HyperNIR system for hyperspectral imaging of samples in the NIR range (900-1600 nm) [2].
Materials:
- HyperNIR system with LCVR module
- NIR-compatible camera (InGaAs recommended)
- Standard NIR fluorophores or reflectance standards
- Computer with control software
Procedure:
System Setup
- Mount the HyperNIR module between the microscope/imager and the NIR camera
- Ensure linear polarizers are oriented at 45° relative to the LCVR fast axis
- Connect LCVR to controller and computer
Spectral Range Calibration
- Set desired spectral window (50-700 nm range within 900-1600 nm)
- Apply voltage sequences to LCVR to achieve sine and cosine filtering modes
- Capture reference images using NIR standards with known spectra
- Verify transmission function matches theoretical expectations
Image Acquisition
- For each sample position, acquire three images:
- Image with sine spectral filtering
- Image with cosine spectral filtering
- Reference image without spectral filtering (retardance set to zero)
- Maintain consistent exposure times across acquisitions
- For each sample position, acquire three images:
Phasor Calculation
- For each pixel, calculate real (G) and imaginary (S) phasor components: [ G = \frac{I{\text{cosine}}}{I{\text{reference}}}, \quad S = \frac{I{\text{sine}}}{I{\text{reference}}} ]
- Plot phasor coordinates for each pixel on 2D phasor plot
- Apply clustering algorithms to identify distinct spectral signatures
Troubleshooting Tips:
- If phasor points appear compressed, adjust LCVR voltage to optimize spectral range
- For low signal-to-noise, increase exposure time or sample concentration
- Verify polarization alignment using control samples
Protocol 2: NIR Fluorescence Hyperspectral Imaging of Fluorophores
Purpose: To distinguish NIR fluorophores with closely spaced emission peaks using HyperNIR phasor analysis [2].
Materials:
- NIR fluorophores (e.g., single-walled carbon nanotubes, organic NIR dyes)
- Appropriate solvent and sample chambers
- Excitation source matched to fluorophore absorption
- HyperNIR system calibrated per Protocol 1
Procedure:
Sample Preparation
- Prepare fluorophore solutions at optimal concentrations for detection
- For comparison, select fluorophores with emission peaks separated by <10 nm
- Deposit samples in designated wells or imaging chambers
Image Acquisition
- Set excitation wavelength appropriate for target fluorophores
- Acquire sine, cosine, and reference images for each sample
- Ensure minimal bleed-through between channels
Data Analysis
- Transform each pixel to phasor space
- Identify clusters corresponding to different fluorophores
- Calculate phasor distance between fluorophore species
- Verify separation of fluorophores with <5 nm peak separation
Validation
- Compare with conventional spectrometer measurements if available
- Confirm linear combination properties by analyzing mixed samples
Protocol 3: Label-Free Hyperspectral NIR Reflectance Imaging
Purpose: To identify material compositions and monitor biological processes without labeling using NIR reflectance hyperspectral imaging [2].
Materials:
- Test materials (plastic polymers, plant samples)
- Reference standards for validation
- HyperNIR system with reflectance illumination
Procedure:
System Configuration for Reflectance
- Arrange illumination at appropriate angle to minimize specular reflection
- Set spectral range to target specific molecular vibrations (O-H, C-H, N-H bonds)
- Optimize camera exposure for reflectance mode
Sample Imaging
- Position samples to ensure flat field of view
- Acquire hyperspectral dataset using three-image protocol
- Include background reference measurements
Spectral Analysis
- Transform reflectance data to phasor space
- Identify distinct clusters for different materials
- For plant samples, monitor phasor position shifts indicating water content changes
Data Interpretation
- Correlate phasor positions with known material properties
- Track temporal changes in phasor coordinates for dynamic processes
- Generate false-color maps based on phasor cluster membership
Performance Metrics and Applications
Table 1: Performance Characteristics of HyperNIR Spectral Phasor Imaging
| Parameter | Performance | Comparison to Conventional HSI |
|---|---|---|
| Imaging Speed | 0.2 s⁻¹ frame rate | 10-100x faster than scanning methods [21] |
| Spectral Resolution | <5 nm fluorophore separation | Comparable to scanning spectrophotometers [2] |
| Spatial Resolution | Full camera resolution maintained | Superior to mosaic-pattern snapshot cameras [2] |
| Spectral Range | Tunable from 900-1600 nm | Adaptable versus fixed-range systems [2] |
| Light Throughput | 64% average filter transmission | Higher than dispersive scanning systems [21] |
| Cost | ~2000 € for core components | Significantly less than custom interference filters [2] |
Table 2: Application Examples for HyperNIR Spectral Phasor Imaging
| Application Domain | Specific Use Case | Key Advantage |
|---|---|---|
| Biomedical Imaging | Metabolic imaging of live tissues [21] | Minimal phototoxicity enables long-term imaging |
| Environmental Monitoring | Plastic polymer identification [2] | Label-free chemical discrimination |
| Agricultural Science | Plant water uptake monitoring [2] | Non-destructive temporal tracking |
| Cell Biology | Organelle tracking in 3D cultures [21] | High speed enables 5D (x,y,z,λ,t) imaging |
| Drug Development | Membrane order assessment with environment-sensitive dyes [22] | Fit-free analysis of complex systems |
| Food Safety | Bacterial biofilm detection [23] | Rapid, non-contact inspection |
Data Analysis Workflow
The phasor analysis approach provides a fit-free method for analyzing hyperspectral data without requiring a priori knowledge of spectral profiles, which is particularly valuable in complex biological systems where reference spectra may be unavailable or variable [21].
Phasor Transformation Mathematics
For each pixel in the hyperspectral image, the real (G) and imaginary (S) components of the spectral phasor are calculated using the following transformations:
[ G = \frac{\int{\lambda{\text{min}}}^{\lambda{\text{max}}} I(\lambda) \cos \left( 2\pi n \frac{(\lambda - \lambdai)}{\lambda{\text{max}} - \lambda{\text{min}}} \right) d\lambda}{\int{\lambda{\text{min}}}^{\lambda_{\text{max}}} I(\lambda) d\lambda} ]
[ S = \frac{\int{\lambda{\text{min}}}^{\lambda{\text{max}}} I(\lambda) \sin \left( 2\pi n \frac{(\lambda - \lambdai)}{\lambda{\text{max}} - \lambda{\text{min}}} \right) d\lambda}{\int{\lambda{\text{min}}}^{\lambda_{\text{max}}} I(\lambda) d\lambda} ]
where (I(\lambda)) represents the intensity as a function of wavelength, (n) is the harmonic number, and (\lambda_i) is the initial wavelength [22]. In the HyperNIR implementation, these integrals are effectively computed optically through the sine and cosine filtering approach, with normalization provided by the reference image [2].
Linear Combination Property
A key advantage of the phasor approach is the linear combination property, which states that mixtures of spectral components appear along straight lines between the pure components in the phasor plot [22] [21]. This enables:
- Quantitative determination of component ratios without reference spectra
- Identification of unknown spectral species through geometric relationships
- Model-free analysis of complex systems with multiple interacting components
- Resolution of subtle spectral differences between similar biological states
Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for HyperNIR Experiments
| Item | Function | Example Applications |
|---|---|---|
| Liquid Crystal Variable Retarder | Generates wavelength-dependent retardation | Core component of HyperNIR system [2] |
| NIR Linear Polarizers | Filters specific polarization components | Creates spectral filtering with LCVR [2] |
| Environment-Sensitive Dyes (e.g., LAURDAN) | Report on local environmental properties | Membrane order and hydration studies [22] |
| Single-Walled Carbon Nanotubes | NIR fluorescent nanomaterials | Biosensor development and deep-tissue imaging [2] |
| NIR Fluorophores with Narrow Emission | Spectral fingerprinting references | System calibration and validation [2] |
| Standard Reference Materials | Calibration and validation | System performance verification [2] |
Integration in Biomedical Research
The HyperNIR spectral phasor approach enables several advanced applications in biomedical research and drug development. For brain tumour surgery, hyperspectral imaging has demonstrated potential as an intraoperative guidance tool, with one study achieving 70.2% median macro F1-Score for tumour identification using machine learning classification [20]. The phasor method enhances these applications by providing rapid spectral information without the computational overhead of traditional hyperspectral analysis.
In membrane biology research, the combination of environment-sensitive dyes like LAURDAN with spectral phasor analysis has provided insights into membrane order and hydration [22] [24]. The phasor approach surpasses conventional generalized polarization (GP) analysis by utilizing the entire spectrum rather than just two wavelength bands, enabling detection of subtle heterogeneities and intermediate states [22].
The minimal phototoxicity and high imaging speed of phasor-based hyperspectral snapshot microscopy also enables metabolic imaging of live, three-dimensional mouse tissues and tracking of multiple organelles in 3D cultured cells over time [21]. These capabilities make the technology particularly valuable for drug development applications where understanding spatial-temporal dynamics of drug distribution and effect is crucial.
Spectral phasor transformation via the HyperNIR system represents a significant advancement in NIR hyperspectral imaging, addressing the critical limitation of acquisition speed while maintaining high spectral resolution. The direct optical transformation of spectral information into phasor space enables rapid, fit-free analysis of complex biological and materials systems. With applications spanning from biomedical research to environmental monitoring, and its compatibility with standard microscopy platforms, this approach promises to make high-speed hyperspectral imaging accessible to a broad research community. The protocols and guidelines presented here provide researchers with a foundation for implementing this powerful technology in their experimental workflows.
In biomedical research, the drive to observe dynamic processes within living systems using fluorescence microscopy is fundamentally constrained by the photon budget. This concept refers to the finite number of photons that can be collected from a sample before biological integrity is compromised by photobleaching or phototoxicity. This limitation creates an inescapable trade-off between spectral, spatial, and temporal resolution [25] [26]. Hyperspectral imaging (HSI), which captures the full spectrum of light at each pixel, exacerbates this challenge by dividing the photon signal across numerous spectral dimensions [1]. Consequently, a critical need exists for innovative imaging strategies and computational approaches that maximize information extraction from every collected photon. This application note details the underlying principles of these trade-offs and provides validated protocols to guide researchers in optimizing experimental design for hyperspectral biofluorescence characterization, particularly in drug development and live-cell studies.
Quantitative Analysis of Resolution Trade-offs
The following tables summarize the key trade-offs and performance characteristics of different HSI modalities, providing a quantitative foundation for experimental planning.
Table 1: Impact of Resolution Enhancement on Imaging Parameters
| Resolution Type | Spatial Cost | Temporal Cost | Photon Budget Cost | Primary Applications |
|---|---|---|---|---|
| High Spectral | Reduced field of view or spatial sampling | Increased acquisition time per frame | Signal divided across many spectral channels | Spectral unmixing of multiple fluorophores [27] |
| High Spatial | --- | Reduced frame rate or smaller FOV | Signal divided across many pixels | Subcellular localization, fine structure analysis |
| High Temporal | Reduced spatial and/or spectral sampling | --- | Lower signal-to-noise per time point | Live-cell kinetics, rapid signaling events [26] |
Table 2: Comparison of Hyperspectral Imaging Modalities
| Imaging Modality | Spectral Resolution | Temporal Resolution | Photon Efficiency | Key Advantage |
|---|---|---|---|---|
| Emission-Scanning HSI [26] | High (0.5 nm achievable) [28] | Lower (sequential channel capture) | Lower (signal loss through filtering) | High spectral fidelity of emission profiles |
| Excitation-Scanning HSI [29] [26] | High (dependent on light source) | Moderate to High | Higher (>10x signal vs emission-scanning) [26] | Detects all emitted photons; reduced photobleaching |
| Single-Shot HSI (e.g., SHy-Cam) [25] | Moderate | Very High (single exposure) | High (avoids sequential scanning) | Enables full-speed volumetric multiplexing in vivo |
| Full-Spectral FLIM [28] | Very High (512 channels) | Lower (6 s for 256x256 image) | Lower (high-dimensional data) | Simultaneous spectral & lifetime information |
Experimental Protocols for Optimizing the Photon Budget
This protocol is designed for kinetic studies of cell signaling, such as Ca²⁺ flux, where maintaining viability and high temporal resolution is critical [26].
1. Equipment and Reagent Setup
- Microscope Platform: Inverted widefield fluorescence microscope.
- Excitation Light Source: Wavelength-specific LED array illuminator with a Cassegrain-style optical combiner [29].
- Detection: Scientific CMOS or EMCCD camera with high quantum efficiency.
- Cells and Reagents: Human Airway Smooth Muscle Cells (HASMCs); culture media; fluorescent Ca²⁺ indicator dye (e.g., Cal-520 or Fluo-4); laminin-coated glass coverslips [26].
2. Sample Preparation
- Seed HASMCs onto laminin-coated 20 mm glass coverslips and culture for 48 hours to 70-80% confluency in standard conditions (37°C, 5% CO₂).
- Load cells with the cell-permeable Ca²⁺ indicator dye according to manufacturer instructions. Incubate for 30-45 minutes at 37°C, followed by a wash step with fresh media.
- Mount the coverslip in a live-cell imaging chamber on the microscope stage, maintaining physiological temperature and CO₂ throughout the experiment.
3. Data Acquisition
- Spectral Calibration: Acquire reference images of control cells (unlabeled) to establish the autofluorescence spectral signature.
- Excitation Scan: Set the acquisition software to sequentially cycle through the pre-defined LED excitation wavelengths (e.g., 20-30 bands across the visible spectrum). For each wavelength, acquire a single image frame with exposure times between 50-200 ms.
- Time-Lapse Imaging: Repeat the entire excitation scan cycle over the desired time course (e.g., every 10-30 seconds for 30 minutes). To initiate signaling, add the agonist of interest (e.g., histamine) during the time-lapse sequence.
4. Data Processing and Analysis
- Algorithm Selection: Process the hyperspectral data cube using the Matched Filter (MF) or Linear Unmixing (LU) algorithm, which have shown superior performance for quantifying Ca²⁺ signals against autofluorescence [26].
- Pixel Filtering: Apply a signal intensity threshold (e.g., 10x the background noise level) to exclude pixels with signals below the minimum detectable limit, which enhances the accuracy of kinetic traces [26].
- Kinetic Trace Extraction: Generate quantitative traces of Ca²⁺ flux over time by plotting the unmixed signal intensity from regions of interest (ROIs).
Figure 1: Experimental workflow for excitation-scanning HSI of live-cell calcium signaling.
Protocol: Single-Shot Hyperspectral Phasor Analysis for Multiplexed Imaging
This protocol leverages a single-shot hyperspectral phasor camera (SHy-Cam) to rapidly unmix multiple fluorescent labels, ideal for sensitive samples where light exposure must be minimized [25] [27].
1. Equipment and Reagent Setup
- Imaging System: Single-shot hyperspectral phasor camera system (e.g., SHy-Cam) integrated with a widefield or light sheet microscope [25].
- Software: Original MATLAB code for SHy-Cam pre-processing and phasor-based linear unmixing (available from referenced GitHub repository) [25].
- Samples: Biological samples (e.g., zebrafish, fixed tissues) labeled with 3+ fluorophores with overlapping spectra.
2. System Configuration and Calibration
- Ensure the hyperspectral camera is properly calibrated for spectral response according to the manufacturer's specifications.
- In the control software, define the spatial and spectral sampling parameters. The single-shot nature of the system means no sequential scanning is required.
- For phasor analysis, pre-load or acquire reference spectral signatures for the fluorophores used, if available.
3. Data Acquisition
- Single-Exposure Capture: Illuminate the sample with broad-spectrum light suitable for all fluorophores. Acquire the hyperspectral image data in a single camera exposure.
- Volumetric Imaging (Optional): For 3D samples, perform a Z-stack, capturing a single-shot hyperspectral image at each focal plane. The high speed of acquisition enables full-speed volumetric multiplexing [25].
4. Data Processing and Unmixing
- Phasor Transformation: Process the raw hyperspectral cube using the phasor analysis algorithm. This transformation projects the complex spectral data at each pixel into a 2D phasor plot [27].
- Semi-Automated Unmixing: Utilize the hybrid phasor/linear unmixing approach. This method automates the separation of different fluorescent signals without requiring the user to manually interact with the phasor plot, simplifying the workflow [27].
- Component Visualization: Review the unmixed channels to verify correct separation of each fluorophore's signal and generate the final composite image.
Figure 2: Workflow for single-shot hyperspectral phasor imaging and analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Tools for Hyperspectral Fluorescence Imaging
| Item | Function/Description | Example Use Case |
|---|---|---|
| Wavelength-Specific LED Array [29] | Provides rapid, narrow-band excitation light for excitation-scanning HSI. | Live-cell Ca²⁺ signaling studies [26]. |
| Thin-Film Tunable Filter (TFTF) | An alternative for spectral filtering in emission-scanning HSI. | Filter-wheel based HSI of fixed samples [26]. |
| Supercontinuum White Light Laser [28] | A bright, broadband laser source for excitation. | Full-spectrum fluorescence lifetime imaging (FS-FLIM) [28]. |
| Single-Shot Hyperspectral Camera [25] | Captures the entire spectral data cube in a single exposure. | Fast, multi-color fluorescence microscopy in vivo [25]. |
| Phasor Analysis Software [25] [27] | Simplifies and improves the accuracy of spectral unmixing. | Discriminating multiple labels with significant spectral overlap [27]. |
| Linear Unmixing (LU) Algorithm [26] | A standard computational method to separate overlapping fluorescence signals. | Quantitative analysis of excitation-scanning HSI data [26]. |
| Matched Filter (MF) Algorithm [26] | A target detection algorithm that maximizes the signal-to-noise ratio for a known signature. | Detecting weak fluorescent signals against strong autofluorescence [26]. |
From Theory to Practice: Methodological Workflows and Cutting-Edge Biomedical Applications
Hyperspectral imaging (HSI) has emerged as a powerful analytical technique in biomedical research, capable of capturing detailed spatial and spectral information from biological samples. This non-destructive method records a wide spectrum of wavelengths for each pixel in an image, generating complex, high-dimensional datasets often called "hypercubes" [30]. In the specific context of biofluorescence characterization, HSI enables researchers to detect and analyze multiple fluorescent markers or endogenous fluorophores simultaneously, providing unprecedented insight into cellular processes and molecular interactions.
The extraction of meaningful biological information from these complex datasets requires sophisticated chemometric approaches. This application note details practical methodologies for implementing three foundational chemometric techniques—Principal Component Analysis (PCA), Partial Least Squares-Discriminant Analysis (PLS-DA), and Soft Independent Modeling of Class Analogy (SIMCA)—specifically for the automated segmentation of bio-traces in hyperspectral images. When properly validated and applied, these methods transform raw spectral data into actionable biological intelligence for drug discovery and development workflows.
Theoretical Foundations of Key Chemometric Techniques
Principal Component Analysis (PCA)
PCA is an unsupervised dimensionality reduction technique that identifies the principal components (PCs)—orthogonal vectors that capture the maximum variance in the data without using class labels [31]. Informally, the PCA algorithm calculates the first PC along the first eigenvector by minimizing the projection error, then iteratively projects all points to a subspace orthogonal to the last PC and repeats the process [31]. For a data matrix X with n samples and m features, the principal component vectors correspond to the eigenvectors of the covariance matrix. The loading vectors, denoted by L~1~,...,L~n~, are given in terms of the eigenvectors, e~1~,...,e~n~, and the eigenvalues, λ~1~,...,λ~n~, of the covariance matrix C as follows: L~i~ = √λ~i~ e~i~, i = 1, ..., n [31].
Partial Least Squares-Discriminant Analysis (PLS-DA)
PLS-DA is a supervised adaptation of PCA that incorporates class label information to maximize the separation between predefined groups [31] [32]. Whereas PCA maximizes variance, PLS-DA maximizes the covariance between the spectral data (X) and the class assignment vector (y) [31]. The iterative process of PLS-DA computes loading vectors that have the highest covariance with the response, making it particularly effective for classification tasks where the goal is to distinguish between different biological states or tissue types [32]. However, as a supervised method, PLS-DA is prone to overfitting and requires rigorous validation [31] [33].
Soft Independent Modeling of Class Analogy (SIMCA)
SIMCA is a class-modeling technique that builds separate PCA models for each class in the training set. During classification, new samples are projected onto each class model, and their fit is evaluated to determine class membership. This approach is particularly valuable in quality control and authenticity testing, where the goal is to verify whether a sample belongs to a specific class rather than simply assigning it to one of several predefined classes.
Experimental Protocols for Hyperspectral Image Segmentation
Sample Preparation and HSI Acquisition
- Biological Sample Preparation: Plate cells or tissue sections of interest. Apply fluorescent probes or biomarkers relevant to the drug mechanism under investigation. Ensure appropriate controls are included (e.g., untreated controls, isotype controls for immunofluorescence).
- HSI System Setup: Configure the hyperspectral imaging system (e.g., push-broom, spectral scanning) to cover the appropriate excitation and emission ranges for your fluorophores. Implement dark current correction and spectral calibration using standard reference materials.
- Image Acquisition: Capture the hyperspectral datacube. The resulting data structure will be a three-dimensional array (x, y, λ) with two spatial dimensions and one spectral dimension.
Data Pre-processing Workflow
- Spectral Correction: Apply dark current subtraction and flat-field correction to minimize instrumental artifacts.
- Spectral Smoothing: Implement Savitzky-Golay filtering or similar techniques to reduce high-frequency noise while preserving spectral features.
- Normalization: Normalize spectra to correct for variations in signal intensity (e.g., using Standard Normal Variate normalization or vector normalization).
- Data Arrangement: Reshape the hypercube into a two-dimensional matrix where each row represents a pixel (x × y) and each column represents a spectral wavelength (λ).
Chemometric Analysis for Segmentation
Table 1: Performance Comparison of Chemometric Techniques in Hyperspectral Imaging Applications
| Application Area | Technique Used | Reported Performance | Reference |
|---|---|---|---|
| Crop Classification | HSI-TransUNet | 86.05% Accuracy | [30] |
| Disease Detection | PLS-DA-based | 98.09% Accuracy | [30] |
| Colorectal Cancer ID | HSI with Classifier | 86% Sensitivity, 95% Specificity | [30] |
| Skin Cancer | HSI with Classifier | 87% Sensitivity, 88% Specificity | [30] |
| Counterfeit Alcohol | HSI with Classifier | 99.03% F1-score | [30] |
Protocol 1: PCA for Unsupervised Pattern Recognition
- Center the Data: Subtract the mean spectrum from each pixel's spectrum in the data matrix.
- Compute Principal Components: Perform singular value decomposition on the covariance matrix of the mean-centered data.
- Determine Significant Components: Use scree plots or cumulative variance explained to select the number of components (d) that capture the majority of variance (typically >95%).
- Generate Score Images: Project the data onto the selected PCs and reshape the scores back into images to visualize spatial patterns corresponding to each component.
- Interpret Loadings: Analyze the loading vectors to identify which spectral features contribute most to each PC, linking them to potential biological or chemical entities.
Protocol 2: PLS-DA for Supervised Classification
- Define Training Set: Select representative regions of interest (ROIs) from the HSI and assign class labels based on known biological features.
- Model Training: Build a PLS-DA model using the training spectra and their associated class labels. The algorithm finds latent variables that maximize covariance between spectral data and class separation [32].
- Cross-Validation: Implement k-fold cross-validation (typically 5- or 7-fold) to determine the optimal number of latent variables and prevent overfitting [31] [32].
- Permutation Testing: Validate model significance by randomly permuting class labels and comparing the performance of the true model with permutation-based null models [33] [32].
- Whole-Image Prediction: Apply the trained model to all pixels in the HSI to generate a classification map.
- Feature Importance: Calculate Variable Importance in Projection (VIP) scores to identify spectral regions most influential for class discrimination [32].
Protocol 3: SIMCA for Class Modeling
- Build Class Models: For each class of interest, develop a separate PCA model using only training samples from that class.
- Define Acceptance Criteria: Establish critical distance limits for each class model based on the residual variance and score distances of the training samples.
- Classify New Samples: Project each pixel onto all class models and assign it to a class if it falls within the critical distance of that model's space.
- Handle Ambiguity: Pixels may be assigned to multiple classes (overlapping) or no classes (outliers), providing valuable information about classification certainty.
The following workflow diagram illustrates the complete experimental process from sample preparation to segmentation:
Figure 1: Experimental workflow for hyperspectral image segmentation using chemometrics, showing key steps from sample preparation to biological interpretation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagent Solutions for Biofluorescence HSI
| Item | Function in HSI Experiment | Example Applications |
|---|---|---|
| Hyperspectral Imaging System | Captures spatial and spectral data simultaneously; types include push-broom, snapshot, and tunable filter systems. | All HSI applications |
| Fluorescent Probes & Dyes | Target-specific biomarkers that emit characteristic spectra when excited. | Cell labeling, receptor targeting, viability assessment |
| Reference Standards | Materials with known spectral properties for instrument calibration and validation. | Wavelength calibration, intensity normalization |
| Bioinformatics Software | Platforms with implemented chemometric algorithms (PCA, PLS-DA, SIMCA). | Metabolon Platform, mixOmics R package [32] [31] |
| Cell Culture Reagents | Maintain biological samples during imaging experiments. | Live-cell imaging, tissue slice maintenance |
Critical Implementation Considerations
Avoiding Overfitting in Supervised Models
PLS-DA is particularly susceptible to overfitting, especially with high-dimensional data where features far outnumber samples [31] [33]. A permutation test is essential to validate whether the observed classification accuracy is significantly better than chance [33] [32]. In one metabolomics study, while PLS-DA achieved an impressive 81% AUCCH, permutation testing revealed this was not statistically significant (p = 0.057), with the empirical null distribution having a mean of 76.2% AUCCH [33]. Always use cross-validation and permutation tests, and consider alternative methods like Bayesian networks when overfitting is detected [33].
Data Dimensionality and Sample Size
The ratio of samples (n) to features (m) significantly impacts model reliability. Studies show that when features outnumber samples (e.g., ratios of 1:2 to 1:200), PLS-DA can find spurious separations merely by chance [31]. In such high-dimensionality scenarios, consider sparse variants like sPLS-DA that incorporate LASSO penalization to select a subset of relevant features [31].
Validation Strategies
Proper validation requires splitting data into training and test sets, or using cross-validation where data is limited [33]. For hyperspectral image segmentation specifically, care must be taken to avoid training-test data leakage by ensuring pixels from the same spatial region aren't split across training and test sets [34]. Creating appropriate benchmark datasets with proper training-test partitions is essential for fair algorithm validation [34].
Advanced Applications and Future Directions
Deep learning approaches are emerging as powerful alternatives for HSI segmentation, particularly through architectures like convolutional autoencoders (CAEs) that can detect and compress spatio-spectral features in an end-to-end fashion [35]. These approaches are especially valuable when ground truth data is limited, as they can operate in fully unsupervised modes [35].
Future advancements will likely focus on integrating deep learning with traditional chemometrics, developing lightweight portable HSI devices, and improving real-time processing capabilities [30]. These developments will enhance the accessibility and practicality of HSI in both industrial and clinical environments, opening new possibilities for drug discovery and development.
In respiratory physiology and pharmacology, understanding calcium (Ca²⁺) signaling in human airway smooth muscle (ASM) cells is paramount, as the intracellular Ca²⁺ concentration ([Ca²⁺]i) is a primary regulator of bronchial tone, hyperresponsiveness, and remodeling in diseases such as asthma and COPD [36] [37]. Activation of surface receptors by contractile agonists like acetylcholine initiates a dynamic, biphasic elevation of [Ca²⁺]i, characterized by an initial transient peak followed by a sustained plateau [36]. This response results from the coordinated release of Ca²⁺ from intracellular stores, primarily the sarcoplasmic reticulum (SR), and Ca²⁺ influx from the extracellular space. Modern imaging techniques, particularly those leveraging hyperspectral capabilities, now allow researchers to dissect the spatiotemporal organization of these signals with unprecedented detail, capturing propagating calcium waves and oscillations that are fundamental to ASM cell function and dysfunction [36] [38]. This application note details protocols for kinetic studies of these Ca²⁺ dynamics, framed within advanced hyperspectral imaging research.
Calcium Indicators for Live-Cell Imaging
The choice of calcium indicator is critical for successfully capturing kinetic data. The table below compares genetically encoded calcium indicators (GECIs) and small-molecule dyes, the two primary classes of tools for these studies.
Table 1: Comparison of Calcium Indicators for Live-Cell Imaging
| Indicator Type | Example Indicators | Key Advantages | Key Limitations | Best Suited For |
|---|---|---|---|---|
| Genetically Encoded (GECIs) | NEMO, GCaMP6/8, D-Cys | • Targetable to subcellular locations [39]• Long-term expression for chronic studies [39]• Minimal background fluorescence [40] | • Requires transfection/transduction [39]• Generally slower response kinetics [39]• Lower dynamic range than top chemical dyes [39] | Long-term kinetic studies in transfected cells; specific organelle signaling |
| Small-Molecule Dyes | Fura-2, Indo-1, Fluo-4 | • High dynamic range and sensitivity [39]• Fast response kinetics [39]• Easy loading via acetoxymethyl (AM) esters [39] | • Cannot be targeted genetically [39]• Can leak from cells or be extruded [39]• Potential for cellular toxicity | High-speed, high-fidelity kinetic measurements in untransfected primary cells |
NEMO GECIs represent a significant advancement, with a dynamic range over 100-fold greater than older GCaMP variants and a peak signal-to-baseline ratio (SBR) up to 20 times larger, enabling the detection of subtle calcium transients with high resolution [40]. For ratiometric imaging, which corrects for artifacts like variable dye concentration or cell thickness, FRET-based cameleons (e.g., D1-D4cpv series) are excellent choices, as they provide an internal reference signal [39].
Experimental Workflow for Kinetic Calcium Imaging
The following diagram and protocol outline the core workflow for conducting a kinetic calcium imaging experiment in ASM cells.
Diagram 1: Experimental workflow for kinetic calcium imaging.
Protocol: Agonist-Induced Calcium Oscillation Assay
This protocol is designed to capture the characteristic biphasic and oscillatory Ca²⁺ response of ASM cells to contractile agonists like acetylcholine [36].
Materials:
- Cells: Primary human ASM cells (passages 3-7).
- Culture Medium: Smooth Muscle Cell Growth Medium 2, supplemented as per provider's instructions.
- Imaging Buffer: Hanks' Balanced Salt Solution (HBSS) with 20 mM HEPES, pH 7.4.
- Agonist: 1 mM Acetylcholine (ACh) stock solution in dH₂O. Prepare a 10 µM working solution in imaging buffer.
- Calcium Indicator: Choose from Table 1. For example, NEMO plasmid for transfection or Fluo-4 AM dye.
- Equipment: Confocal or hyperspectral microscope with environmental chamber (37°C, 5% CO₂), appropriate laser lines and filters.
Procedure:
- Cell Seeding: Seed ASM cells onto glass-bottom imaging dishes at a density of 50,000 cells/dish and culture for 24-48 hours until ~70% confluent.
- Indicator Introduction:
- For GECIs (e.g., NEMO): Transfect cells with the NEMO plasmid 24-48 hours before imaging using a standard transfection reagent.
- For small-molecule dyes (e.g., Fluo-4 AM): On the day of imaging, incubate cells with 2-5 µM Fluo-4 AM in imaging buffer for 30-45 minutes at 37°C. Replace with fresh imaging buffer and incubate for an additional 20 minutes to allow for complete de-esterification.
- Microscope Setup: Place the dish on the pre-warmed microscope stage. For Fluo-4, set excitation to ~488 nm and collect emission at ~520 nm. For hyperspectral systems like the CHNSPEC FigSpec, configure the spectral range (e.g., 400-1000nm) and resolution (2.5nm) to optimize signal capture [38].
- Image Acquisition:
- Focus on a field of healthy, appropriately transfected or loaded cells.
- Acquire images at a baseline rate of 1-2 frames per second for 60 seconds to establish a stable F₀ (basal fluorescence).
- Without interrupting acquisition, carefully add the 10 µM ACh working solution to the dish to achieve the final desired concentration (e.g., 1 µM). Gently mix.
- Continue acquiring images for at least 10-15 minutes to capture the full kinetic response, including the initial transient, sustained phase, and any oscillations [36].
- Data Processing:
- Use analysis software (e.g., Herschel Vision for hyperspectral data [41]) to extract fluorescence intensity (F) over time (F(t)) for each cell or region of interest (ROI).
- Calculate the change in fluorescence (ΔF) as F(t) - F₀.
- Express the result as ΔF/F₀ (%) to normalize for differences in indicator concentration and cell thickness.
Key Calcium Signaling Pathways in ASM Cells
The calcium dynamics observed in the protocol above are governed by a complex interplay of channels, pumps, and receptors. The following diagram summarizes the primary pathways involved.
Diagram 2: Key calcium signaling pathways in ASM cells.
Pathway Description:
- Initial Release: Agonist binding to G-protein-coupled receptors (GPCRs) triggers phospholipase C activation, generating inositol 1,4,5-trisphosphate (IP₃). IP₃ binds to IP₃ receptors (IP₃R) on the SR, causing an initial rapid release of Ca²⁺ into the cytosol [36].
- Calcium-Induced Calcium Release (CICR): The initial Ca²⁺ rise can activate ryanodine receptors (RyR) on the SR, leading to further Ca²⁺ release in a regenerative process known as CICR [36]. Unitary Ca²⁺ release events through RyRs, called "calcium sparks," can fuse to initiate propagating calcium waves and oscillations [36]. The frequency and amplitude of these oscillations encode information about agonist concentration and are critical for contraction [36].
- Calcium Influx: To replenish SR stores and sustain the response, Ca²⁺ enters the cell from the extracellular space via store-operated calcium entry (SOCE) and receptor-operated channels [36]. Transient receptor potential (TRP) channels are key mediators of this influx.
- Calcium Removal: To restore low basal [Ca²⁺]i, Ca²⁺ is pumped back into the SR by the sarcoplasmic-endoplasmic reticulum calcium ATPase (SERCA) and out of the cell by the plasma membrane Ca²⁺ ATPase (PMCA) [36].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagent Solutions for Calcium Signaling Studies
| Item | Function/Description | Example Use Case |
|---|---|---|
| NEMO GECIs [40] | Genetically encoded Ca²⁺ indicators with very high dynamic range and low basal fluorescence. | Detecting subtle Ca²⁺ transients and single action potentials with high resolution in transfected cells. |
| cADPR [36] | Endogenous second messenger that acts as an agonist for RyR channels, mobilizing Ca²⁺ from the SR. | Investigating the role of the cADPR/RyR pathway in calcium-induced calcium release and oscillation modulation. |
| Thapsigargin [36] | A specific, irreversible inhibitor of the SERCA pump. | Depleting SR Ca²⁺ stores to study store-operated calcium entry (SOCE) mechanisms in isolation. |
| Ryanodine [36] | A plant alkaloid that modulates RyR function (high concentrations lock the channel in a closed state). | Probing the contribution of RyR-mediated CICR to global calcium signals and oscillations. |
| Hyperspectral Imaging System (e.g., CHNSPEC FigSpec) [38] | Camera system capable of capturing a full spectrum per pixel, enabling unmixing of multiple fluorescent signals. | Distinguishing between multiple fluorophores in multiplex assays or resolving autofluorescence from specific Ca²⁺ indicator signals in complex samples. |
| SignalStar Multiplex IHC Kits [42] | Validated antibody panels and fluorescent detection reagents for multiplex immunohistochemistry. | Profiling the expression of multiple signaling proteins (e.g., GPCRs, channels) alongside Ca²⁺ activity in fixed tissue samples. |
The precision of surgical resection is a critical determinant of oncological outcomes. Complete removal of malignant tissue, while preserving healthy structures, directly impacts patient survival and reduces recurrence rates [43]. Intraoperative tissue assessment has traditionally relied on techniques like frozen section analysis, which are subjective, time-consuming, and prone to sampling error [43]. Within the broader context of hyperspectral imaging (HSI) for biofluorescence characterization research, new modalities are emerging to overcome these limitations. Hyperspectral imaging (HSI) is an optical technique that captures spatial and spectral data across hundreds of contiguous wavelengths, generating unique spectral "fingerprints" for different biological tissues [44]. This non-contact, non-ionizing, and contrast-free technology provides real-time, quantitative data on both tissue perfusion parameters, such as oxygenation and hemoglobin concentration, and morphological features indicative of cancer margins, thereby guiding surgical decisions with unprecedented accuracy [44].
Key Quantitative Data on HSI Performance in Oncology
Research demonstrates that HSI, particularly when combined with machine learning (ML), can differentiate between healthy and tumorous tissues with high accuracy. The following tables summarize key quantitative findings from recent studies.
Table 1: Performance Metrics of HSI in Tumor Margin Assessment
| Tumor Type | Key Performance Metrics | Machine Learning Model Used | Reference |
|---|---|---|---|
| Oral Squamous Cell Carcinoma (OSCC) | Accuracy: 0.76, Specificity: 0.89, Sensitivity: 0.48 | Supervised 3D Convolutional Neural Network (CNN) | [43] |
| Renal Tissue (Ischemia Monitoring) | Median AU-ROC: 1.0, Mean AU-ROC: 0.9 | Ensemble of Invertible Neural Networks (INNs) | [44] |
| Renal Perfusion (Porcine Model) | Accuracy: 97.8% in differentiating perfusion states | Machine Learning Algorithms | [44] |
Table 2: Physiological Parameters Quantified by HSI for Perfusion Assessment
| Parameter | Description | Clinical Significance in Oncology |
|---|---|---|
| Tissue Oxygenation (StO₂) | Oxygen saturation level in tissue | Identifies hypoxic regions, a hallmark of aggressive tumors; assesses viability of reconstructed flaps. |
| Oxygenated Hemoglobin (HbO₂) | Concentration of oxygen-carrying hemoglobin | Indicates areas of high metabolic activity and angiogenesis. |
| Deoxygenated Hemoglobin (HbH) | Concentration of deoxygenated hemoglobin | Elevated levels can indicate impaired venous outflow or ischemic tissue. |
| Melanin Concentration | Skin pigment concentration | Used for objective quantification of radiation dermatitis [44]. |
| Water Content | Level of water in tissue | Can be altered in edematous or pathologic tissues. |
Experimental Protocols
Protocol for Ex Vivo HSI of Unstained Tissue Sections for Tumor Margin Detection
This protocol outlines the procedure for acquiring HSI data from fresh-frozen tissue sections to train machine learning models for tumor recognition, as detailed in [43].
I. Sample Preparation
- Tissue Acquisition: Obtain fresh tissue samples directly from the operating room following tumor resection. Snap-freeze samples immediately in liquid nitrogen and store at -80°C until measurement.
- Sectioning: Use a cryotome to cut tissue into sections of 12 μm thickness. Mount sections on standard glass slides. For every 120 μm, allocate one section for HSI measurement to ensure histological correlation.
II. HSI Data Acquisition
- Microscopy System: Use an inverted light microscope (e.g., Axio Scope A1; Carl Zeiss AG) equipped with a 10x objective lens.
- HSI Camera: Integrate an HSI platform (e.g., TIVITA Mini; Diaspective Vision GmbH) with a spectral resolution of 500-1000 nm in 10 nm steps (100 channels).
- Calibration: Before measurement, capture a white reference (blank slide with microscope lamp on) and a dark reference (lamp off) for radiometric calibration.
- Scanning: Perform a systematic meander scan of the entire tissue section using imaging software (e.g., ZEN blue). Acquire corresponding RGB and HSI images at each position. The acquisition time is approximately 5-15 minutes per sample.
III. Histopathological Ground Truth Annotation
- After HSI measurement, stain the tissue sections with standard Hematoxylin and Eosin (H&E).
- Have experienced pathologists manually annotate the H&E-stained slides to delineate tumor regions.
- Co-register the annotated H&E images with the corresponding RGB images and HSI datacubes to create a labeled dataset for machine learning.
IV. Machine Learning and Data Analysis
- Data Preprocessing: Filter HSI datacubes for measurement artifacts and remove samples with no tissue or ambiguous classification.
- Model Training: Train a supervised 3D Convolutional Neural Network (CNN) on the HSI data cubes to perform pixel-wise tumor classification and segmentation. Employ cross-validation strategies (e.g., sixfold) to evaluate model performance.
Protocol for Intraoperative Renal Perfusion Assessment via Laparoscopic HSI
This protocol describes the use of HSI for real-time perfusion monitoring during laparoscopic surgery, such as partial nephrectomy [44].
I. System Setup and Integration
- Employ a lightweight, compact HSI camera capable of video-rate acquisition (e.g., 25 Hz) for real-time assessment.
- Integrate the HSI system into the existing laparoscopic surgical workflow, ensuring the camera is connected to the laparoscope and the display system.
II. Intraoperative Data Acquisition
- Position the laparoscope to capture a clear view of the kidney or tissue of interest.
- Record HSI data before, during, and after vascular clamping to capture the spectrum of perfusion states (physiological, arterial ischemia, venous congestion).
- Ensure consistent illumination and minimize camera movement during capture.
III. Real-Time Data Processing and Analysis
- Use a personalized deep-learning method, such as an ensemble of Invertible Neural Networks (INNs), to treat ischemia detection as an out-of-distribution problem, accounting for high inter-patient variability.
- Generate false-color maps of parameters like StO₂ or a binary classification (perfused/ischemic) that can be overlaid on the surgical view in near-real-time to guide the surgeon.
Workflow and Signaling Pathway Visualizations
HSI for Tumor Margin Assessment Workflow
HSI Data Acquisition and Analysis Logic
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Materials and Reagents for HSI-based Tissue Assessment
| Item | Function/Application | Specifications/Notes |
|---|---|---|
| Cryostat | Preparation of thin, fresh-frozen tissue sections for ex vivo HSI analysis. | Essential for maintaining tissue integrity and biomolecular state. Section thickness typically 10-20 μm. |
| H&E Staining Kit | Gold standard for histopathological evaluation and ground truth annotation. | Used to stain tissue sections after HSI scan for correlative analysis. |
| Liquid Nitrogen | Snap-freezing resected tissue samples to preserve metabolic and morphological state. | Prevents ice crystal formation and degradation, crucial for accurate spectral analysis. |
| Hyperspectral Imaging System | Acquisition of spatial and spectral data from tissue. | Systems can be microscope-integrated or laparoscopic; spectral range should cover visible to near-infrared (e.g., 500-1000 nm). |
| Machine Learning Software Stack | Analysis of complex HSI datacubes for tissue classification and segmentation. | Libraries like TensorFlow or PyTorch for implementing 3D CNNs and other deep learning models. |
| Calibration Standards (White/Dark Reference) | Radiometric calibration of the HSI system to account for illumination and sensor noise. | A white reference (e.g., Spectralon) and a dark reference (lamp off) must be acquired before each measurement session. |
Hyperspectral imaging (HSI) is an advanced optical sensing technique that integrates spectroscopy and digital photography, simultaneously acquiring spatial and spectral data to capture spatially resolved images across numerous contiguous spectral bands [1]. This process generates a three-dimensional data cube, known as a hypercube, where two dimensions represent spatial coordinates (x, y) and the third represents spectral information (λ) [45]. Each pixel in the captured scene contains a unique spectral signature or "fingerprint," enabling non-invasive, label-free analysis of material, chemical, and biological properties based on their interaction with light, including absorption, reflection, and fluorescence [1].
The technique covers a broad optical window, typically from 380 to 2500 nm, encompassing visible light (400-700 nm), near-infrared (NIR), and shortwave infrared (SWIR) regions [1]. The extension into the ultraviolet region (e.g., 225-400 nm) has recently shown promise for characterizing bacterial colonies due to specific absorption and emission peaks from molecular components like amino acids, pigments, and proteins [45]. HSI's capability to capture hundreds of spectral channels at high resolution (5-10 nm) differentiates it fundamentally from conventional imaging, providing rich spectral detail that reveals subtle, diagnostically significant features often invisible to the naked eye or standard cameras [1].
Application Note 1: Subcellular Organelle Imaging
Lipid Subtype Identification via PRM-SRS Microscopy
Background: Mapping the spatial distributions and metabolic dynamics of diverse lipid subtypes in cells and tissues is crucial for understanding their roles in aging and diseases. Conventional methods like mass spectrometry are destructive, while fluorescence labeling can alter native lipid distributions [46]. Stimulated Raman Scattering (SRS) microscopy offers a non-destructive, label-free alternative with subcellular resolution, but distinguishing lipid subtypes with high specificity has remained challenging [46].
Experimental Protocol: Penalized Reference Matching SRS (PRM-SRS)
- Objective: To visualize and identify specific lipid subtypes (e.g., high-density lipoprotein, sphingosine, cardiolipin) within subcellular organelles in human kidney, mouse hippocampus, and human brain tissues [46].
- Sample Preparation: Tissue sections (e.g., human kidney, brain) are prepared using standard cryosectioning methods without chemical fixation or staining to preserve native lipid distributions.
- Instrumentation: A hyperspectral SRS microscopy platform is used. Imaging is typically performed in the Raman CH stretching region (2700–3150 cm⁻¹) across 75 Raman shifts with a spectral distance of 6 cm⁻¹ between images [46].
- Reference Library: A library of spontaneous Raman spectra from 38 known biomolecule standards is acquired and preprocessed for background removal and normalization [46].
- Data Acquisition: Hyperspectral SRS images (e.g., 512 x 512 pixels) are collected from the sample. Each pixel's spectrum undergoes simplex normalization (scaling between 0 and 1) and is divided by its Euclidean norm to focus analysis on spectral shape [46].
- Data Analysis - PRM Algorithm: The core of the protocol involves the Penalized Reference Matching algorithm, which enhances specificity over traditional cosine similarity scoring.
- Each preprocessed pixel spectrum is compared to every preprocessed reference spectrum.
- A similarity score is calculated using the modified formula:
score = (u_i · v - αΔx_i²), whereu_iis the pixel spectrum,vis the reference spectrum,αis a penalty coefficient (optimized at 1×10⁻⁴ cm²), andΔx_iis the positional deviation of spectral peaks [46]. - This penalty term reduces false positives by proportionally decreasing the similarity score when peak positions differ, ensuring accurate identification based on both spectral shape and peak position.
- Output: The algorithm generates images where each pixel is assigned to a specific lipid subtype based on the highest similarity score, revealing subcellular distributions with high chemical specificity. The entire process for a 512x512 hyperspectral image stack takes less than one minute [46].
Key Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Hyperspectral SRS Microscope | Enables label-free chemical imaging with subcellular resolution by detecting intrinsic molecular vibrations. |
| Reference Lipid Library (38 subtypes) | Provides known spectral fingerprints for accurate identification of target lipid molecules via the PRM algorithm. |
| Cryostat | Prepares thin, undamaged tissue sections necessary for high-quality, transparent microscopy. |
| Penalized Reference Matching (PRM) Algorithm | Enhances detection specificity by integrating spectral shape and peak position data, minimizing false positives. |
Quantitative Data Outputs
Table 1: Representative Findings from PRM-SRS Analysis of Tissue Sections
| Tissue / Cell Type | Key Finding | Lipid Subtypes Identified | Spectral Region |
|---|---|---|---|
| Human Kidney | Visualization of high-density lipoprotein particles | HDL | CH Stretching (2700-3150 cm⁻¹) |
| Mouse Hippocampus (Granule Cells) | High cholesterol to phosphatidylethanolamine ratio | Cholesterol, Phosphatidylethanolamine | CH Stretching (2700-3150 cm⁻¹) |
| Human Brain | Subcellular distributions of sphingosine and cardiolipin | Sphingosine, Cardiolipin | CH Stretching (2700-3150 cm⁻¹) |
Application Note 2: Whole Tissue and Bio-Fluid Analysis
Raman HSI for Forensic Bio-Fluid Segmentation
Background: Forensic analysis of biological traces relies on preliminary identification of fluids. Raman HSI offers a non-destructive method to characterize and differentiate stains of biological fluids on various substrates, such as cotton, based on their unique spectral signatures [47].
Experimental Protocol: Raman HSI with Chemometrics
- Objective: To differentiate stains of four distinct biological fluids (blood, urine, sperm, and saliva) on cotton supports [47].
- Sample Preparation: Spots of each bio-fluid are deposited on clean cotton substrates and allowed to dry. No specific chemical pre-treatment is applied.
- Instrumentation: A Raman hyperspectral imager is used. The specific laser wavelength and spectral range are not detailed in the provided results, but standard Raman systems typically use 532 nm, 785 nm, or 1064 nm lasers to avoid fluorescence and cover a fingerprint region (e.g., 500-1800 cm⁻¹) [47].
- Data Acquisition: Hyperspectral images of the stained cotton are collected. Each pixel contains a full Raman spectrum.
- Data Analysis - Chemometrics:
- Soft Independent Modelling of Class Analogy (SIMCA): A classification method that builds a principal component analysis (PCA) model for each class of bio-fluid. Unknown samples are assigned to a class based on their similarity to the class model [47].
- Principal Component Analysis (PCA): Used for dimensionality reduction and to identify the most significant spectral patterns that differentiate the bio-fluids [47].
- Partial Least Squares Discriminant Analysis (PLS-DA): A supervised method that finds a linear relationship between the spectral data (X) and the class membership (Y) to maximize separation between pre-defined groups [47].
- Validation: The model is trained and validated using known samples, and its accuracy is reported [47].
Key Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Raman Hyperspectral Imager | Provides molecular vibrational spectra for every pixel, enabling fingerprinting of bio-fluids. |
| Cotton Supports | A common, complex substrate that mimics real-world forensic evidence conditions. |
| Chemometric Software (SIMCA, PCA, PLS-DA) | Processes high-dimensional spectral data to build predictive models for bio-fluid classification. |
| Reference Bio-fluid Samples (Blood, Urine, Sperm, Saliva) | Creates training and validation datasets for the chemometric models. |
Quantitative Data Outputs
Table 2: Raman HSI for Bio-fluid Identification on Cotton
| Bio-Fluid | Differentiation Capability | Primary Chemometric Tools | Key Outcome |
|---|---|---|---|
| Blood | Successfully differentiated from urine, sperm, saliva | SIMCA, PCA, PLS-DA | Accurate, non-destructive identification for forensic segmentation |
| Urine | Successfully differentiated from blood, sperm, saliva | SIMCA, PCA, PLS-DA | Accurate, non-destructive identification for forensic segmentation |
| Sperm | Successfully differentiated from blood, urine, saliva | SIMCA, PCA, PLS-DA | Accurate, non-destructive identification for forensic segmentation |
| Saliva | Successfully differentiated from blood, urine, sperm | SIMCA, PCA, PLS-DA | Accurate, non-destructive identification for forensic segmentation |
Application Note 3: Environmental Monitoring
UV Hyperspectral Imaging for Bacterial Colony Identification
Background: Traditional plate culturing for bacterial identification is manual, interpretative, and prone to human error. While VIS-NIR HSI has been explored, it can be sensitive to culture medium changes. UV hyperspectral imaging leverages the specific absorption and emission of bacterial components in the ultraviolet range for more robust identification [45].
Experimental Protocol: UV-HSI with PCA-Discriminant Analysis
- Objective: To develop a predictive model for detecting and identifying bacterial colonies from different species on agar plates using UV hyperspectral imaging [45].
- Bacterial Strains and Culture:
- Strains: Escherichia coli, Staphylococcus arlettae, Pseudomonas putida, Shewanella oneidensis [45].
- Media: Cultured on Luria Bertani (LB) or Tryptic Soy (TS) agar plates [45].
- Preparation: Overnight liquid cultures are diluted to ~10⁸ CFU/mL, and 5 µL spots are inoculated onto agar plates. Incubation temperatures are 37°C for E. coli and S. arlettae, and 30°C for P. putida and S. oneidensis [45].
- Instrumentation: A UV hyperspectral imaging system with a back-illuminated CCD camera and a spectrograph, capturing the wavelength range of 225–400 nm. The setup includes a conveyor belt for automated plate transport [45].
- Data Acquisition: Hyperspectral images of the agar plates are acquired after colony formation. The system captures a hypercube for each plate.
- Data Analysis:
- Principal Component Analysis (PCA): The spectral data is processed using PCA to reduce dimensionality and extract the most significant sources of variance (principal components). The first three principal components are often sufficient to capture the major spectral differences [45].
- Discriminant Analysis (DA): A predictive model (e.g., using Quadratic Discriminant Analysis, QDA) is built on the principal components. This model is trained to assign a new spectral signature to one of the bacterial species with a certain probability [45].
- Model Validation: The model is trained and validated using samples of known bacterial species, achieving an accuracy of approximately 90% in differentiating the species [45].
Key Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| UV Hyperspectral Imager (225-400 nm) | Detects unique UV absorption/emission fingerprints of bacterial colonies. |
| Agar Plates (LB, TS Media) | Standard medium for bacterial colony growth, compatible with UV-HSI. |
| Conveyor Belt System | Automates the transport of agar plates for high-throughput analysis. |
| PCA-DA Chemometric Software | Processes UV spectral data to build a predictive model for bacterial ID. |
Quantitative Data Outputs
Table 3: UV-HSI for Bacterial Colony Identification
| Bacterial Species | Relevance / Habitat | Culture Medium | Incubation Temp. | Model Accuracy |
|---|---|---|---|---|
| Escherichia coli | Water quality indicator, pathogens | Luria Bertani (LB) | 37 °C | ~90% (Overall) |
| Staphylococcus arlettae | Nosocomial infections | Luria Bertani (LB) | 37 °C | ~90% (Overall) |
| Pseudomonas putida | Nosocomial infections | Luria Bertani (LB) | 30 °C | ~90% (Overall) |
| Shewanella oneidensis | Opportunistic pathogen, water, food | Tryptic Soy (TS) | 30 °C | ~90% (Overall) |
Broad-Scale Environmental Monitoring
Background: Hyperspectral imaging is pivotal for large-scale environmental monitoring from aerial platforms (satellites, aircraft, drones). Its fine spectral resolution allows detailed assessment of ecosystems, natural resources, and environmental changes [48].
Applications and Protocols:
- Water Quality Monitoring:
- Objective: Assess parameters like chlorophyll content, turbidity, and detect harmful algal blooms and pollutants [48].
- Methodology: Airborne or drone-based HSI systems capture data over water bodies. Spectral signatures of specific water constituents are identified through spectral library matching or inversion models.
- Pollution Detection:
- Objective: Identify and track pollutants in air, water, and soil [48].
- Methodology: Minerals and chemical fluids have distinctive spectra in SWIR, MWIR, and LWIR ranges. HSI can map these signatures to locate contamination invisible to the naked eye.
- Forestry Management:
- Objective: Early detection of forest diseases, insect infestations, and other stressors [48].
- Methodology: Changes in leaf pigment and water content caused by stress alter the spectral reflectance. HSI can detect these subtle changes before they are visually apparent.
Navigating Analytical Challenges: A Guide to Preprocessing, Calibration, and Data Optimization
Hyperspectral imaging (HSI) holds significant promise for biofluorescence characterization in surgical and drug development research, offering enhanced spectral information for precise tissue analysis. However, its clinical adoption is hampered by a critical vulnerability: calibration drift under the dynamic lighting conditions of an operating room. This application note details a novel, neural network-based illumination calibration method that enables spatially resolved, automatic, and sterile calibration. We present comprehensive experimental protocols and validation data demonstrating that this approach successfully disentangles illumination from tissue properties, generalizes across species, and restores the performance of downstream HSI tasks such as physiological parameter estimation and surgical scene segmentation, thereby facilitating reliable biofluorescence research.
Hyperspectral Imaging is a powerful, non-destructive modality that captures a spectrum for each pixel in an image, creating a three-dimensional data cube. This allows for the detailed identification of chemical compositions and physical properties, making it invaluable for biomedical research, including biofluorescence characterization [49] [50]. Despite its potential, the fidelity of HSI data is critically dependent on stable illumination. In surgical environments, lighting conditions are inherently dynamic; surgical lights are adjusted, ceiling lights are dimmed, and daylight intrusion varies. These changes corrupt the spectral data, as the camera sensor integrates both the desired tissue reflectance/fluorescence and the varying ambient light.
Traditional calibration requires a physical "white reference" measurement—a snapshot of a reference tile under the current lighting—to be performed whenever lights change [51] [52]. This process is tedious, disrupts surgical workflow, and raises sterility concerns. The consequence is calibration drift, where the accuracy of spectral data degrades, compromising subsequent analyses like fluorescence quantification and tissue segmentation. This application note outlines a learning-based solution to conquer this drift, enabling robust HSI integration in dynamic environments.
Core Methodology: Neural Illumination Calibration
The proposed neural calibration method reframes the problem: instead of manually acquiring a white reference, the corresponding reference image is predicted directly from an uncalibrated hyperspectral input.
Key Innovation: Disentanglement and Synthetic Training
The core novelty lies in a two-dataset training paradigm that conceptually disentangles the space of possible illuminations from the space of possible tissue configurations [52].
- Illumination Dataset: A collection of real-world white reference images captured under diverse OR lighting conditions (e.g., varying surgical light angles, intensities, and ceiling light states) is combined with physics-inspired simulated illuminations. This creates a comprehensive and representative set of possible lighting scenarios.
- Sample Dataset: A separate set of accurately calibrated HSI images of relevant biological samples (e.g., tissues).
During training, a calibrated sample from the sample dataset is synthetically corrupted by element-wise multiplication with a white reference image from the illumination dataset, simulating the effect of stray light. The neural network is then trained to reconstruct the original illuminating white reference from this corrupted input [52].
Neural Network Architecture and Workflow
The following diagram illustrates the complete workflow, from data preparation through to calibrated output.
Experimental Validation and Performance Metrics
The method was rigorously validated on a total of 1,890 HSI cubes from phantoms, porcine subjects, rats, and humans [51] [52]. Evaluation was conducted using both simulated and real stray light scenarios, assessing performance on downstream tasks like semantic segmentation and physiological parameter estimation.
Quantitative Performance Data
The table below summarizes the key quantitative findings from the validation studies, comparing the proposed method against traditional and previously proposed calibration methods.
Table 1: Quantitative Performance of Neural Illumination Calibration on Downstream Tasks
| Test Dataset | Metric | No Recalibration (Stray Light) | Physical White Reference (Gold Standard) | Previous Calibration Methods | Proposed Neural Method |
|---|---|---|---|---|---|
| Porcine (in-domain) | Segmentation Accuracy (Dice Score) | Dramatically reduced [52] | Restored to optimal performance [52] | Performance degraded [52] | Matches gold standard, outperforms previous methods by a large margin [51] [52] |
| Human (out-of-domain) | Physiological Parameter Estimation Error | Significant error [51] | Minimal error (baseline) [51] | Not sufficient to restore performance [52] | Robust generalization, restores reliable parameter estimation [51] [52] |
| Rat & Phantom | Calibration Accuracy (vs. ground truth) | N/A | N/A | Poor performance in OR-like conditions [52] | Accurate and reliable across species and camera systems [51] |
The Necessity of Spatially Resolved Calibration
A critical finding supporting the design of this method was that the assumption of spatially uniform illumination is invalid in the OR [52]. Surgical lights create complex, non-uniform light fields. The proposed neural approach, by predicting a full white reference image, provides a spatially resolved calibration that corrects for these local variations, a significant advantage over methods that only estimate a single, global illuminant.
Application Notes & Detailed Experimental Protocols
Protocol 1: Implementing Neural Calibration for Biofluorescence Research
This protocol describes the steps to integrate the neural illumination calibration module into an existing HSI data acquisition pipeline for biofluorescence studies.
Purpose: To enable automatic, sterile, and accurate calibration of HSI data during experiments with dynamic lighting. Primary Applications: Intra-operative biofluorescence characterization, real-time tissue viability assessment, and long-term fluorescence imaging studies under variable illumination.
Workflow:
System Setup:
- Mount the HSI camera securely, ensuring a clear field of view of the target area.
- The system should be pre-equipped with the trained neural network model (e.g., on a connected GPU-accelerated workstation).
Initialization:
- Perform a one-time, traditional physical white reference calibration under a defined, neutral light condition to establish a baseline. This may also be used for initial network training data.
Data Acquisition & Real-Time Calibration:
- Acquire an uncalibrated HSI cube (
I_raw) of the target tissue or fluorescence sample. - Input
I_rawinto the pre-trained neural network model. - The network outputs the predicted white reference image (
I_white_pred). - Perform element-wise division to generate the calibrated image:
I_calibrated = I_raw / I_white_pred. - The calibrated HSI cube is now ready for downstream analysis (e.g., spectral unmixing, fluorescence quantification).
- Acquire an uncalibrated HSI cube (
Continuous Operation:
- Repeat Step 3 for every HSI acquisition. The model automatically adapts to any changes in lighting between captures, preventing calibration drift.
Protocol 2: Generating a Validation Dataset
This protocol is for researchers who need to validate the neural calibration method on their own HSI systems or under specific lighting conditions.
Purpose: To create a paired dataset of uncalibrated and ground-truth calibrated HSI images for quantifying calibration performance.
Procedure:
Preparation:
- Place a calibration target (e.g., a color checker board with known reflectance properties or a fluorescence standard) within the imaging field.
- Set up the lighting to a "reference state" (e.g., only the HSI system's internal lights).
Ground Truth Acquisition:
- Acquire a hyperspectral image of the target. This serves as the ground truth calibrated image (
I_gt).
- Acquire a hyperspectral image of the target. This serves as the ground truth calibrated image (
Stray Light Introduction:
- Introduce a dynamic light source (e.g., a surgical LED light) at a specific angle and intensity.
- Without moving the target or the HSI camera, acquire a new hyperspectral image. This is the uncalibrated image under stray light (
I_raw).
White Reference Acquisition:
- Replace the target with a sterile white reference tile (or use an integrated reference if available) at the exact same position and under the exact same stray light conditions.
- Acquire a hyperspectral image of the white tile. This is the ground truth white reference (
I_white_gt) for this specific stray light scenario.
Data Pairing and Replication:
- The triple (
I_raw,I_white_gt,I_gt) forms one complete data point. - Repeat steps 2-4 for multiple stray light configurations (varying angles, distances, and intensities of external lights) and for different target samples.
- The dataset can be used to benchmark the neural network's prediction accuracy by comparing
I_white_predtoI_white_gtand the finalI_calibratedtoI_gt.
- The triple (
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Equipment for Implementing Neural HSI Calibration
| Item | Function / Application | Specifications / Notes |
|---|---|---|
| Hyperspectral Imaging Camera | Core data acquisition device. | Systems like Tivita Tissue (halogen) or Tivita 2.0 Surgery (LED); spectral range suitable for biofluorescence (e.g., visible to near-infrared) [52]. |
| Sterile White Reference Standard | For acquiring ground truth white references and initial system characterization. | A sterile, spectrally flat reflector with high reflectance (>99%) across the camera's spectral range. Addresses sterility concerns in the OR [52]. |
| Spectralon Targets | For laboratory validation and system calibration. | Certified reflectance standards (e.g., color checker boards) for quantitative accuracy assessment [52]. |
| Dynamic Stray Light Source | For simulating realistic OR lighting conditions during validation. | Adjustable LED surgical light (e.g., Dr. Mach LED surgical light) [52]. |
| GPU-Accelerated Workstation | For running the neural network inference in real-time. | Requires compatible hardware (e.g., NVIDIA GPU) and software framework (e.g., PyTorch, TensorFlow). |
| Biofluorescence Phantoms | For controlled validation of fluorescence quantification post-calibration. | Tissue-simulating phantoms with embedded fluorophores of known concentration. |
The neural illumination calibration method presented herein provides a robust, automated solution to the longstanding problem of calibration drift in dynamic surgical environments. By leveraging a disentangled learning approach and spatially resolved prediction, it ensures the reliability of HSI data, which is foundational for advanced biofluorescence characterization research. This technology paves the way for the seamless and widespread adoption of HSI in clinical and pharmaceutical settings, enhancing the precision of surgical guidance and quantitative biosensing.
Hyperspectral imaging (HSI) has emerged as a cornerstone technology for biofluorescence characterization, enabling the non-invasive quantification of molecular interactions and biochemical processes critical to drug development. This technique acquires three-dimensional datacubes, where each pixel contains a continuous spectrum, thereby encoding both spatial and chemical information. The analytical power of HSI, however, is contingent upon robust preprocessing pipelines that mitigate spectral artifacts and enhance biologically relevant signals. For research scientists quantifying biofluorescence signatures, the selection and sequencing of preprocessing strategies—specifically spectrum scaling, noise smoothing, and artifact filtering—directly influence the accuracy, reproducibility, and sensitivity of downstream analyses. This document provides detailed application notes and protocols for optimizing these preprocessing components, framed within the context of a thesis on hyperspectral biofluorescence characterization. The guidelines are designed to equip researchers and drug development professionals with methodologies to ensure data integrity, improve model generalizability, and maximize the detection of subtle spectral features indicative of therapeutic effects.
Comparative Analysis of Preprocessing Techniques
The efficacy of a hyperspectral preprocessing pipeline is determined by the synergistic performance of its constituent techniques. The table below summarizes the core functions, common algorithms, and performance considerations for scaling, smoothing, and filtering, based on empirical evaluations from recent studies.
Table 1: Comparative Analysis of Core Preprocessing Techniques
| Technique | Core Function | Common Algorithms | Performance & Key Considerations |
|---|---|---|---|
| Scaling | Adjusts spectral intensity to a common scale, enhancing convergence and reducing patient-specific bias [4]. | Standardization (Z-score), Normalization (e.g., Min-Max, SNV) [4] [53]. | Standardization often outperforms normalization for biological classification [4]. SNV and Min-Max are highly effective at reducing glare and height variation artifacts [53]. |
| Smoothing | Reduces high-frequency noise across spatial or spectral dimensions. | Median Filter, Gaussian Filter, Savitzky-Golay Filter [4]. | Performance is application-dependent. Can degrade performance by oversmoothing informative features; use with caution [4] [54]. Savitzky-Golay can preserve spectral shape better than median filters [4]. |
| Filtering | Removes pixels with artifacts that confound analysis (e.g., blood, glare). | Threshold-based masking, spectral angle mapper. | Blood filtering is critical when its strong absorption spectrum mimics or obscures target signals (e.g., cancerous tissues) [4]. Glare filtering addresses wavelength-independent offsets [53]. |
The following workflow diagram illustrates the logical sequence for integrating these techniques into a coherent preprocessing pipeline for hyperspectral biofluorescence data.
Workflow: Hyperspectral Preprocessing Pipeline
Detailed Experimental Protocols
Protocol 1: Scaling for Spectral Uniformity
Objective: To transform spectral data into a consistent scale, mitigating variations from instrumentation and sample geometry, thereby improving the performance of subsequent machine learning models [53] [55].
Materials:
- Raw hyperspectral datacube (Dimensions:
X × Y × λ) - Computing environment (e.g., Python with NumPy, SciPy)
Procedure:
- Data Extraction: Extract all spectral vectors
R(x, y)from the datacube. - Algorithm Selection & Application:
- Standard Normal Variate (SNV):
- For each individual spectrum
R, calculate its mean (μ) and standard deviation (σ). - Apply the transformation:
R_SNV = (R - μ) / σ[53].
- For each individual spectrum
- Min-Max Normalization:
- Global Standardization (Z-score):
- For each wavelength band
λ_iacross the entire dataset, calculate the global mean (μ_λi) and standard deviation (σ_λi). - Apply the transformation to each pixel:
R_std(λ_i) = (R(λ_i) - μ_λi) / σ_λi[4].
- For each wavelength band
- Standard Normal Variate (SNV):
- Validation: Visually inspect the scaled spectra to ensure preservation of spectral shape (e.g., peak-trough relationships). Compare the distribution of a subset of spectra before and after scaling.
Application Note: SNV and Min-Max are pixel-based operations and are highly effective for correcting light-scattering effects and path-length differences. Global Standardization is feature-based and can help correct for sensor drift across a large experiment but may be less effective for single-image analysis [4] [53].
Protocol 2: Noise Reduction via Spectral Smoothing
Objective: To attenuate high-frequency noise in spectral signals while preserving the underlying biochemical signatures, enhancing the signal-to-noise ratio for more robust feature extraction [4] [54].
Materials:
- Scaled hyperspectral datacube
- Computing environment (e.g., Python with SciPy.signal)
Procedure:
- Parameter Initialization:
- Savitzky-Golay Filter (1D Spectral): Set the window length (e.g., 9 points) and polynomial order (e.g., 2nd order) [4].
- Median Filter (2D Spatial): Define a kernel size (e.g., 3×3 or 5×5) for spatial smoothing on each wavelength band.
- Application:
- 1D Spectral Smoothing: Apply the Savitzky-Golay filter independently to every spectral vector
R(x, y)along the wavelength axis. - 2D Spatial Smoothing: Apply the median filter to each individual wavelength band
λ_iacross the spatial (X, Y) dimensions.
- 1D Spectral Smoothing: Apply the Savitzky-Golay filter independently to every spectral vector
- Validation:
- Plot representative raw and smoothed spectra to visually confirm noise reduction without significant distortion of key spectral features (e.g., fluorescence peaks).
- Quantitatively evaluate the impact by comparing the signal-to-noise ratio or the performance of a downstream task (e.g., classification accuracy) on a small, held-out validation set with and without smoothing.
Application Note: Smoothing is not universally beneficial. Overly aggressive smoothing can erase subtle but biologically meaningful spectral features. It is crucial to optimize smoothing parameters on a representative subset of data prior to full dataset processing [4] [54].
Protocol 3: Filtering of Biological and Optical Artifacts
Objective: To identify and mask non-informative or confounding pixels, such as those containing blood or specular reflections, to prevent misclassification and improve model specificity [4] [53].
Materials:
- Smoothed hyperspectral datacube
- Reference spectral libraries (if available) for blood and other artifacts.
Procedure:
- Blood Pixel Identification:
- Method: Spectral Angle Mapper (SAM).
- Action: Calculate the spectral angle between each pixel's spectrum and a reference blood spectrum. Pixels with an angle below a defined threshold are flagged as blood and masked [4].
- Glare/Reflection Pixel Identification:
- Method: Intensity Thresholding.
- Action: Calculate the mean intensity across all or a subset of wavelengths for each pixel. Pixels with an intensity value above a statistically defined threshold (e.g., mean + 3 standard deviations of the image intensity) are identified as glare and masked [53].
- Mask Application: Create a binary mask of valid pixels and apply it to the datacube. Subsequent analysis (e.g., patch extraction) will only consider these valid pixels.
Application Note: The threshold for glare should be determined empirically from the data. For blood detection, the accuracy is highly dependent on the quality of the reference spectrum. Generating a reference from a small region of interest (ROI) confirmed to contain blood within your own images is often more reliable than using a generic library spectrum [4].
The Scientist's Toolkit
The following table details essential reagents, materials, and software solutions for implementing the hyperspectral biofluorescence preprocessing pipelines described in this document.
Table 2: Key Research Reagent Solutions for HSI Preprocessing
| Item Name | Vendor Examples | Function in Preprocessing Pipeline |
|---|---|---|
| Tungsten Halogen Light Source | Thorlabs, Labsphere | Provides stable, broad-spectrum illumination from visible to near-infrared, essential for consistent reflectance and fluorescence data capture [56]. |
| NIST-Traceable Reflectance Targets | Labsphere (e.g., Spectralon) | Serves as a white reference for calibrating raw digital numbers to absolute reflectance, a critical first step in quantitative analysis [55]. |
| Pushbroom Hyperspectral Camera | Specim, Headwall Photonics, Diaspective Vision | Captures high-resolution spatial and spectral data; the pushbroom design (line-scanning) is common for benchtop and medical imaging systems [4] [56]. |
| Python with SciPy/Scikit-learn | Anaconda, PyPI | Provides open-source libraries for implementing scaling (StandardScaler, MinMaxScaler), smoothing (savgol_filter, medfilt), and other preprocessing operations [4]. |
| ENVI/IDL Software | L3Harris Geospatial | Commercial software platform offering a comprehensive graphical environment for hyperspectral data visualization, ROI selection, and preprocessing [56]. |
Autofluorescence, the inherent background emission from biological tissues and materials, presents a significant challenge in fluorescence microscopy and bioimaging. This unwanted signal can obscure the specific emission from fluorescent labels (e.g., antibodies, fluorescent proteins, RNA probes), reducing the signal-to-noise ratio, compromising quantitative accuracy, and limiting the ability to multiplex several fluorescent markers [57] [58]. Hyperspectral imaging (HSI) captures the complete emission spectrum at every pixel in an image, and spectral unmixing is a powerful computational technique that decomposes this mixed signal into its constituent components [59] [58]. When applied to biological samples, this process allows researchers to isolate and subtract the autofluorescence spectrum, thereby revealing a clear, quantitative signal from the fluorophore-of-interest [57] [60]. This application note details the underlying principles and provides a robust protocol for implementing linear unmixing to mitigate autofluorescence in complex samples, such as plant and brain tissues, within the broader context of hyperspectral imaging for biofluorescence characterization research.
Theoretical Foundation: The Linear Mixing Model
Spectral unmixing in fluorescence imaging is predominantly based on a linear mixture model (LMM). This model operates on the principle that the total hyperspectral signal measured at any given pixel is a linear combination of the pure spectral signatures of all fluorescent entities within that pixel, weighted by their respective abundances [61] [58]. The model is mathematically represented as:
$$ I(x, y, \lambda) = \sum{i=1}^{n} Ci(x, y) \cdot S_i(\lambda) + \epsilon $$
Where:
- ( I(x, y, \lambda) ) is the measured intensity at pixel (x, y) and wavelength ( \lambda ).
- ( C_i(x, y) ) is the concentration (abundance) of the i-th fluorescent component at pixel (x, y).
- ( S_i(\lambda) ) is the reference emission spectrum (endmember) of the i-th fluorescent component.
- ( n ) is the total number of fluorescent components (including autofluorescence and all labels).
- ( \epsilon ) represents additive noise.
The power of this approach lies in its ability to computationally dissect the overlapping signals. If the reference spectra (( Si(\lambda) )) of the autofluorescence and the target fluorophores are known or can be accurately estimated, solving the inverse of this linear system allows for the calculation of the concentration map ( Ci(x, y) ) for each component, effectively isolating them from one another [57] [58].
Key Spectral Unmixing Algorithms and Their Applications
Several algorithms can be employed to solve the LMM. The choice of algorithm often depends on prior knowledge of the sample's spectral signatures.
Table 1: Comparison of Primary Spectral Unmixing Algorithms
| Algorithm | Principle | Prior Knowledge Required? | Advantages | Ideal Use Cases |
|---|---|---|---|---|
| MCR-ALS [61] [62] | Iteratively alternates between calculating concentration profiles and spectral profiles to achieve a least-squares solution. | No (can be applied without) | Highly flexible; allows application of constraints (e.g., non-negativity); suitable for complex image fusion. | Analyzing data from multiple HSI platforms; systems where reference spectra are difficult to obtain. |
| Linear Unmixing with Reference Spectra [57] [59] | Uses known reference spectra (endmembers) to solve the linear equations for abundance maps. | Yes (reference spectra) | Computationally efficient; simple to implement; provides direct quantification. | Standard multiplexed fluorescence imaging; when pure spectra of labels and autofluorescence can be acquired. |
| Vertex Component Analysis (VCA) [58] | Automatically extracts the purest spectral signatures (endmembers) directly from the hyperspectral data cube. | No | Fully automated; removes user bias in selecting reference pixels. | Complex specimens like human brain tissue with abundant lipofuscin; high-throughput analysis. |
| Principal Component Analysis (PCA) [60] | Reduces data dimensionality by transforming it to a new set of orthogonal axes (principal components) that capture the greatest variance. | No | Powerful for identifying major patterns of variation and separating tissues based on autofluorescence. | Label-free tissue characterization; initial exploratory analysis of multispectral autofluorescence data. |
Experimental Protocol: Linear Unmixing for Autofluorescence Subtraction
This protocol outlines the steps for acquiring hyperspectral data and performing linear unmixing to isolate a target fluorescent signal from tissue autofluorescence, using post-mortem brain tissue with lipofuscin as a representative example [58].
Materials and Equipment
Table 2: Essential Research Reagents and Equipment
| Item | Function/Description | Example |
|---|---|---|
| Hyperspectral Microscope | Instrument for acquiring spatial and spectral data. | Confocal microscope with spectral detector (e.g., Zeiss LSM 780) [58]. |
| Spectral Unmixing Software | Software to perform linear unmixing calculations. | ZEN Black, SUFI, or open-source tools in FIJI/ImageJ [58]. |
| Tissue Sections | The biological sample under investigation. | Fixed, frozen, or paraffin-embedded sections (e.g., mouse or human brain tissue). |
| Target-Specific Fluorophores | Probes to label the molecule/structure of interest. | Alexa Fluor dyes, Cy dyes, or Opal dyes for immunofluorescence or smFISH [58]. |
| Mounting Medium | To preserve the sample for microscopy. | Antifade mounting medium. |
Step-by-Step Procedure
Sample Preparation and Labeling:
- Prepare your tissue sections according to standard protocols for your application (e.g., immunofluorescence, smFISH) [58].
- Include the necessary controls: a single-stained control for each fluorophore used and an unstained control (or a tissue region with no specific labeling) to characterize the autofluorescence spectrum.
Hyperspectral Image Acquisition:
- Place your multiplexed stained sample on the microscope stage.
- Define Acquisition Parameters: Set the excitation wavelength and configure the spectral detector to collect emission across a continuous range of wavelengths that covers the emission profiles of all your fluorophores and the autofluorescence. For instance, collect emission from 420 nm to 720 nm in 5-10 nm increments [60].
- Acquire Image Stacks: Capture a hyperspectral data cube (x, y, λ) for your sample and for all the single-stained and unstained controls under identical instrument settings (laser power, detector gain, exposure time) [59].
Spectral Library Generation:
- For each single-stained control, manually select several regions of interest (ROIs) that are brightly and specifically labeled. Average the spectra from these ROIs to generate a pure reference spectrum for each fluorophore.
- For the autofluorescence spectrum, manually select ROIs from the unstained control or from areas in your multiplexed image that are known to be autofluorescent but lack specific labeling (e.g., lipofuscin granules in brain tissue). Average these spectra to create the autofluorescence reference signature [58].
Linear Unmixing Computation:
- Input the hyperspectral data cube from your multiplexed sample into the unmixing software.
- Load the reference spectral library (all fluorophores + autofluorescence).
- Run the linear unmixing algorithm. The algorithm will solve the LMM for every pixel, calculating the relative contribution (abundance) of each reference spectrum.
- Apply Constraints: Ensure that non-negativity constraints are applied to both concentrations and spectra, as negative values are not physically meaningful [61] [62].
Output and Analysis:
- The algorithm will output a set of concentration maps (images), one for each component in the spectral library.
- The concentration map for your target fluorophore will represent the isolated specific signal, with the autofluorescence signal effectively subtracted.
- These unmixed images can then be used for downstream quantitative analysis, such as measuring fluorescence intensity or co-localization.
Workflow Visualization
Critical Considerations for Effective Unmixing
- Spectral Distinguishability: The success of linear unmixing is contingent on the reference spectra not being perfectly correlated. Even heavily overlapping spectra can be separated if there are subtle but consistent differences in their spectral shape [59].
- Addressing the "Black Box": To enhance reproducibility and transparency, especially when using proprietary software, it is good practice to report the source of your reference spectra and the specific unmixing algorithm used [58].
- Advanced Automation: For high-throughput studies or to eliminate user bias in selecting reference pixels, automated endmember extraction algorithms like Vertex Component Analysis (VCA) can be integrated into the workflow [58].
Spectral unmixing is an indispensable tool for modern biofluorescence characterization, transforming challenging imaging experiments by enabling clear isolation of target signals from confounding autofluorescence. By following the detailed protocol and considerations outlined in this application note, researchers and drug development professionals can robustly apply this technique to enhance the sensitivity, specificity, and multiplexing capability of their hyperspectral imaging workflows, thereby extracting more reliable and quantitative biological data.
In hyperspectral imaging (HSI) for biofluorescence characterization, the accurate quantification of fluorophore concentration is often the primary research objective. However, the measured fluorescence signal is intrinsically convolved with the absorption and scattering properties of the tissue itself. These effects, caused by the heterogeneous distribution of components like hemoglobin, water, and lipids, can dramatically alter the path of both excitation and emission light, leading to significant errors in quantification [63] [64]. For instance, in the context of 5-aminolevulinic acid (5-ALA)-induced protoporphyrin IX (PpIX) detection in glioma, the local microenvironment—including factors like pH and tissue consistency—directly influences the fluorescence emission, complicating the direct correlation between signal intensity and actual fluorophore concentration [63]. Algorithms that correct for these effects are therefore not merely optional post-processing steps but are essential for transforming qualitative HSI into a quantitative, reliable tool for scientific and clinical decision-making [65] [64]. This document outlines the core algorithmic approaches and provides detailed protocols for their implementation in biofluorescence research.
Algorithmic Approaches for Correction
A range of algorithms, from classical to AI-driven, have been developed to disentangle the effects of tissue optics from the desired fluorophore signal. The choice of algorithm depends on the availability of a priori knowledge of the optical properties and the required accuracy.
Table 1: Key Algorithms for Correcting Tissue Optical Effects in HSI
| Algorithm Name | Underlying Principle | Key Inputs Required | Primary Advantages | Quantified Performance |
|---|---|---|---|---|
| Classical Spectral Unmixing [57] | Linear mixture modeling to separate signal contributions | Basis spectra of target fluorophore and autofluorescence | Conceptually simple; effective when basis spectra are accurate | Improved tumor contrast; enabled detection of faint features [57] |
| Semi-Supervised Deep Learning [64] | Deep neural network trained with limited labeled data and larger unlabeled datasets | Labeled data (e.g., known PpIX concentrations); unlabeled hyperspectral data | Reduces need for extensive labeled data; improves generalization | Pearson R: 0.91 (pig brain); 36% lower false-positive rate (human data) [64] |
| Supervised Deep Learning [64] | Deep neural network trained entirely on labeled data | Large dataset with known ground-truth fluorophore concentrations | High performance when sufficient, high-quality labels are available | Pearson R: 0.997 (phantom), 0.990 (pig brain) [64] |
The following diagram illustrates the logical relationship and workflow between these different algorithmic approaches based on the available data.
Experimental Protocol for Validation
To validate any correction algorithm, a robust experimental protocol comparing HSI-derived measurements against a gold standard is essential. The following protocol, adapted from a recent study using LC-MS for validation, provides a detailed workflow [63].
Protocol: Validating PpIX Quantification with LC-MS
Objective: To assess the accuracy of hyperspectral imaging quantification of protoporphyrin IX (PpIX) in tissue by comparison with reversed-phase liquid chromatography coupled to mass spectrometry (LC-MS).
Hypothesis: The HSI-based quantification of PpIX concentration, after application of a correction algorithm, will show a strong correlation with the concentrations measured by LC-MS.
Table 2: Research Reagent Solutions for HSI-LC-MS Validation
| Item Name | Function/Description | Supplier Example |
|---|---|---|
| Protoporphyrin IX (PpIX) | Target fluorophore for quantification | Enzo Life Sciences GmbH |
| Mesoporphyrin (MpIX) | Internal standard for LC-MS analysis | Merck KGaA |
| Dimethyl Sulfoxide (DMSO) | Solvent for preparing porphyrin stock solutions | Merck KGaA |
| Pig Brain Homogenate | Surrogate matrix to mimic tissue optical properties | Local butcher |
| Acousto-Optic (AOTF) or Liquid Crystal Tunable Filter (LCTF) | Wavelength selection for HSI system | Meadowlark Optics Inc. |
| sCMOS Camera | High-sensitivity detector for fluorescence | PCO |
| Hyperspectral Imaging Algorithm | Software for spectral unmixing and correction | MATLAB (The MathWorks Inc.) |
Pre-experiment Preparation:
- Solution Preparation: Dissolve PpIX and MpIX in DMSO to create 300 pmol/µl stock solutions. Store at -20°C protected from light.
- Surrogate Tissue Preparation: Homogenize fresh pig brain using a blender. Aliquot 250 mg for LC-MS and 600 mg for HSI.
Procedure:
- Sample Spiking:
- For LC-MS calibration: Spike 250 mg aliquots of pig brain homogenate with PpIX stock to create a concentration series (e.g., 0.002, 0.01, 0.04, 1.0, 2.5, 3.0 pmol/mg). Perform in triplicate.
- For HSI calibration: Similarly, spike 600 mg aliquots across a wider concentration range (e.g., 0 to 50.0 pmol/mg). Shake at room temperature for 30 minutes to allow for porphyrin incorporation.
- LC-MS Analysis:
- Extract porphyrins from the spiked 250 mg samples using a validated method (e.g., involving protein precipitation and centrifugation).
- Inject the extract into the LC–MS system. Use the internal standard (MpIX) for quantification.
- Calculate the absolute PpIX concentration in each sample (in pmol/mg) based on the calibration curve. Record recovery rates (typically 80% for PpIX) [63].
- Hyperspectral Imaging:
- Acquire HSI data of the spiked 600 mg samples using a wide-field HSI system [63].
- Imaging Setup: Use a 405 nm LED for excitation. Employ an LCTF or AOTF to capture images from 420 nm to 730 nm in fine increments (e.g., 3-5 nm). Include a dark measurement (light off) and a broadband white light measurement.
- Data Preprocessing: Perform dark subtraction and exposure time correction on the raw spectral images.
- Apply Correction Algorithm: Process the hyperspectral data using the chosen algorithm (e.g., spectral unmixing or a deep learning model) to compute the PpIX contribution, typically in units of µg/ml (HIPpIX).
- Data Correlation and Analysis:
- Convert HSI-derived HIPpIX values to pmol/mg (HICalc-PpIX) using the calibration curve from the spiked pig brain samples.
- For the human biopsy samples (e.g., 27 biopsies from glioma patients), process both with LC-MS and HSI as described above.
- Perform a linear regression or correlation analysis (e.g., Pearson correlation) between the LC-MS-derived PpIX concentrations (ground truth) and the HICalc-PpIX values for both the surrogate tissue and human biopsies.
The following workflow diagram summarizes the key steps in this validation protocol.
The transition of hyperspectral imaging from a qualitative visualization tool to a quantitative analytical platform in biofluorescence research hinges on the effective correction of tissue absorption and scattering. As demonstrated, algorithms ranging from classical spectral unmixing to advanced semi-supervised deep learning models can significantly improve quantification accuracy. The provided experimental protocol offers a framework for rigorously validating these algorithms against gold-standard methods like LC-MS. By adopting these sophisticated correction techniques, researchers in drug development and biomedical science can obtain more reliable and interpretable data on fluorophore biodistribution and concentration, ultimately enhancing the utility of HSI in critical applications such as tumor margin detection and therapeutic agent tracking.
In hyperspectral imaging (HSI) for biofluorescence characterization, data integrity is paramount. The high-dimensional nature of HSI data, which combines spatial and spectral information across numerous contiguous bands, makes it particularly susceptible to specific artifacts and data quality issues [1]. These challenges—namely class imbalance in biological samples, contaminating reflections, and the presence of blood and noisy pixels—can significantly compromise analytical results and the validity of scientific conclusions if not properly addressed. This document provides detailed application notes and experimental protocols to identify, manage, and correct for these pervasive issues, enabling robust and reproducible HSI analysis in biomedical research and drug development.
Addressing Data Imbalance
The Challenge in HSI
Class imbalance occurs when the number of samples or pixels belonging to different classes varies significantly. In biomedical HSI, this is common; for instance, pathological tissue regions (regions of interest) are often vastly outnumbered by healthy tissue in training datasets [66] [4]. This imbalance can bias machine learning models toward the majority class, reducing their sensitivity to detect rare but critical phenotypes.
Strategic Solutions and Protocols
Strategy 1: Data Augmentation with Generative Models Synthetic data generation can effectively balance datasets by creating realistic, artificial samples of the underrepresented classes.
- Recommended Technique: Wasserstein Generative Adversarial Network with Gradient Penalty (WGAN-GP). This method stabilizes training and generates high-quality synthetic hyperspectral signatures [66].
- Experimental Protocol:
- Isolate Minority Class: Extract all spectral signatures (pixels) corresponding to the rare class (e.g., specific cell type, diseased tissue).
- Train WGAN-GP: Train the generator ((G)) and critic ((C)) networks on the isolated minority class spectra.
- Input: Raw spectral vectors from the minority class.
- Output: Synthetic spectral vectors that mimic the real minority class distribution.
- Generate Data: Use the trained generator to create a sufficient number of synthetic spectra to balance the class distribution.
- Incorporate: Add the synthetic data to the original training set, ensuring label consistency.
- Key Considerations: WGAN-GP is computationally intensive but highly effective for large-scale, complex HSI datasets [66].
Strategy 2: Algorithmic-Level Cost-Sensitivity Adjust the learning algorithm to be more sensitive to the minority class by assigning a higher penalty for misclassifying its samples.
- Implementation:
- Calculate Class Weights: Compute weights inversely proportional to class frequencies. For example, in a binary case:
weight_minority = total_samples / (2 * count_minority_samples). - Integrate into Loss Function: Incorporate these weights into the loss function during model training (e.g.,
weighted_cross_entropyin TensorFlow orclass_weightin scikit-learn).
- Calculate Class Weights: Compute weights inversely proportional to class frequencies. For example, in a binary case:
Table 1: Comparison of Data Imbalance Mitigation Strategies
| Strategy | Mechanism | Best-Suited Scenario | Advantages | Limitations |
|---|---|---|---|---|
| WGAN-GP Augmentation [66] | Generates synthetic spectral signatures for minority classes. | Large, complex datasets with severe imbalance. | Creates a robust, balanced dataset; improves model generalization. | High computational cost; complex implementation and training. |
| Class Weighting | Adjusts loss function to penalize minority class errors more. | Moderate imbalance; quick implementation is needed. | Simple to implement; no change to dataset size or model architecture. | Does not add new information; can be less effective for extreme imbalance. |
| Hierarchical Modeling [67] | Splits data into phases (e.g., early/late) and models each separately. | Data with known, distinct temporal or pathological phases. | Can improve accuracy by modeling sub-populations. | Requires prior knowledge to define phases; increases model complexity. |
Workflow Diagram: Managing Data Imbalance
Mitigating Blood and Reflection Artifacts
Impact on Biofluorescence Analysis
Blood and specular reflections introduce strong, confounding spectral signals that can mask the underlying biofluorescence of interest. Blood has strong absorption and scattering properties, distorting spectral signatures [4]. Reflections from surfaces like glass coverslips or wet tissue can saturate detectors and obscure spatial detail. Both artifacts lead to inaccurate feature extraction and quantification.
Strategic Solutions and Protocols
Strategy 1: Blood Pixel Identification and Filtering The spectral signature of blood can be identified and masked out from analysis.
- Experimental Protocol:
- Reference Collection: Collect reference spectral profiles for pure blood and unaffected tissue/background from control areas in your images [4] [67].
- Similarity Measurement: For each pixel in the HSI cube, calculate a similarity metric (e.g., Spectral Angle Mapper - SAM) between the pixel's spectrum and the reference blood spectrum.
- Thresholding: Apply a predefined threshold to the similarity map. Pixels with a similarity score above the threshold are classified as blood.
- Masking: Create a binary mask from these classifications and use it to exclude blood pixels from downstream analysis.
- Normalization: To minimize the effect of underlying skin or tissue spectra, normalize the hematoma data by dividing the raw spectrum of the blood-affected area by the spectrum of unaffected nearby skin [67].
Strategy 2: Reflection Removal via Decomposition Reflections can be handled by decomposing the image into transmission (desired signal) and reflection components.
- Recommended Technique: Utilize neural rendering frameworks like RAS-NeRF or NeRFReN, which are designed to separate reflective and transmissive components in a scene by leveraging geometric constraints and optimized rendering [68].
- Experimental Protocol:
- Data Acquisition: Capture multiple images of the sample from different viewpoints if possible. This provides the geometric information necessary for decomposition.
- Model Training: Train a reflection decomposition model (e.g., RAS-NeRF) on the multi-view data.
- Component Separation: The model outputs separate layers for the transmitted image (your target biofluorescence signal) and the reflection artifact.
- Analysis: Proceed with analysis using only the transmitted image component.
Table 2: Artifact Mitigation Techniques and Their Efficacy
| Artifact Type | Mitigation Strategy | Key Implementation Details | Reported Efficacy |
|---|---|---|---|
| Blood Pixels [4] [67] | Spectral Identification & Masking | Normalize using unaffected skin spectrum; use SAM or SID for detection. | More effective than reflection filtering, though not universally significant [4]. |
| Specular Reflections [4] [68] | Image Decomposition (e.g., RAS-NeRF) | Requires multi-view images; uses neural rendering and Fourier feature mapping. | High-quality reflection-free synthesis; improves depth estimation [68]. |
| General Light Reflections [4] | Filtering based on intensity thresholds | Identify and mask pixels with saturation-level intensity. | Effective for removing glaring artifacts, but may not handle complex reflections. |
Workflow Diagram: Managing Reflection and Blood Artifacts
Correcting for Noisy Pixels
HSI data is contaminated by various noise types including Gaussian noise (additive random variations), stripe noise (structured linear artifacts), deadline noise (lines of inactive pixels), and impulse noise (random spikes in intensity) [69]. These arise from sensor imperfections, environmental conditions, and the imaging process itself, degrading the signal-to-noise ratio (SNR) and obscuring subtle spectral features crucial for biofluorescence analysis.
Strategic Solutions and Protocols
Strategy 1: Advanced Denoising with Deep Learning Employ deep learning models designed to handle the spectral-spatial complexity of HSI noise.
- Recommended Technique: Hybrid Spectral Transformer Network (HSTNet). HSTNet integrates 3D Convolutional Neural Networks (3DCNN) for local feature extraction with a 3D Vision Transformer (3D-ViT) for capturing global dependencies in both spatial and spectral dimensions, effectively treating denoising as a 3D task [69].
- Experimental Protocol:
- Data Preparation: Partition your HSI cubes into small, overlapping 3D patches (e.g., spatial size 64x64, full spectral depth).
- Model Training: Train the HSTNet model on clean and artificially noisy HSI pairs if available, or use the model to directly learn noise residuals from your data.
- Inference: Apply the trained model to your entire HSI cube to generate a denoised output.
- Advantage: This approach simultaneously leverages spatial and spectral information, leading to superior noise removal while preserving structural and spectral integrity [69].
Strategy 2: Data-Driven Dimensionality Reduction Noise can be reduced by projecting the data onto a lower-dimensional space that retains the majority of the biologically relevant signal.
- Recommended Technique: Standard Deviation (STD)-based Band Selection. This simple, unsupervised method identifies and retains the most informative spectral bands, drastically reducing data volume and noise [70].
- Experimental Protocol:
- Calculate STD: For each spectral band across the entire image, compute the standard deviation of all pixel intensities.
- Rank Bands: Rank all spectral bands based on their calculated STD in descending order.
- Select Top Bands: Select the top (k) bands (e.g., 10-30 bands) with the highest standard deviation for all subsequent analysis.
- Validation: The retained bands should be evaluated on a validation set to ensure classification or regression performance is maintained.
Table 3: HSI Denoising and Dimensionality Reduction Methods
| Method | Principle | Complexity | Impact on Data | Recommended Use |
|---|---|---|---|---|
| HSTNet Denoising [69] | 3D CNN + Transformer for global/local feature learning. | High | Preserves full spatial-spectral dimensions. | High-quality data; computational resources available. |
| STD-based Band Selection [70] | Selects bands with highest variance. | Low | Reduces data size by up to 97.3%. | Fast pre-processing; resource-constrained environments. |
| Smoothing (e.g., Gaussian Filter) [4] | Applies a low-pass filter spatially or spectrally. | Very Low | Can blur fine spatial/spectral features. | Not recommended as it degraded performance in a study [4]. |
| Mutual Information Band Selection [70] | Selects bands most relevant to a class label. | Medium | Reduces data size significantly. | When accurate labels are available and interpretability is key. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Research Reagents and Solutions for HSI Experimentation
| Item | Function / Purpose | Example Application / Note |
|---|---|---|
| Stabilized Tungsten-Halogen Broadband Source [70] | Provides uniform, continuous spectrum from visible to NIR for reflectance/transmission HSI. | Essential for consistent illumination; often integrated with collimating optics. |
| Hyperspectral Imaging Microscope | High-resolution spatial and spectral data capture of microscopic samples. | Often uses push-broom or snapshot HSI technology; requires precise motorized stage. |
| Spectralon or White Reference Tile [67] | Provides a >99% reflective Lambertian surface for radiometric calibration. | Critical for converting raw digital numbers to reflectance, enabling cross-sample comparison. |
| LCTF or AOTF Tunable Filter [1] | Electronically filters specific wavelength bands without moving parts. | Enables flexible, rapid spectral selection in laboratory or stationary imaging setups. |
| Portable HSI Camera (e.g., Specim IQ) [67] | Push-broom scanner for mobile in-situ data collection. | Ideal for clinical settings, operating rooms, or fieldwork (400-1000 nm range). |
| WGAN-GP Software Implementation [66] | Generative model for creating synthetic spectral data to combat class imbalance. | Requires Python frameworks like TensorFlow/PyTorch; computationally intensive. |
| HSTNet or Similar Denoising Model [69] | Deep learning model for removing complex noise from HSI cubes. | Pre-trained models or custom training needed; superior to traditional filters. |
Integrated Experimental Workflow
This integrated protocol provides a step-by-step guide for processing HSI data, from acquisition to analysis, while incorporating the strategies outlined above.
Sample Preparation & HSI Acquisition:
- Prepare biological samples according to standard protocols.
- Acquire HSI datacubes using a calibrated HSI system. Include images of a white reference and dark current for calibration [1].
Preprocessing & Calibration:
- Convert raw data to reflectance/radiance using the white reference and dark current images.
- Apply Scaling: Standardize the spectral data (Z-score normalization) per patient/sample to minimize individual biases and enhance model convergence [4].
Artifact Mitigation (Parallel Options):
- Option A: Blood/Reflection Removal: Follow the protocols in Section 3.2 to identify and mask blood pixels or separate reflection components.
- Option B: Denoising: Apply the HSTNet denoising protocol from Section 4.2 to the calibrated datacube.
Dimensionality Reduction & Data Balancing:
- Perform STD-based band selection (Section 4.2) to reduce data volume and noise.
- Analyze class distribution. If imbalanced, apply WGAN-GP augmentation (Section 2.2) to the training set.
Analysis & Modeling:
- Proceed with downstream tasks such as spectral unmixing, classification, or regression using the cleaned, balanced, and reduced dataset.
Workflow Diagram: Integrated HSI Data Processing
Benchmarking Performance: Validation Against Gold Standards and Comparative Algorithm Analysis
In both biomedical research and clinical drug development, the precise assessment of tissue viability is a critical determinant of success, particularly in procedures involving anastomotic healing or evaluating the efficacy of novel cardiovascular and oncological therapeutics. The perfusion border—the demarcation between well-oxygenated and hypoxic tissue—serves as a crucial biomarker for surgical planning and therapeutic monitoring. Traditional methods for assessing this border often rely on subjective visual cues, which introduces significant variability. This application note details a prospective, comparative analysis of two advanced optical imaging modalities: Hyperspectral Imaging (HSI) and Fluorescence Angiography (FA) with Indocyanine Green (ICG). Framed within a broader thesis on hyperspectral imaging for biofluorescence characterization, this document provides researchers and drug development professionals with validated experimental protocols and quantitative data to guide the selection and implementation of these technologies in preclinical and clinical research.
Key Comparative Findings
A prospective, non-randomized, open-label, two-arm study directly compared HSI and FA for determining the transection margin in colorectal resections [71] [72]. The study involved 32 consecutive patients, with evaluable data from 30. The core finding was that both HSI and FA provided a comparable determination of the borderline between well-perfused and poorly perfused tissue (p = 0.704) [71]. Despite this agreement in outcome, the characteristics of the border zone differed between the modalities. FA presented a sharper, more distinct border, optimally assessed approximately 31 seconds after ICG injection. In contrast, HSI visualized a wider transition zone and revealed more pronounced differences between the proximal and distal borders [71]. Critically, the objective data from these imaging techniques led to a change in the planned surgical resection line in 15 out of 30 cases (50%), underscoring their potential to improve clinical and research outcomes over subjective assessment alone [71].
Table 1: Summary of Key Comparative Study Findings
| Parameter | Hyperspectral Imaging (HSI) | Fluorescence Angiography (FA) with ICG |
|---|---|---|
| Agreement on Perfusion Border | Comparable to FA (p = 0.704) [71] | Comparable to HSI (p = 0.704) [71] |
| Border Zone Characteristic | Wider transition zone [71] | Sharper, more distinct border [71] |
| Optimal Assessment Time | N/A (instantaneous measurement) | ~31 seconds post-injection [71] |
| Impact on Surgical Plan | Resection line changed in 15/30 cases [71] | Resection line changed in 15/30 cases [71] |
| Physiological Parameters | Tissue Oxygenation (StO₂), NIR Perfusion Index, Hemoglobin/Water Distribution [71] | Fluorescence intensity of intravascular tracer [71] |
The two modalities operate on distinct physical principles, interrogating different aspects of tissue physiology, which is a key consideration for research design.
Hyperspectral Imaging (HSI)
HSI is a non-invasive, contactless imaging technique that requires no exogenous contrast agents [71]. It works by illuminating tissue with light across the visible and near-infrared spectrum (500–1000 nm) and analyzing the reflected light to generate a three-dimensional "hypercube" of data (x, y, λ) [71]. This data is processed to produce quantitative, false-color maps of key physiological parameters [71]:
- Tissue Oxygenation (StO₂): Refers to the relative oxygenation of blood in the tissue at a penetration depth of ~1 mm, expressed as a percentage (0–100%) [71] [73].
- Near-Infrared Perfusion Index (NIR PI): Indicates oxygenation in deeper structures (4–6 mm depth) in arbitrary units (0–100) [71] [73].
- Organ Hemoglobin Index (OHI) and Tissue Water Index (TWI): Visualize the distribution of hemoglobin and water content, respectively, in arbitrary units (0–100) [71].
Fluorescence Angiography (FA) with ICG
FA is a well-established imaging technique that assesses blood flow dynamics using the exogenous contrast agent Indocyanine Green (ICG). Upon intravenous injection, ICG binds to plasma proteins and circulates within the vasculature. It is excited by near-infrared light (typically 805 nm) and emits fluorescence at a longer wavelength (825–850 nm) [71]. The intensity of the emitted fluorescence, typically measured on an 8-bit scale (0–255), is proportional to the local blood volume and flow [71]. The technique involves analyzing the time-fluorescence intensity curve to derive quantitative perfusion parameters such as TMAX (time to maximum intensity) and Slope (rate of intensity increase) [73].
Diagram 1: Logical workflow comparing the fundamental principles and outputs of HSI and FA technologies.
Experimental Protocols
The following protocols are adapted from the cited clinical studies and can be tailored for preclinical research settings.
Protocol for Hyperspectral Imaging Acquisition
This protocol utilizes the TIVITA Tissue system [71] [73].
Pre-imaging Setup:
- Turn off ambient lights in the operating or imaging room to standardize conditions.
- Position the HSI camera at a fixed distance of 50 cm from the target tissue surface. The system has a field of view of 8 x 6.5 cm² at this distance [71].
Data Acquisition:
Data Analysis:
- The integrated software automatically processes the hypercube to generate false-color maps of StO₂, NIR PI, OHI, and TWI within approximately 15 seconds [71] [73].
- The perfusion border is identified by a significant gradient or a drop below a threshold value in the StO₂ or NIR PI maps (e.g., StO₂ < 60% may indicate poor perfusion) [73].
Protocol for Fluorescence Angiography with ICG
This protocol is described for use with a system like the VisionSense-3 iridium camera [71] [73].
Pre-imaging Setup:
Contrast Agent Administration and Imaging:
- Prepare a solution of ICG (e.g., 25 mg diluted in 10 mL of distilled water) [73].
- Inject the ICG solution intravenously (minimum dose 0.2 mg/kg), followed by a 20 mL saline flush [73].
- Immediately begin recording the fluorescence video for at least 2 minutes to capture the first pass of the bolus and the wash-out phase [73].
Quantitative Analysis:
- Export the fluorescence video and use analysis software (e.g., ICG Analyzer Program) to plot a time-fluorescence intensity curve for regions of interest [73].
- Calculate key perfusion parameters from the curve as defined in Table 2.
Table 2: Key Quantitative Parameters for ICG Angiography and their Safe Values [73]
| Parameter | Definition | Reported "Safe Value" Reflecting Good Perfusion |
|---|---|---|
| TMAX | Time from first fluorescence increase to maximum intensity. | ≤ 30 seconds |
| T1/2MAX | Time to reach half of the maximum fluorescence intensity. | ≤ 10 seconds |
| Slope | The rate of fluorescence increase, calculated as FMAX/TMAX. | ≥ 5 |
| NIR Perfusion Index | Derived from HSI correlation; indicates deeper microcirculation. | ≥ 50 (Arbitrary Units) |
| Perfusion TR | Time ratio, calculated as T1/2MAX / TMAX. | High sensitivity for StO₂ ≥ 60% |
Diagram 2: Experimental workflow for the quantitative analysis of Fluorescence Angiography data.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for HSI and FA
| Item | Function/Description | Example & Notes |
|---|---|---|
| HSI System | For non-contact, contrast-free measurement of tissue physiology. | TIVITA Tissue System (Diaspective Vision GmbH). Provides quantitative maps of StO₂, NIR PI, OHI, and TWI [71] [73]. |
| Fluorescence Camera System | For visualizing and quantifying ICG fluorescence. | VisionSense-3 iridium (Medtronic) or 1588 AIM (Stryker). Must include NIR excitation and detection capabilities [71] [73]. |
| Indocyanine Green (ICG) | Exogenous fluorophore for vascular flow imaging. | 25 mg vials. Binds to plasma proteins; remains intravascular. Excitation: ~805 nm, Emission: ~830 nm [71] [73]. |
| Quantitative Analysis Software | Essential for extracting objective parameters from raw image data. | ICG Analyzer Program for fluorescence kinetics [73]. Vendor-specific or custom software for HSI parameter extraction [71]. |
| Standardized Phantom | For system calibration, performance validation, and cross-platform benchmarking. | Multi-parametric fluorescent phantoms. Critical for ensuring measurement accuracy and reproducibility in research [74]. |
Discussion and Research Implications
The comparative analysis indicates that HSI and FA are functionally complementary. FA excels in providing a high-contrast, dynamic visualization of vascular flow, making it ideal for identifying arterial inflow obstructions. HSI, meanwhile, provides a more comprehensive snapshot of tissue physiology, including oxygenation and hemoglobin content, which may be more directly related to metabolic need and viability [71] [75] [73].
For researchers, the choice between modalities depends on the specific research question. FA is highly suited for:
- Studies focused on vascular permeability, flow kinetics, and the efficacy of anti-angiogenic drugs.
- Applications where a sharp, real-time vascular map is critical.
HSI is preferable for:
- Investigating tissue oxygenation and hypoxia in cancer biology or wound healing models.
- Evaluating the metabolic effects of therapeutics beyond mere blood flow.
- Longitudinal studies where repeated measurements are needed, avoiding the cumulative dosing limits of exogenous agents.
The establishment of "safe values" for quantitative ICG parameters, validated against HSI-derived tissue oxygenation, represents a significant step towards standardizing perfusion assessment in both clinical and research settings [73]. Future work in biofluorescence characterization should focus on integrating these multimodal data streams to create unified predictive models of tissue viability and therapeutic response.
Maximal safe resection is a cornerstone of glioma treatment, yet a significant challenge persists: accurately identifying infiltrative tumor cells at the margins that are invisible to the human eye [76]. While 5-aminolevulinic acid (5-ALA) fluorescence-guided surgery with surgical microscopes has improved visualization, its sensitivity is often insufficient for detecting low-grade gliomas or the diffuse infiltrative zones of high-grade gliomas [63] [76].
Hyperspectral Imaging (HSI) is an emerging, non-invasive optical technique that captures both spatial and spectral information across hundreds of contiguous wavelength bands, generating a unique spectral "fingerprint" for each pixel in a scene [1] [20]. This label-free, non-ionizing method provides rich data on tissue composition and has shown promise for intraoperative tissue differentiation [77] [78]. This application note details an experimental protocol to quantitatively validate the superior sensitivity of HSI over standard surgical microscopy for detecting protoporphyrin IX (PpIX) in glioma biopsies.
Background
The 5-ALA Metabolic Pathway and PpIX Accumulation
The administration of 5-ALA bypasses the rate-limiting step of heme synthesis. In glioma cells, due to factors such as disrupted metabolism and decreased ferrochelatase activity, PpIX accumulates instead of being converted to heme. PpIX is a fluorophore that can be excited by violet-blue light, emitting red fluorescence [63].
Figure 1: The 5-ALA Metabolic Pathway and PpIX Detection. Exogenous 5-ALA leads to PpIX accumulation in glioma cells. While surgical microscopy has limited sensitivity for detecting the resulting fluorescence, HSI offers a highly sensitive, spectral-based detection method [63].
Technological Limitations of Surgical Microscopy
Standard surgical microscopes used in fluorescence-guided surgery employ a violet-blue excitation light (~400 nm) and long-pass emission filters to visualize PpIX fluorescence as a red color [63]. This method is primarily qualitative and suffers from limited sensitivity, particularly in regions with low tumor cell density or non-enhancing tumor areas, leading to an underestimation of tumor infiltration [63] [76].
Experimental Protocol: Validation Study
This protocol is designed for a controlled laboratory study using human glioma biopsies acquired during 5-ALA-mediated surgery, comparing HSI analysis to the gold standard of liquid chromatography-mass spectrometry (LC-MS).
Research Reagent Solutions
Table 1: Essential Materials and Reagents
| Item | Function/Description | Source/Example |
|---|---|---|
| 5-ALA | Pro-drug administered to patients to induce PpIX accumulation in tumor tissue. | Not specified [63] |
| PpIX Standard | High-purity chemical for creating calibration curves in LC-MS and phantom studies. | Enzo Life Sciences GmbH [63] |
| Coproporphyrin I & III | Porphyrin standards to account for potential spectral interference in HSI analysis. | Frontier Specialty Chemicals [63] |
| Pig Brain Homogenate | Surrogate matrix for developing and validating the LC-MS method and HSI calibration. | Obtained from a local butcher [63] |
| Dimethyl Sulfoxide (DMSO) | Solvent for preparing stock solutions of porphyrin standards. | Merck KGaA [63] |
| Mesoporphyrin (MpIX) | Suitable for use as an internal standard in LC-MS quantification. | Merck KGaA [63] |
Sample Preparation and Biopsy Collection
- Patient Preparation: Administer 5-ALA orally to patients 3-4 hours before surgery, following standard clinical protocols for glioma resection [63].
- Biopsy Collection: During tumor resection, collect multiple biopsy samples under both white light and fluorescent light guidance using a surgical microscope. Samples should represent a spectrum of tissues:
- Visibly Fluorescent Tissue: Core tumor tissue showing strong pink-red fluorescence under the surgical microscope.
- Non-Visibly Fluorescent Tissue: Peri-tumoral tissue appearing normal or non-fluorescent under the surgical microscope.
- Sample Handling: Immediately after collection, each biopsy should be divided into two halves:
- One half is flash-frozen in liquid nitrogen and stored at -80°C for subsequent LC-MS analysis.
- The other half is used for immediate HSI measurement without any processing (ex vivo).
Hyperspectral Image Acquisition and Analysis
- HSI System Setup: The protocol utilizes a wide-field HSI system built on an surgical microscope platform, incorporating [63]:
- A 405 nm LED for excitation.
- A scientific CMOS (sCMOS) camera for high-sensitivity detection.
- A Liquid Crystal Tunable Filter (LCTF) to scan the emission spectrum from 420 nm to 730 nm in fine steps (e.g., 3-5 nm).
- Image Acquisition:
- Place the fresh biopsy sample under the HSI camera.
- Acquire hyperspectral cubes in three modes: fluorescence mode (405 nm excitation), broadband white light mode, and dark mode (for background subtraction) [63].
- Data Preprocessing:
- Spectral Unmixing and PpIX Quantification:
- Employ advanced algorithms, such as deep learning-based correction models, to unmix the spectral data and isolate the specific PpIX signal from background autofluorescence and other interfering porphyrins [64].
- The output is a quantitative PpIX contribution map, expressed in µg/ml (HIPpIX), which can be converted to pmol/mg (HICalc-PpIX) using a calibration curve derived from spiked pig brain homogenates [63].
Gold Standard Quantification via LC-MS
- Sample Extraction:
- Homogenize the frozen biopsy samples or spiked pig brain surrogate.
- Extract porphyrins using a suitable solvent (e.g., DMSO). Include an internal standard (e.g., MpIX) to correct for recovery variations.
- LC-MS Analysis:
- Use Reversed-Phase Liquid Chromatography coupled to a Mass Spectrometer.
- Separate and quantify PpIX, Coproporphyrin I, and Coproporphyrin III based on their unique mass-to-charge ratios.
- Quantify concentrations using a calibration curve from spiked pig brain homogenates, with reported accuracy of 98-137% and a coefficient of variation of 5-14% [63].
Data Analysis and Validation
- Correlate HSI-derived PpIX concentrations (HICalc-PpIX) with the absolute concentrations obtained from LC-MS for each biopsy sample using Pearson correlation.
- Calculate the sensitivity and specificity of both HSI and surgical microscopy (using a binary fluorescent/non-fluorescent assessment) against the LC-MS gold standard. LC-MS can define a positive sample based on a PpIX concentration threshold above that found in normal brain tissue.
Results and Performance Comparison
The following table summarizes the expected performance outcomes based on published literature and the described validation study.
Table 2: Comparative Performance of PpIX Detection Methods
| Method | Principle | Sensitivity for Low PpIX | Quantitative Output | Key Limitations |
|---|---|---|---|---|
| Surgical Microscopy | Visual assessment of red fluorescence through a filter. | Low to moderate; fails in low-density infiltrative zones [63]. | Qualitative or semi-quantitative. | Subjective; limited by human vision and camera dynamics; poor detection of low-grade gliomas [76]. |
| Hyperspectral Imaging (HSI) | Spectral unmixing of the full fluorescence emission spectrum. | High; can detect PpIX in non-visibly fluorescing tumor samples [63]. | Quantitative (e.g., µg/ml). | Can overestimate PpIX without proper calibration; requires complex data processing [63]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Physical separation and mass-based quantification of molecules. | Gold standard for specificity and sensitivity [63]. | Absolute quantitative (pmol/mg). | Destructive; not real-time; not suitable for intraoperative use. |
This protocol provides a robust framework for validating the superior sensitivity of HSI over surgical microscopy. The core advantage of HSI lies in its ability to resolve the full emission spectrum of PpIX, allowing sophisticated algorithms to separate its signal from background tissue autofluorescence, which is not possible with the broad-band filters of surgical microscopes [63] [64]. Studies have confirmed that HSI can detect PpIX in samples deemed "non-fluorescent" under a surgical microscope, directly addressing the challenge of diffuse tumor infiltration [63].
A critical consideration is the need for rigorous calibration and advanced processing models. Initial studies indicate that HSI can overestimate PpIX concentration compared to LC-MS, highlighting the importance of using biological surrogates like pig brain homogenate and deep learning-based correction to improve accuracy [63] [64].
In conclusion, HSI represents a significant technological advancement for fluorescence-guided glioma surgery. By providing quantitative, highly sensitive detection of PpIX, it holds the potential to guide more complete tumor resections, particularly in critical marginal zones. Future work should focus on the integration of real-time HSI systems and analysis software directly into the neurosurgical workflow.
Hyperspectral imaging (HSI) has emerged as a powerful analytical technique that combines conventional imaging with spectroscopy to provide both spatial and chemical information about samples. A significant challenge in interpreting HSI data, particularly in biofluorescence characterization research, lies in accurately identifying and separating the signals of interest from complex mixtures. This application note provides a detailed comparative analysis of three fundamental algorithms—Linear Unmixing (LU), Matched Filter (MF), and Spectral Angle Mapper (SAM)—for hyperspectral image analysis in biological and pharmaceutical contexts. We evaluate their performance characteristics, establish standardized protocols for their implementation, and provide guidance for researchers and drug development professionals seeking to optimize their hyperspectral imaging workflows for biofluorescence applications.
Theoretical Foundations of the Algorithms
Core Mathematical Principles
Each algorithm operates on distinct mathematical principles that determine its suitability for specific applications. Linear Unmixing is grounded in the linear mixing model, where the measured spectrum at each pixel is assumed to be a linear combination of the spectral signatures of pure constituents (endmembers) weighted by their relative abundances [61]. The model is represented as: x = As + ε, where x is the measured spectrum vector, A is the matrix of known endmember spectra, s is the vector of abundances, and ε represents noise or error. LU solves for the abundance estimates by minimizing the residual error, often subject to constraints such as non-negativity and sum-to-one for physical realism [61] [59].
The Matched Filter is an adaptive target detection algorithm that maximizes the response of a target signature while suppressing the background response. It operates as a constrained energy minimization technique that does not require knowledge of all background endmembers, instead using a background statistics-based approach [3] [79]. The MF output for a pixel vector x is given by the expression: MF(x) = (x - μ)ᵀ C⁻¹ (t - μ) / (t - μ)ᵀ C⁻¹ (t - μ), where t is the target signature, μ is the mean background spectrum, and C is the background covariance matrix.
The Spectral Angle Mapper is a physically-based spectral classification algorithm that determines similarity between two spectra by calculating the angle between them as vectors in multidimensional space [80] [81]. The spectral angle θ between a test spectrum vector t and a reference spectrum vector r is computed as: θ = cos⁻¹[(t • r) / (||t|| ||r||)]. Smaller angles indicate greater similarity to the reference spectrum, with the algorithm being insensitive to variations in illumination intensity since it uses only the vector direction.
Algorithm Workflows and Relationships
The following diagram illustrates the core decision logic and workflow relationships between the three algorithms in a typical hyperspectral analysis scenario:
Performance Comparison and Quantitative Assessment
Comprehensive Algorithm Performance Metrics
Table 1: Comparative performance metrics of LU, MF, and SAM algorithms across critical evaluation parameters
| Performance Parameter | Linear Unmixing | Matched Filter | Spectral Angle Mapper |
|---|---|---|---|
| Sensitivity to Target Concentration | Linear response to concentration [3] | Linear response to concentration [3] | Non-linear; varies with spectral shape |
| Background Suppression | Excellent when endmembers properly defined [61] | Excellent background rejection [3] [79] | Moderate; affected by unknown backgrounds |
| Computational Efficiency | Moderate to high complexity [61] | Moderate complexity [3] | Low complexity; rapid calculation [80] |
| Required Prior Knowledge | Complete endmember spectra [61] [59] | Target spectrum only [3] [79] | Reference spectrum only [80] [81] |
| Robustness to Illumination | Sensitive to intensity variations | Sensitive to intensity variations | Invariant to illumination [80] [81] |
| Typical Application Context | Component quantification [61] [82] | Target detection [3] [79] | Classification/identification [80] [81] |
Experimental Performance Data
Table 2: Experimental results from comparative studies in biological and pharmaceutical applications
| Application Domain | Linear Unmixing Performance | Matched Filter Performance | Spectral Angle Mapper Performance | Reference Study |
|---|---|---|---|---|
| Ca²⁺ signaling in HASMCs | Linear response to Ca²⁺ concentration; effective autofluorescence separation [3] | Similar linear response to Ca²⁺; comparable to LU [3] | Not recommended for weak signals in autofluorescence [3] | [3] |
| Land Use/Land Cover Classification | Not evaluated | Overall Accuracy: ~90% (with PCA) [80] | Overall Accuracy: 66.67% [80] | [80] |
| Agricultural Classification | Not evaluated | Not evaluated | Overall Accuracy: 66.67% (vs. 33.33% for Parallelepiped) [81] | [81] |
| Mineral Classification | Not evaluated | Not evaluated | Outperformed by SID-SAM and SID-SCA hybrid approaches [83] | [83] |
| Pharmaceutical API Characterization | Implemented via MCR-ALS for multi-platform fusion [61] | Not evaluated | Not evaluated | [61] |
Experimental Protocols
Protocol 1: Linear Unmixing for Multi-Platform Image Fusion
This protocol adapts the MCR-ALS approach for fusing hyperspectral images from different spectroscopic platforms, based on the methodology applied to rice leaf cross-sections [61].
Materials and Reagents:
- Biological samples (e.g., tissue sections, cell cultures)
- Agarose for sample embedding
- Calcium fluoride slides and coverslips
- Nail polish for sealing
Procedure:
- Sample Preparation: Embed tissue samples in agarose and prepare cryosections of 7 μm thickness using a cryostat at -20°C. Mount sections on calcium fluoride slides, cover with calcium fluoride coverslips, and seal with nail polish.
- Multi-Modal Image Acquisition: Acquire hyperspectral images from each platform:
- Collect SR-FTIR HSI using a synchrotron infrared microscope
- Acquire Raman HSI with appropriate excitation wavelengths
- Obtain fluorescence HSI using relevant excitation/emission parameters
- Data Preprocessing: Balance images from different platforms in terms of spatial resolution, orientation, and scanned area. Perform dark current subtraction and flat-field correction.
- Data Structuring: Fuse the multiple HSI modalities into a single multiset structure containing all image blocks.
- MCR-ALS Analysis: Apply the MCR-ALS algorithm with appropriate constraints:
- Implement non-negativity constraints for both spectra and concentrations
- Apply spectral normalization
- Use optional constraints (e.g., closure, selectivity)
- Validation: Assess model quality through percent variance explained and analysis of residuals.
This protocol details the implementation of excitation-scanning HSI for dynamic cell signaling studies, enabling separation of Ca²⁺ signals from autofluorescence [3].
Materials and Reagents:
- Human Airway Smooth Muscle Cells (HASMCs)
- Dulbecco's Modified Eagles Medium (DMEM)
- Fetal bovine serum
- Cal 520-AM Ca²⁺ indicator (5 μM)
- NucBlue nuclear label
- Laminin-coated glass coverslips
- Extracellular buffer: 145 NaCl, 4 KCl
Procedure:
- Cell Culture: Maintain HASMCs in DMEM supplemented with 5% fetal bovine serum, growth factors, and antibiotics at 37°C and 5% CO₂. Seed cells onto laminin-coated coverslips and incubate for 48 hours until 70-80% confluency.
- Fluorescent Labeling:
- For Ca²⁺ labeling: Incubate with 5 μM Cal 520-AM at 37°C for 30 minutes
- For nuclear labeling: Incubate with NucBlue at 37°C for 20 minutes
- Hyperspectral Image Acquisition:
- Use an excitation-scanning HSI system with narrow-band tunable excitation
- Set emission detection with a broad-band or long-pass filter
- Acquire time-lapse HSI data with appropriate temporal resolution
- Algorithm Implementation: Apply each algorithm to the HSI data:
- Linear Unmixing: Use reference spectra from control samples
- Matched Filter: Apply with target Ca²⁺ spectrum
- Spectral Angle Mapper: Calculate spectral angles relative to reference
- Pixel Filtering: Implement theoretical sensitivity framework to reject pixels with signals below minimum detectable limit.
- Kinetic Analysis: Extract quantitative signal traces from unmixed data and analyze Ca²⁺ transient features.
The following workflow diagram illustrates the key steps in the excitation-scanning HSI protocol for dynamic cell signaling studies:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for hyperspectral biofluorescence imaging
| Item | Function/Application | Example Use Case |
|---|---|---|
| Cal 520-AM | Fluorescent Ca²⁺ indicator | Dynamic Ca²⁺ signaling studies in live cells [3] |
| NucBlue | Nuclear counterstain | Cell identification and segmentation in complex samples [3] |
| Calcium Fluoride Slides/Coverslips | Optical substrates for IR spectroscopy | Low-autofluorescence imaging in SR-FTIR HSI [61] |
| Agarose | Tissue embedding medium | Structural support for cryosectioning of delicate samples [61] |
| IRDye 680RD/800CW | NIR fluorescent labels | Multiplexed imaging in whole-animal cryo-imaging [82] |
| Sodium Fluorescein | Fluorescent tracer | Vascular imaging and permeability studies [82] |
| Active Pharmaceutical Ingredients (APIs) | Drug compound analysis | Pharmaceutical tablet characterization [84] [9] |
Implementation Guidelines and Best Practices
Algorithm Selection Framework
Choosing the appropriate algorithm depends on several factors related to the specific research question and data characteristics. For quantitative biofluorescence studies requiring precise component concentration measurements, particularly in complex biological environments with significant autofluorescence, Linear Unmixing generally provides superior performance when reference spectra are available [3]. The constrained implementation in MCR-ALS offers particular advantages for multi-platform data fusion, allowing integration of complementary information from different spectroscopic techniques [61].
For target detection applications where the signature of a specific fluorophore is known but background constituents are undefined or highly variable, the Matched Filter provides excellent performance with less computational burden than full unmixing [3] [79]. This approach is particularly valuable in drug distribution studies where target engagement needs to be identified against heterogeneous tissue backgrounds.
The Spectral Angle Mapper algorithm is most appropriate for classification tasks where illumination conditions cannot be controlled or normalized, due to its inherent invariance to intensity variations [80] [81]. However, its performance limitations in biological fluorescence applications with significant autofluorescence suggest it should be used cautiously for quantitative biofluorescence studies [3].
Optimization Strategies
- Spectral Preprocessing: For LU and MF applications, implement spectral normalization or standardization to mitigate intensity variations. For SAM, such preprocessing is generally unnecessary due to inherent intensity invariance [80] [81].
- Dimensionality Reduction: When processing high-dimensional HSI data, consider principal component analysis (PCA) as a preprocessing step to reduce computational burden while preserving essential spectral information [80].
- Reference Spectrum Quality: For all algorithms, the accuracy of reference/target spectra significantly impacts performance. Collect reference spectra using identical instrumentation parameters to the experimental data [3] [59].
- Validation Approaches: Implement cross-validation techniques when ground truth is unavailable. For biological applications, correlate HSI findings with complementary analytical techniques when possible [61].
This comprehensive comparison demonstrates that algorithm selection in hyperspectral biofluorescence imaging must be guided by specific application requirements. Linear Unmixing excels in quantitative applications requiring complete component separation, particularly when implemented through constrained approaches like MCR-ALS. Matched Filter provides an efficient alternative for specific target detection with strong background suppression. Spectral Angle Mapper offers computational efficiency and illumination invariance but with limitations in quantitative biofluorescence applications. By implementing the standardized protocols and guidelines presented herein, researchers can optimize their hyperspectral imaging workflows for more reliable and reproducible results in biofluorescence characterization and drug development research.
In hyperspectral imaging (HSI) for biofluorescence characterization research, the transition from promising experimental results to clinically viable tools hinges on rigorous external validation. External validation is the process of evaluating a predictive model's performance on data that was not used in its development, originating from different populations, species, or clinical cohorts. This process is critical for assessing a model's generalization capability—its ability to make accurate predictions on new, unseen data. In biomedical research, where models are increasingly developed to diagnose diseases like cancer or monitor tissue health, a failure to generalize can render a technologically advanced system useless in real-world clinical practice [85] [86] [87]. This application note provides a structured framework and detailed protocols for the external validation of HSI-based models, ensuring their robustness and reliability across species and clinical cohorts.
Quantitative Performance Benchmarks
Successful external validation is quantified by a drop in key performance metrics when a model is applied to an external test set, compared to its performance on internal data. The following benchmarks, drawn from recent literature, illustrate typical performance ranges and the importance of rigorous sampling.
Table 1: Performance Metrics of HSI Models in Medical Applications
| Application | Model/Dataset | Accuracy (%) | Sensitivity (%) | Specificity (%) | Notes | Source |
|---|---|---|---|---|---|---|
| Colorectal Cancer Detection | Excitation-Scanning HSI with Deep Learning | ~80 (Internal) | ~81 (Internal) | ~78 (Internal) | Performance on internal validation; external validation is required. | [85] |
| Head and Neck Cancer | 3D-CNN (Densenet3D) | 81 | 92 | 65 | Example of potential sensitivity-specificity trade-off. | [85] |
| Diabetic Foot Ulcer Assessment | PCA on HSI data | N/A | 83 | 100 | Highlights the potential for very high specificity in clinical use cases. | [87] |
| Skin Complications in Diabetes | ANN on HSI data | N/A | 95 | 85 | Demonstrates high sensitivity for early-stage detection. | [87] |
Table 2: Impact of Disjoint Sampling on HSI Classification Generalization
| Dataset | Reported Accuracy with Disjoint Sampling (%) | Reported Performance with Non-Disjoint Sampling | Key Implication | |
|---|---|---|---|---|
| Indian Pines | 96.36 | Inflated and unreliable | Disjoint sampling provides a true measure of model generalization. | [86] |
| Pavia University | 99.73 | Inflated and unreliable | Prevents data leakage and mitigates overfitting. | [86] |
| University of Houston | 98.29 | Inflated and unreliable | Ensures unbiased evaluation for real-world application. | [86] |
| Salinas | 99.88 | Inflated and unreliable | Facilitates fair and accurate model comparison. | [86] |
Experimental Protocols
Protocol 1: Implementing Disjoint Sampling for Robust HSI Model Development
Principle: Ensure that the training, validation, and test sets are strictly separated, with no spatial or spectral data from the same sample or patient appearing in more than one set [86]. This is the foundational step for any subsequent external validation.
Materials:
- Hyperspectral data cube (format:
[spatial_x, spatial_y, spectral_λ]) - Ground truth label map
- Data processing software (e.g., Python with NumPy, SciKit-learn)
Procedure:
- Data Partitioning by Unique Identifier: Instead of randomly splitting pixels, partition the data based on unique biological or physical identifiers.
- For plant studies: Split by individual plant. All pixels from one plant belong to only one set (training, validation, or test).
- For animal studies: Split by individual animal.
- For clinical tissue studies: Split by individual patient. All tissue samples from a single patient are assigned to the same set [86].
- Stratified Sampling: Within the above constraint, ensure that each set (training, validation, test) has a representative distribution of all target classes (e.g., healthy, diseased) to avoid bias.
- Spatial Separation (for remote sensing): If dealing with geographical data, ensure a physical distance between the areas designated for training and testing to prevent spatial autocorrelation from inflating performance [86].
- Algorithmic Implementation:
- Identify all unique subjects (e.g., patient IDs, plant IDs) in the dataset.
- Randomly shuffle the list of unique subjects.
- Assign subjects to training (e.g., 70%), validation (e.g., 15%), and test (e.g., 15%) groups.
- Extract all HSI patches and their corresponding labels based on this subject-level grouping.
Protocol 2: External Validation Across Species
Principle: Test the model trained on data from one species on HSI data acquired from a different, phylogenetically distinct species to assess the robustness of biofluorescence signatures.
Materials:
- Fully trained HSI classification model (e.g., a 3D-CNN or Spatial-Spectral Transformer).
- HSI dataset from primary species (e.g., Mus musculus).
- HSI dataset from secondary, external species (e.g., Rattus norvegicus, or Sus scrofa).
- Standardized HSI acquisition platform.
Procedure:
- Model Training: Train your HSI model to completion using the disjoint training and validation sets from the primary species.
- Data Harmonization: Pre-process the external species' HSI data using the identical workflow (e.g., flat-field correction, spectral normalization, noise filtering) applied to the primary training data.
- Blinded Prediction: Input the pre-processed HSI cubes from the external species into the trained model without providing the true labels to the testing software.
- Performance Analysis: Calculate performance metrics (Accuracy, Sensitivity, Specificity, F1-Score) by comparing the model's predictions against the ground truth for the external species.
- Signature Analysis: Investigate model misclassifications by analyzing the spectral signatures of incorrectly classified pixels. This can reveal species-specific spectral differences that the model failed to learn during training on a single species.
Protocol 3: External Validation Across Clinical Cohorts
Principle: Evaluate a model developed on data from one clinical cohort (e.g., a single hospital) on data collected from a different cohort (e.g., a different hospital with varying demographics and equipment) [85] [87].
Materials:
- HSI model trained on data from "Cohort A".
- De-identified HSI dataset from "Cohort B", collected with a different imaging system or patient population.
- Associated clinical metadata for both cohorts.
Procedure:
- Cohort Characterization: Document key differences between Cohort A (training) and Cohort B (testing), including:
- HSI camera manufacturer and model.
- Illumination source and intensity.
- Patient demographics (age, sex, ethnicity).
- Disease prevalence and severity.
- Cross-Cohort Calibration: Apply domain adaptation techniques, such as spectral normalization or more advanced unsupervised domain alignment methods, to minimize the technical variability between the two datasets. Note: The model must not be retrained on any data from Cohort B at this stage.
- Validation and Analysis:
- Run the model from Cohort A on the calibrated data from Cohort B.
- Compute performance metrics and compare them to the model's internal validation performance.
- Use interpretability tools like Grad-CAM (Gradient-weighted Class Activation Mapping) to visualize if the model is focusing on biologically relevant regions in the new cohort or being misled by technical artifacts [85].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for HSI Biofluorescence Research
| Item | Function/Application | Example Specification |
|---|---|---|
| Hyperspectral Camera | Captures the 3D hypercube (x, y, λ). Critical for signal acquisition. | Pushbroom or snapshot type; spectral range 400-1000 nm for biofluorescence [88] [89]. |
| Tunable Filter | Enables spectral scanning by selecting narrow excitation or emission bands. | Liquid Crystal Tunable Filter (LCTF) or filter wheel [85] [87]. |
| Standardized Calibration Targets | For radiometric and spectral calibration to ensure consistency across sessions and devices. | White reference panel, fluorescent calibration standards. |
| Biofluorescence Standards | Provide a consistent fluorescence signal for validating system performance and cross-model comparison. | Solutions of known fluorophores (e.g., fluorescein, quantum dots) [10]. |
| Domain Adaptation Software | Algorithms to minimize technical variability between data from different cohorts or species, improving generalization. | Python libraries for ComBat, cycleGAN, or other normalization techniques. |
Workflow and Data Relationship Visualizations
External Validation Workflow This diagram outlines the critical path from internal development to external validation, emphasizing that the model must be locked before exposure to external data.
Challenges and Solutions This diagram maps the primary challenges in external validation to the specific solutions and methodologies required to overcome them and achieve a generalizable model.
Hyperspectral imaging (HSI) has emerged as a powerful, non-invasive tool in the armamentarium of cancer diagnostics. By capturing spatial and spectral information across hundreds of contiguous wavelength bands, HSI generates unique spectral fingerprints that enable precise differentiation of malignant from healthy tissues based on their distinct biochemical and morphological properties [90] [44]. This Application Note provides a structured compilation of quantitative performance metrics and detailed experimental protocols for implementing HSI in cancer detection, with a specific focus on objectivity, reproducibility, and integration into biofluorescence characterization research. The data presented herein serve as a critical reference for researchers and drug development professionals seeking to validate HSI methodologies and incorporate them into standardized workflows for enhanced diagnostic and therapeutic assessment.
Quantitative Performance Metrics
The integration of HSI with advanced analytical algorithms, particularly deep learning models, has demonstrated exceptional performance in classifying various cancer types. The following tables summarize key metrics reported in recent, rigorous studies.
Table 1: Performance Metrics for HSI in Detecting Various Cancers
| Cancer Type | Model/Algorithm | Sensitivity (%) | Specificity (%) | Accuracy (%) | Citation |
|---|---|---|---|---|---|
| Skin Cancer (AK, BCC, SK) | Convolutional Neural Network (CNN) | - | - | 98.0 | [91] |
| Head and Neck Cancer | Linear Discriminant Analysis (LDA) | 91.0 | 93.0 | 92.0 | [92] |
| Colorectal Cancer | Deep Learning (NN) | 86.0 | 95.0 | - | [90] [93] |
| Esophageal Adenocarcinoma (Therapy Response Prediction) | 3D-CNN | - | - | 68.0 | [93] |
| Head and Neck Cancer (Tumor vs. Benign) | Adaptive Deep Learning (Auto-encoder) | 92.3 | 91.3 | - | [94] |
Table 2: Comparison of Algorithm Performance for Head and Neck Cancer Detection
| Algorithm | Sensitivity (%) | Specificity (%) | Accuracy (%) |
|---|---|---|---|
| Linear Discriminant Analysis (LDA) | 91.0 | 93.0 | 92.0 |
| Convolutional Neural Network (CNN) | 77.0 | 86.0 | 82.0 |
| Support Vector Machine (SVM) | 48.0 | 89.0 | 76.0 |
Source: Meta-analysis of HNC studies [92]
Detailed Experimental Protocols
Protocol 1: HSI for Skin Cancer Classification using the SAVE Algorithm
This protocol details a novel method for enhancing the contrast of skin lesions by converting standard RGB images into narrow-band images (NBI) [91].
- Objective: To accurately classify actinic keratosis (AK), basal cell carcinoma (BCC), and seborrheic keratosis (SK) using HSI-based contrast enhancement.
- Materials:
- Imaging Source: 954 skin lesion images from the International Skin Imaging Collaboration (ISIC) archive.
- Calibration Tool: Macbeth Color Checker (X-Rite Classic) for color calibration.
- Annotation Software: Roboflow platform for image annotation and dataset management.
- Computational Framework: Python environment with libraries for image processing and deep learning (e.g., TensorFlow, PyTorch).
- Procedure:
- Image Acquisition and Preprocessing: Download and standardize all RGB images to a resolution of 640 x 640 pixels.
- Color Calibration: Capture an image of the Macbeth Color Checker using the imaging system. Establish a transformation matrix to convert the camera's sRGB color space to the CIE 1931 XYZ color space, correcting for non-linear response and color distortion.
- NBI Transformation (SAVE Algorithm): Apply the Spectrum-Aided Vision Enhancer (SAVE) algorithm to convert the calibrated RGB images into simulated NBI. This process selectively uses narrow bands of light (e.g., 415 nm and 540 nm) to enhance the visualization of superficial vasculature and deeper structures, increasing the contrast between cancerous and normal tissue.
- Model Training and Classification: Split the generated dataset (original RGB and SAVE-transformed images) into training and validation sets. Train ten different machine learning classifiers (including CNN, Random Forest, YOLOv8, and various SVM classifiers) to differentiate between AK, BCC, and SK.
- Validation: Evaluate model performance using a separate test set. Calculate accuracy, sensitivity, specificity, and mean average precision (mAP).
Protocol 2: Deep Learning for Colorectal Cancer Detection with Preprocessing Optimization
This protocol focuses on the critical impact of data preprocessing on the performance of deep learning models for identifying colorectal cancer in HSI datacubes [4].
- Objective: To systematically evaluate the effect of different preprocessing combinations on the sensitivity and specificity of a 3D-CNN for colorectal cancer detection.
- Materials:
- HSI System: Push-broom TIVITA Tissue camera system.
- Dataset: Hyperspectral datacubes from 56 patients, with expert-annotated ground truth masks.
- Computational Resources: High-performance computing cluster with GPU acceleration.
- Software: Python with scientific computing libraries (NumPy, SciPy) and deep learning frameworks.
- Procedure:
- Data Acquisition: Capture HSI datacubes of resected colorectal tissue within five minutes post-resection. Each datacube has dimensions of 480 x 640 pixels with 100 spectral bands (500-1000 nm). Exclude the noisy 500-540 nm range, resulting in 92 used bands.
- Preprocessing Pipeline:
- Scaling: Apply either Normalization (scaling to a [0,1] range) or Standardization (transforming data to have zero mean and unit variance) per spectral band across the entire dataset.
- Noise Reduction (Smoothing): Test 1D (spectral), 2D (spatial), and 3D (combined) smoothing using Median, Gaussian, or Savitsky-Golay filters.
- Filtering: Identify and remove pixels with strong blood absorption or light reflections using spectral unmixing or thresholding techniques.
- Patch Extraction: For each annotated pixel, extract a 3D patch from the hyperspectral cube. Common patch sizes are 3x3 or 5x5 pixels.
- Model Training and Evaluation:
- Train a 3D-CNN model for binary classification (cancerous vs. non-malignant tissue).
- To ensure fair comparison, maintain identical training conditions (data order, model initialization, random seeds) while varying only the preprocessing steps.
- Evaluate performance based on sensitivity and specificity on a held-out test set.
- Key Findings: Standardization consistently outperformed normalization. Larger input patch sizes (5x5) enhanced performance by capturing more spatial context. Contrary to expectations, smoothing filters often degraded model performance, and blood filtering was more effective than filtering light reflections [4].
Signaling Pathways and Workflows
Single-Cell HSI and Transcriptomics Integration Workflow
The following diagram illustrates the SpectralSeq workflow, which correlates hyperspectral autofluorescence with gene expression in single cells.
HSI Data Processing and Analysis Pipeline
This diagram outlines the general computational workflow for HSI data in cancer detection, from raw data to diagnostic classification.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions and Materials for HSI Cancer Detection
| Item | Function/Application | Example/Note |
|---|---|---|
| Push-broom HSI Camera | Captiates spatial and spectral data line-by-line, generating a 3D hypercube. Suitable for ex vivo tissue analysis. | TIVITA Tissue system; used for colorectal cancer detection [4]. |
| Hyperspectral Microscope | Enables single-cell level hyperspectral autofluorescence imaging for correlating spectral features with molecular states. | Olympus IX83 inverted microscope customized for 15-color imaging [95]. |
| Color Calibration Target | Essential for standardizing colors and ensuring consistency across different imaging sessions and setups. | Macbeth Color Checker (X-Rite Classic) [91]. |
| Cell Picking System | Automates the isolation of single cells from a culture dish for downstream transcriptomic analysis. | Used in SpectralSeq workflow after HSI [95]. |
| Deep Learning Frameworks | Provide the computational environment for developing and training models for tissue classification and feature extraction. | TensorFlow, PyTorch; used for 2D-CNN, 3D-CNN, and Hybrid-SN models [94] [93]. |
| Spectral Analysis Software | For preprocessing, visualizing, and analyzing hyperspectral datacubes, including scaling, filtering, and spectral unmixing. | Python with NumPy, SciPy, Scikit-learn; critical for data preparation [4]. |
Conclusion
Hyperspectral imaging has firmly established itself as a powerful and versatile modality for biofluorescence characterization, offering significant advantages over conventional imaging through its unique combination of spatial and spectral data. The technology provides researchers and clinicians with a non-destructive, label-free method for sensitive detection and quantification of biochemical signals, from subcellular dynamics to tissue-level pathology. While challenges remain in workflow integration, data optimization, and standardization, the continued development of advanced calibration techniques, robust preprocessing pipelines, and validated analytical algorithms is rapidly addressing these limitations. The future of HSI in biomedical research is exceptionally promising, with clear pathways for clinical translation in areas such as real-time surgical guidance, high-content drug screening, and personalized medicine diagnostics. As hardware becomes more accessible and data analysis more sophisticated, HSI is poised to become an indispensable tool in the advanced imaging arsenal.
References
- 1. Hyperspectral Imaging [https://arxiv.org/html/2508.08107v1]
- 2. High‐Speed Hyperspectral Imaging for Near Infrared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12021105/]
- 3. Comparing Performance of Spectral Image Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10295298/]
- 4. Exploring the role of preprocessing combinations in ... [https://www.nature.com/articles/s41598-025-20735-x]
- 5. AI Deep Learning Advances Hyperspectral Imaging for ... [https://www.spectroscopyonline.com/view/ai-deep-learning-advances-hyperspectral-imaging-for-earth-observation]
- 6. HyperSpectral imaging microscopy for identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3517021/]
- 7. Pre-processing visualization of hyperspectral fluorescent ... [https://www.nature.com/articles/s41467-020-14486-8]
- 8. Application of Raman hyperspectral imaging for bio-fluid ... [https://www.sciencedirect.com/science/article/abs/pii/S1386142525002392]
- 9. Characterization of Pharmaceutical Tablets Using UV ... [https://headwallphotonics.com/published-research/characterization-of-pharmaceutical-tablets-using-uv-hyperspectral-imaging-as-a-rapid-in-line-analysis-tool/]
- 10. Hyperspectral and Fluorescence Imaging Approaches for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11085301/]
- 11. Hyperspectral imaging combined with fluorescence for the ... [https://www.sciencedirect.com/science/article/pii/S0023643823003067]
- 12. Comparing Methods for Analysis of Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8161548/]
- 13. Compressive fluorescence microscopy for biological and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3387031/]
- 14. sCMOS vs CCD: Advancing High-Speed CARS ... [https://www.spectroscopyonline.com/view/scmos-vs-ccd-advancing-high-speed-cars-spectroscopy]
- 15. A Comparison of EMCCD vs sCMOS Cameras [https://andor.oxinst.com/learning/view/article/comparing-scmos]
- 16. sCMOS vs. EMCCD: Choosing the Right Scientific Camera for ... [https://www.revealerhighspeed.com/scmos-vs-emccd-choosing-the-right-scientific-camera-for-your-needs.html]
- 17. Fluorescence excitation-emission-matrix hyperspectral ... [https://opg.optica.org/abstract.cfm?uri=cleopr-2024-We2G_3]
- 18. A review of fluorescence imaging system supported by ... [https://www.sciencedirect.com/science/article/abs/pii/S0956713524007576]
- 19. Spectral reflectance imaging with dual-illumination and ... [https://opg.optica.org/oe/abstract.cfm?uri=oe-33-21-44191]
- 20. Hyperspectral imaging benchmark based on machine ... [https://www.nature.com/articles/s41698-023-00475-9]
- 21. Phasor-based hyperspectral snapshot microscopy allows ... [https://www.nature.com/articles/s42003-021-02266-z]
- 22. The spectral phasor approach to resolving membrane ... [https://www.sciencedirect.com/science/article/abs/pii/S0076687924000272]
- 23. Detecting Bacterial Biofilms Using Fluorescence ... [https://www.mdpi.com/1424-8220/21/6/2213]
- 24. The spectral phasor approach to resolving membrane ... [https://pubmed.ncbi.nlm.nih.gov/38971597/]
- 25. A single-shot hyperspectral phasor camera for fast, multi ... [https://www.sciencedirect.com/science/article/pii/S2667237523000565]
- 26. Comparing Performance of Spectral Image Analysis ... [https://www.mdpi.com/2306-5354/10/6/642]
- 27. A New Method for Convenient and Efficient Multicolor ... [https://www.leica-microsystems.com/science-lab/life-science/a-new-method-for-convenient-and-efficient-multicolor-imaging/]
- 28. Full spectrum fluorescence lifetime imaging with 0.5 nm ... [https://www.nature.com/articles/s41467-021-26837-0]
- 29. Microscopy is better in color: development of a streamlined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9352297/]
- 30. Modern Trends and Recent Applications of Hyperspectral ... [https://www.mdpi.com/2227-7080/13/5/170]
- 31. So you think you can PLS-DA? | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-019-3310-7]
- 32. Partial Least Squares Discriminant Analysis (PLS-DA) [https://www.metabolon.com/bioinformatics/pls-da/]
- 33. Partial Least Squares Discriminant Analysis and Bayesian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6316795/]
- 34. [1811.03707] Validating Hyperspectral Image Segmentation [https://arxiv.org/abs/1811.03707]
- 35. Unsupervised segmentation of biomedical hyperspectral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9774878/]
- 36. Calcium Signaling in Airway Smooth Muscle - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2645299/]
- 37. Calcium, a multitasking signaling actor in airway smooth ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2014.00296/full]
- 38. Which Hyperspectral Camera is Best for Cell Activity ... [https://www.chnspec.net/Cell-activity-monitoring-hyperspectral.html]
- 39. Measuring calcium dynamics in living cells with Genetically ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2654717/]
- 40. Engineering of NEMO as calcium indicators with large ... [https://www.nature.com/articles/s41592-023-01852-9]
- 41. Herschel vision: A hyperspectral image processing ... [https://www.sciencedirect.com/science/article/pii/S2352711025000561]
- 42. SignalStar® Panel Builder for mIHC Panel Design [https://www.cellsignal.com/applications/signalstar-multiplex-ihc-panel-builder?srsltid=AfmBOopRk25yVImA-8BEiag5zJGcs_-RfQgd6uC1oi2sHwfwaj_0xfI3]
- 43. Intraoperative Assessment of Tumor Margins in Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9818424/]
- 44. Recent Advances in Perfusion Assessment in Clinical ... [https://www.mdpi.com/2079-9292/14/17/3439]
- 45. Frontiers | Spectroscopic characterization of bacterial colonies... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1530955/full]
- 46. Multi-molecular hyperspectral PRM-SRS microscopy [https://pmc.ncbi.nlm.nih.gov/articles/PMC10881988/]
- 47. of Raman Application for bio-fluid spots... hyperspectral imaging [https://pubmed.ncbi.nlm.nih.gov/40010148/]
- 48. Hyperspectral imaging for environmental monitoring [https://www.specim.com/hyperspectral-imaging-applications/environmental-monitoring/]
- 49. Progress in the application of hyperspectral imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226550/]
- 50. Hyperspectral imaging and its applications: A review [https://www.sciencedirect.com/science/article/pii/S2405844024092399]
- 51. Neural illumination calibration for surgical workflow ... [https://pubmed.ncbi.nlm.nih.gov/41055831/]
- 52. Neural illumination calibration for surgical workflow ... [https://link.springer.com/article/10.1007/s11548-025-03525-8]
- 53. Comparison of preprocessing techniques to reduce ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9541333/]
- 54. Consideration of smoothing techniques for hyperspectral ... [https://www.sciencedirect.com/science/article/abs/pii/S0924271605001012]
- 55. Evaluating Normalization Methods for Robust Spectral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763101/]
- 56. Hyperspectral Imaging for Foreign Matter Detection in Foods [https://www.mdpi.com/2304-8158/14/17/3026]
- 57. Hyperspectral imaging and spectral unmixing for improving ... [https://opg.optica.org/boe/abstract.cfm?uri=boe-12-1-395]
- 58. SUFI: an automated approach to spectral unmixing of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9878864/]
- 59. Spectral Imaging and Linear Unmixing [https://www.microscopyu.com/techniques/confocal/spectral-imaging-and-linear-unmixing]
- 60. Multispectral imaging for characterizing autofluorescent ... [https://www.nature.com/articles/s41598-024-61020-7]
- 61. Linear unmixing protocol for hyperspectral image fusion ... [https://www.nature.com/articles/s41598-021-98000-0]
- 62. Multi-excitation hyperspectral autofluorescence imaging for ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267019302569]
- 63. Integrating mass spectrometry and hyperspectral imaging ... [https://www.nature.com/articles/s41598-025-26245-0]
- 64. Deep learning-based hyperspectral image correction and ... [https://www.sciencedirect.com/science/article/pii/S2589004224024982]
- 65. Quantitative Hyperspectral Reflectance Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3705521/]
- 66. An Automated Classification Method for Acute Leukemia in ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400525018246]
- 67. Age prediction of hematoma using hyperspectral imaging ... [https://link.springer.com/article/10.1007/s12024-025-01076-7]
- 68. RAS-NeRF for novel view synthesis of complex reflective ... [https://www.nature.com/articles/s40494-025-01727-6]
- 69. Hyperspectral Image Denoising through Hybrid Spectral ... [https://www.sciencedirect.com/science/article/abs/pii/S027311772501021X]
- 70. Dimensionality reduction in hyperspectral imaging using ... [https://www.nature.com/articles/s41598-025-21738-4]
- 71. Comparison of hyperspectral imaging and fluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7801293/]
- 72. Comparison of hyperspectral imaging and fluorescence ... [https://pubmed.ncbi.nlm.nih.gov/32968892/]
- 73. The Safe Values of Quantitative Perfusion Parameters ... [https://www.mdpi.com/2227-9059/11/7/2029]
- 74. Impact of signal-to-noise ratio and contrast definition on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11256003/]
- 75. Evaluation of gastric tube blood flow by multispectral ... [https://www.sciencedirect.com/science/article/pii/S2589845024000381]
- 76. Optical Methods for Brain Tumor Detection: A Systematic ... [https://www.mdpi.com/2077-0383/13/9/2676]
- 77. Hyperspectral imaging for tumor resection guidance in surgery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12327654/]
- 78. Technological Frontiers in Brain Cancer: A Systematic Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11394276/]
- 79. Influence of band selection and target estimation error on ... [https://opg.optica.org/ao/abstract.cfm?uri=ao-50-22-4276]
- 80. LAND USE AND LAND COVER CLASSIFICATION USING ... [https://isprs-archives.copernicus.org/articles/XLII-2-W13/1841/2019/]
- 81. Performance of Spectral Angle Mapper and Parallelepiped ... [https://thesai.org/Publications/ViewPaper?Volume=7&Issue=5&Code=IJACSA&SerialNo=9]
- 82. Hyperspectral imaging and spectral unmixing for improving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7818953/]
- 83. Performance evaluation of hyperspectral classification ... [https://www.sciencedirect.com/science/article/pii/S2213020916302099]
- 84. Characterization of Pharmaceutical Tablets Using UV ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8271527/]
- 85. Fluorescence excitation-scanning hyperspectral imaging ... [https://www.nature.com/articles/s41598-024-64917-5]
- 86. Improving Generalization for Hyperspectral Image ... [https://www.techscience.com/cmc/v81n1/58367/html]
- 87. Advancing hyperspectral imaging and machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11629177/]
- 88. Hyperspectral imaging [https://en.wikipedia.org/wiki/Hyperspectral_imaging]
- 89. What is hyperspectral Imaging?: A Comprehensive Guide [https://www.specim.com/technology/what-is-hyperspectral-imaging/]
- 90. Hyperspectral Imaging Is Transforming Science, Medicine, ... [https://www.spectroscopyonline.com/view/hyperspectral-imaging-is-transforming-science-medicine-and-industry]
- 91. Hyperspectral Imaging for Enhanced Skin Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292285/]
- 92. Advancements in Hyperspectral Imaging and Computer ... [https://www.mdpi.com/2227-9059/12/10/2315]
- 93. Artificial neural networks as a prognostic tool using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495013/]
- 94. Deep learning-based time series prediction in multispectral ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1605865/full]
- 95. Integration of hyperspectral imaging and transcriptomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315715/]