Overcoming Penetration Depth Limits in Fluorescence Imaging: From NIR Probes to Clinical Solutions
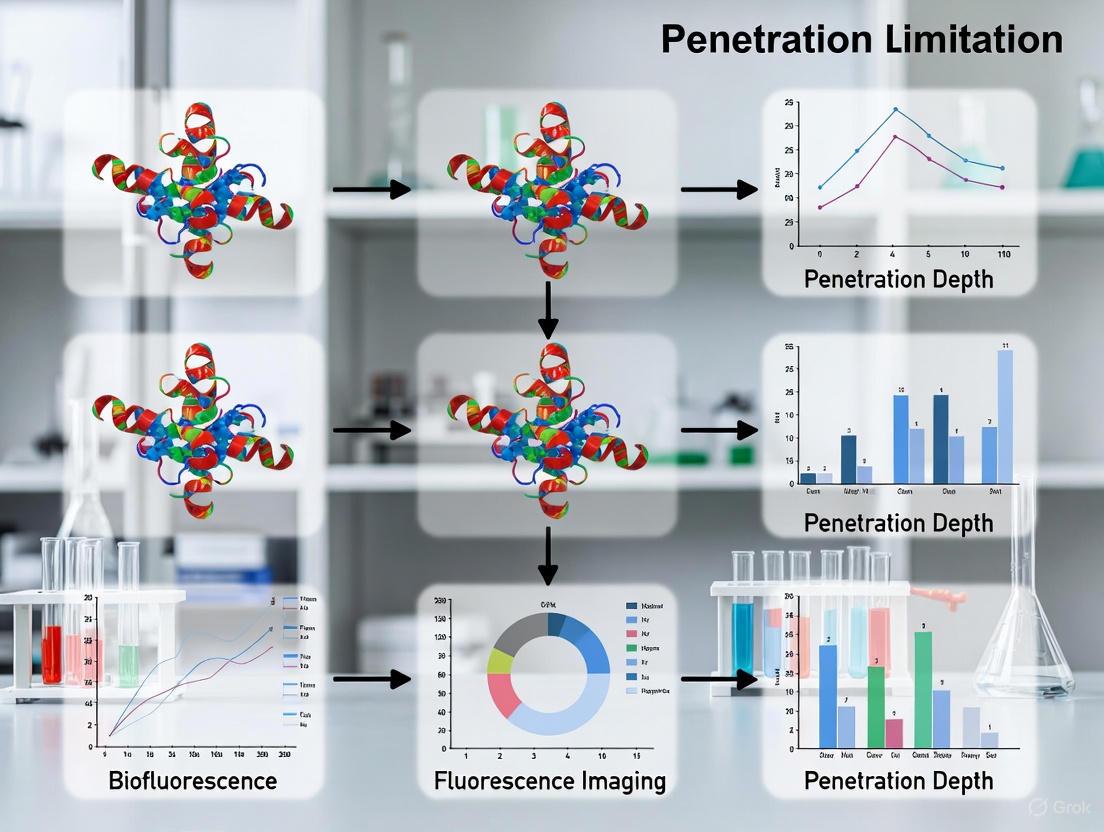
This article provides a comprehensive analysis of the penetration depth limitations inherent to fluorescence imaging, a critical challenge for researchers and drug development professionals.
Overcoming Penetration Depth Limits in Fluorescence Imaging: From NIR Probes to Clinical Solutions
Abstract
This article provides a comprehensive analysis of the penetration depth limitations inherent to fluorescence imaging, a critical challenge for researchers and drug development professionals. We explore the foundational physics of light-tissue interactions, including scattering and absorption, which constrain imaging depth and resolution. The review covers methodological breakthroughs, such as imaging in the Second Near-Infrared (NIR-II) window and the development of novel fluorophores, which significantly enhance signal-to-background ratios. We also detail practical troubleshooting and optimization strategies, from advanced denoising algorithms to probe design, that improve imaging efficacy in deep tissues. Finally, a comparative analysis validates these solutions against established clinical standards, assessing their potential for translation into areas like image-guided surgery and therapeutic monitoring. The synthesized insights aim to guide the strategic implementation of fluorescence imaging technologies in preclinical and clinical research.
The Physics of Light in Tissue: Understanding the Core Barriers to Deep Imaging
Fundamental Principles of Fluorescence and Signal Generation
Core Principles of Fluorescence
What is the fundamental process behind fluorescence generation?
Fluorescence is a three-stage process that occurs in molecules known as fluorophores or fluorescent dyes [1]:
- Excitation: A fluorophore absorbs a photon of light from an external source (e.g., a lamp or laser), elevating it to a higher-energy excited electronic state (Sâ‚´) [1].
- Excited-State Lifetime: The fluorophore resides in the excited state for a short time (typically 1–10 nanoseconds). During this period, it undergoes conformational changes and interacts with its environment, losing some energy and relaxing to a lower vibrational state (Sâ‚) [1].
- Emission: The fluorophore returns to its ground state (Sâ‚€) by emitting a photon of light. Because energy was lost during the excited-state lifetime, this emitted photon has lower energy and a longer wavelength than the excitation photon. This difference in wavelength is known as the Stokes Shift [1].
The Stokes shift is crucial for sensitivity, as it allows the emission light to be distinguished from the excitation light [1].
Diagram of the fluorescence process (Jablonski diagram).
What are the key spectroscopic properties of a fluorophore?
The performance of a fluorescent probe is defined by several key properties, summarized in the table below [1].
| Property | Definition | Significance in Experimental Design |
|---|---|---|
| Excitation Spectrum | Plot of excitation wavelength vs. number of fluorescence photons generated [1]. | Determines the optimal wavelength of light needed to excite the fluorophore most efficiently [1]. |
| Emission Spectrum | Plot of emission wavelength vs. number of fluorescence photons generated [1]. | Used to select the appropriate emission filter for detection and is the basis for multiplexing different fluorophores [1]. |
| Extinction Coefficient (EC) | Measure of a fluorophore's ability to absorb light at a specific wavelength [1]. | The "brightness" of a fluorophore is proportional to the product of its EC and its Quantum Yield [1]. |
| Fluorescence Quantum Yield (QY) | Ratio of photons emitted to photons absorbed [1]. | A measure of the efficiency of the fluorescence process; a higher QY indicates a brighter probe [1]. |
| Stokes Shift | The energy/wavelength difference between the peak excitation and peak emission [1]. | A larger Stokes shift makes it easier to separate the emission signal from scattered excitation light, reducing background [1]. |
| Photobleaching | The irreversible destruction of a fluorophore upon prolonged exposure to excitation light [1]. | Limits the duration over which a sample can be imaged. Can be mitigated by reducing light exposure and using antifade reagents [2] [3]. |
Troubleshooting Guides & FAQs
Why is my fluorescence signal weak or absent?
Weak or absent signal is a common issue with several potential causes and solutions [2].
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| No or Weak Staining | Primary antibody not validated for the application [2]. | Confirm species reactivity and check supplier data for application validation. Use a positive control [2]. |
| Antibody concentration is too low [2]. | Perform a titration experiment to find the optimal antibody concentration [2]. | |
| Intracellular target not accessible for surface staining [2]. | Check antibody epitope location; perform intracellular staining if the target is inside the cell [2]. | |
| Fluorophore is photobleaching [2]. | Use an antifade mounting medium, reduce light exposure during imaging, and choose photostable dyes (e.g., rhodamine-based) [2] [3]. | |
| Incorrect imaging settings [2]. | Verify that the microscope's excitation and emission filters are correctly set for the dye being used [2]. |
How can I reduce high background or non-specific staining?
Excessive background can obscure specific signals. The following table outlines common remedies [2].
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| High Background | Cell or tissue autofluorescence [2]. | Use an unstained control to assess autofluorescence. Avoid blue fluorescent dyes for low-expression targets, as autofluorescence is high in blue wavelengths. Use autofluorescence quenchers [2]. |
| Non-specific binding of secondary antibody [2]. | Include a secondary-only staining control. Use highly cross-adsorbed secondary antibodies and ensure blocking buffers are compatible (e.g., avoid goat serum when using anti-goat secondaries) [2]. | |
| Antibody concentration is too high [2]. | Titrate the antibody to find a concentration that provides strong specific signal with low background [2]. | |
| Insufficient washing [2]. | Increase the number and volume of washes during the staining procedure [2]. |
What can I do if my fluorescence images are blurry or have uneven illumination?
Image quality issues often relate to the microscope's optical components and setup [3] [4].
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Poor Image Quality | Dirty objective lens [3]. | Clean the lens gently with a lens cleaning cloth and an appropriate solvent (e.g., absolute ethanol), using compressed gas to remove dust first [3]. |
| Coverslip of incorrect thickness [3]. | Use high-quality coverslips with a thickness (e.g., 0.17 mm) matched to the microscope objective's correction [3]. | |
| Vignetting or uneven illumination [4]. | Center and align the light source. Increase the image overlap percentage during slide scanning or use background correction software [4]. | |
| Sample drift or out-of-focus areas [4]. | Allow the microscope to thermally stabilize for at least 2 hours before imaging. Add more focus points to the focus map for slide scanning [4]. | |
| Photobleaching between adjacent tiles [4]. | Optimize tissue preparation for fluorophore stability. Reduce exposure time and illumination intensity where possible [4]. |
How does penetration depth limit fluorescence imaging, and what are the emerging solutions?
The penetration depth of high-resolution fluorescence imaging is fundamentally limited by the scattering and absorption of light by biological tissues [5] [6]. This is a central challenge in preclinical and clinical imaging.
Fundamental Limitation: Tissue scatters light strongly, preventing it from being focused deep within tissue. Consequently, techniques like standard confocal microscopy are limited to superficial depths (sub-millimeter), while techniques that can image deeper (e.g., diffuse optical tomography) suffer from poor spatial resolution (millimeters) [6].
Solutions and Advanced Methodologies:
- Near-Infrared (NIR) Imaging: Light in the near-infrared windows (NIR-I: 650-950 nm; NIR-II: 1000-1700 nm) experiences less scattering and absorption than visible light, allowing for greater penetration and higher resolution at depth [5] [7].
- Protocol Insight: A state-of-the-art approach uses biocompatible quantum dots emitting in the NIR-IIc window (1700-2000 nm) with superconducting single-photon detectors. This setup has enabled non-invasive confocal imaging through an intact mouse head to a depth of ~1,100 μm, allowing single-cell resolution in lymph nodes without surgery [7].
- Ultrasound-Switchable Fluorescence (USF): This technique breaks the acoustic diffraction limit to achieve high resolution in deep tissue.
- Experimental Workflow:
- Contrast Agent Synthesis: Environment-sensitive NIR dyes (e.g., ICG) are encapsulated into thermo-sensitive nanoparticles (e.g., made of PNIPAM polymer) [6].
- Switching Mechanism: A focused ultrasound beam locally heats a tiny volume within the tissue. When the temperature crosses the nanoparticle's lower critical solution temperature (LCST), it undergoes a phase transition, changing the dye's microenvironment and dramatically boosting its fluorescence (switching it "ON") [6].
- Image Acquisition: The ultrasound focus is raster-scanned across the sample. Only the fluorescence from the switched-on voxel is detected, building a high-resolution image point-by-point. This method is not susceptible to dynamic processes in tissue, unlike some other deep-imaging techniques [6].
- Experimental Workflow:
Workflow of Ultrasound-Switchable Fluorescence (USF) imaging.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Genetically Encoded Fluorescent Proteins (e.g., GFP, RFP) | Enable labeling and tracking of specific proteins or structures in live cells through genetic fusion. They are the most common fluorophores for live-cell imaging [8]. |
| Organic Dyes (e.g., Cyanine Dyes, CF Dyes) | Synthetic fluorescent molecules often used for immunostaining, flow cytometry, and in vivo imaging. They offer high brightness and photostability [2] [1]. |
| Near-Infrared II (NIR-II) Dyes and Quantum Dots | Fluorophores emitting in the 1000-1700 nm range. They minimize light scattering and autofluorescence, enabling deep-tissue imaging with high spatial resolution [5] [7]. |
| Antifade Mounting Medium | A reagent used to slow down photobleaching in fixed samples prepared for microscopy, preserving fluorescence signal during prolonged observation [2] [3]. |
| Autofluorescence Quenchers (e.g., TrueBlack) | Used to chemically suppress the intrinsic fluorescence of tissues or cells, thereby improving the signal-to-background ratio in an experiment [2]. |
| Ultrasound-Switchable Contrast Agents | Thermo-sensitive nanoparticles encapsulating a dye (e.g., ICG). Their fluorescence is activated by localized ultrasound heating, facilitating high-resolution imaging deep within tissue [6]. |
| Blocking Buffers | Solutions containing proteins (e.g., BSA) or sera used to cover non-specific binding sites on a sample, reducing background staining in immunofluorescence [2]. |
| Acetylexidonin | Acetylexidonin, MF:C26H34O9, MW:490.5 g/mol |
| 3-Epichromolaenide | [(6Z,10Z)-9-acetyloxy-6,10-dimethyl-3-methylidene-2-oxo-3a,4,5,8,9,11a-hexahydrocyclodeca[b]furan-4-yl] (E)-4-hydroxy-2-methylbut-2-enoate |
FAQs: Understanding Penetration Depth
What are the fundamental optical phenomena that limit penetration depth in tissues? The primary limitations are due to absorption and scattering [9]. Absorption occurs when tissue components like hemoglobin, water, or melanin take up light energy, preventing its deeper propagation [9] [10]. Scattering refers to the deflection of light from its original path by tissue components, causing the light to diffuse and reducing the amount that travels straight into the tissue [9] [11]. These two phenomena work together to attenuate light, and penetration depth is defined as the depth at which the light's intensity inside the material falls to about 37% (1/e) of its original surface value [12].
How does the choice of wavelength affect imaging depth? Tissue absorption and scattering are strongly dependent on wavelength. In general, longer wavelengths in the near-infrared (NIR) region penetrate deeper because key tissue chromophores like hemoglobin and water have lower absorption in these ranges, and scattering is reduced [9] [10]. The table below summarizes how different wavelength windows perform.
| Wavelength Window | Wavelength Range | Key Characteristics & Challenges |
|---|---|---|
| Visible | 400 - 700 nm | High scattering and absorption by hemoglobin and melanin; shallow penetration [9] [10]. |
| NIR-I | 700 - 900 nm | Reduced scattering and absorption compared to visible light; better penetration; used by FDA-approved dyes like ICG [10]. |
| NIR-II | 1000 - 1700 nm | Significantly reduced scattering, absorption, and autofluorescence; enables deepest penetration and highest resolution for in vivo imaging [10]. |
| Water Absorption Peaks | ~970 nm, 1200 nm, 1450 nm | Regions of high absorption by water, which can limit penetration and must be considered when selecting wavelengths [9] [10]. |
What are the observable consequences of absorption and scattering during an experiment? In imaging techniques like Light Sheet Fluorescence Microscopy (LSFM), absorption creates "shadow" or "stripe" artifacts [13]. These appear as dark regions in the image where absorbing structures (e.g., pigmented cells) have blocked the excitation light path or the emitted fluorescence on its way to the detector [13]. More generally, attenuation leads to a dimming of the fluorescence signal, a lower signal-to-noise ratio, and can completely obscure structures located deep within or behind attenuating regions [14] [11].
Besides wavelength selection, what strategies can help overcome depth barriers? Several methodological and computational strategies can mitigate depth limitations:
- Chemical Clearing: Treating tissues with chemical clearing agents reduces scattering by matching the refractive indices of different tissue components [13].
- Multi-View Imaging: Acquiring images from multiple angles and computationally merging them can "see around" absorbing structures that would otherwise cast shadows in a single view [13].
- Computational Attenuation Correction: Techniques like OPTiSPIM use a transmission scan to create a 3D map of the sample's attenuation properties, which is then used to computationally correct the shadows in the fluorescence image [13].
- Advanced Fluorophores: Using bright, photostable fluorophores with high quantum yield in the NIR-II window, such as certain quantum dots or novel organic dyes, provides a stronger signal that is less affected by attenuation [10] [15].
Troubleshooting Guides
Problem: Shadow Artifacts in Thick Samples
Issue: Your fluorescence images of thick or mesoscopic samples (e.g., embryos, cleared tissues) show dark shadows or stripes, making it difficult to see the true fluorescence distribution [13].
Explanation: These shadows are attenuation artifacts caused by absorbing materials (e.g., pigment, densely packed cells) in the sample. They affect both the incoming excitation light and the outgoing emitted light [13].
Solutions:
- Strategy: Multi-view Imaging
- Protocol: Image your sample from at least two opposing angles (e.g., 0° and 180°). For more complex samples, acquire multiple views (e.g., every 90° or 120°). Use computational fusion software to combine these views into a single, artifact-reduced image [13].
- Rationale: A structure that is hidden by a shadow in one view may be fully visible in another. Combining these views provides a more complete picture.
- Strategy: Attenuation Correction with Transmission Data
- Protocol:
- Perform a transmission scan of your sample using Optical Projection Tomography (OPT) to measure the 3D distribution of the attenuation coefficient (α) [13].
- Acquire your standard fluorescence image (e.g., via LSFM).
- For each voxel in your fluorescence image, calculate a correction factor based on the Beer-Lambert law. This involves computing the path integral of the attenuation coefficient from the illumination source to the voxel, and from the voxel to the detector, accounting for the detection cone [13].
- Apply the correction factor to each voxel to generate a corrected fluorescence image.
- Rationale: This method directly measures and computationally reverses the physical effects of absorption.
- Protocol:
Diagram: Troubleshooting shadow artifacts in imaging.
Problem: Inadequate Penetration Depth for Deep-Tissue Imaging
Issue: The fluorescence signal from your target structure is too weak or cannot be detected because it is located deep (e.g., >500 µm) within scattering tissue.
Explanation: The excitation light and emitted fluorescence are severely attenuated by scattering and absorption as they travel through tissue. This is the central "depth barrier" in fluorescence imaging [14] [10].
Solutions:
- Strategy: Shift to NIR-II Imaging
- Protocol:
- Select or synthesize a fluorophore with excitation and emission in the NIR-II window (1000-1700 nm) [10].
- Use an imaging system equipped with lasers and detectors (e.g., InGaAs cameras) sensitive in this wavelength range.
- Adjust your optical filters and objectives to be optimized for NIR-II light.
- Rationale: Scattering of light is reduced at longer wavelengths, and tissue autofluorescence is minimal, resulting in deeper penetration and a higher signal-to-background ratio [10].
- Protocol:
- Strategy: Use Multiphoton Microscopy with SWIR Wavelengths
- Protocol:
- Label your sample with fluorophores having high multiphoton cross-sections, such as quantum dots (QDs) designed for infrared emission [15].
- Use a long-wavelength (e.g., 1300 nm or 1650 nm) short-wave infrared (SWIR) ultrafast laser for excitation in a multiphoton microscope [15].
- For large-area imaging, implement a temporal focusing setup to achieve axial resolution while using SWIR excitation [15].
- Rationale: Longer SWIR wavelengths experience less scattering in tissue. Multiphoton excitation provides inherent optical sectioning, and temporal filling allows parallel imaging of a large plane. QDs provide the high brightness needed for efficient excitation under these conditions [15].
- Protocol:
The Scientist's Toolkit: Essential Reagents & Materials
The following table lists key materials used to address penetration depth challenges in fluorescence imaging research.
| Research Reagent / Material | Primary Function |
|---|---|
| Indocyanine Green (ICG) | An FDA-approved NIR-I fluorescent dye (emission ~900 nm) used for clinical applications like surgical navigation and vascular imaging [14] [10]. |
| NIR-II Organic Dyes | Synthetic fluorescent molecules engineered to emit in the 1000-1700 nm range, offering deeper penetration and reduced scattering compared to visible or NIR-I dyes [10]. |
| Quantum Dots (QDs) | Semiconductor nanoparticles with size-tunable emission, high brightness, and large multiphoton cross-sections. Ideal for deep-tissue imaging with NIR-II or SWIR excitation [15]. |
| Chemical Clearing Agents | Chemicals (e.g., Scale, CUBIC) that render tissues transparent by reducing light scattering, thereby improving penetration and image clarity [13]. |
| BODIPY Dyes | Versatile fluorescent probes with high quantum yields and photostability. Their emission can be tuned across 500-700 nm, and they can be conjugated to targeting moieties for specific imaging [14]. |
| Songoroside A | Songoroside A, MF:C35H56O7, MW:588.8 g/mol |
| Marsformoxide B | Marsformoxide B, MF:C32H50O3, MW:482.7 g/mol |
Understanding Autofluorescence and Its Impact on Penetration Depth
What is autofluorescence and why is it a problem in fluorescence imaging?
Autofluorescence (AF) is the natural emission of light from biological structures when excited with specific wavelengths of light, without the application of any exogenous fluorescent markers [16] [17]. This phenomenon originates from endogenous fluorophores present in tissues and cells, including NAD(P)H, flavins, collagen, elastin, lipofuscins, and aromatic amino acids like tryptophan, tyrosine, and phenylalanine [16] [17].
In the context of fluorescence imaging solutions research, autofluorescence creates a significant problem by reducing signal-to-background ratio, which ultimately limits effective penetration depth and obscures specific signals from targeted fluorophores [18] [19] [20]. When excitation light travels through tissue to reach fluorescent markers at depth, it simultaneously excites autofluorescence throughout the entire optical path. This creates a background "haze" that masks the specific signal of interest [18]. As imaging depth increases, this problem becomes more pronounced because the desired signal from deeper targets undergoes greater attenuation due to both absorption and scattering, while autofluorescence continues to be generated from superficial layers [18] [21].
Table 1: Common Endogenous Fluorophores and Their Spectral Properties
| Fluorophore | Excitation Peak (nm) | Emission Peak (nm) | Primary Biological Location |
|---|---|---|---|
| NAD(P)H | 340 | 450-470 | Cytoplasm, mitochondria |
| Flavins | 450-490 | 520-560 | Mitochondria |
| Collagen | 330-370 | 400-450 | Extracellular matrix |
| Elastin | 350-420 | 420-510 | Extracellular matrix |
| Lipofuscin | 410-470 | 500-695 | Lysosomal deposits |
| Tryptophan | 280 | 300-350 | Proteins |
| Keratin | 700-760 (2-photon) | 445-580 | Epithelial cells, hair [22] |
The relationship between autofluorescence and penetration depth limitations follows an exponential decay pattern, where the detectable specific signal decreases dramatically with depth due to the competing autofluorescence background [18]. Research has demonstrated that without proper management of autofluorescence, the practical penetration depth for fluorescence imaging can be limited to as little as 1-2 mm, whereas with optimized techniques, detection up to 6 mm or more may be achievable [21].
Troubleshooting Guides & FAQs
How can I identify if autofluorescence is affecting my imaging results?
Perform control experiments with unlabeled samples to establish baseline autofluorescence levels [23]. This is the most direct method to identify autofluorescence contributions. Additionally, spectral lambda scanning can help characterize the autofluorescence profile of your specific sample [19]. If you observe signal in channels where no fluorophore should be emitting, or if you notice unexpectedly high background that reduces image contrast, autofluorescence is likely a factor.
Key indicators of autofluorescence problems:
- Signal persists in "no dye" control samples [23]
- High, uniform background across the entire field of view
- Poor signal-to-background ratio despite adequate labeling
- Signal bleed-through in multiple detection channels
- Unusual fluorescence in samples fixed with aldehydes [16]
What are the most effective strategies to reduce autofluorescence in biological samples?
Optimize sample preparation to minimize autofluorescence sources [19] [20]. For live-cell imaging, replace standard culture media with phenol red-free medium or clear buffered saline solutions, as phenol red and other media components can be highly fluorescent [19] [20]. For fixed samples, consider alternatives to aldehyde-based fixatives like formalin and glutaraldehyde, which can generate fluorescent condensation products [19]. Chemical treatments with sodium borohydride or Sudan black B can attenuate existing autofluorescence in stored samples [19].
Strategic fluorophore selection is crucial—choose fluorescent probes with excitation and emission spectra that minimize spectral overlap with your sample's autofluorescence profile [19]. Modern synthetic dyes like Alexa Fluor, Dylight, or Atto dyes are preferable as they tend to be brighter, more stable, and have narrower excitation/emission bands [19]. When possible, select far-red fluorescent dyes because autofluorescence is typically stronger in the blue and green regions of the spectrum [19] [20].
Instrument optimization can significantly reduce autofluorescence impact. Use spectral detection systems to precisely define collection windows that exclude autofluorescence peaks [19]. For systems with white light lasers, fine-tune excitation wavelengths to maximize specific signal while minimizing autofluorescence excitation [19].
How does autofluorescence specifically limit penetration depth in fluorescence imaging?
Autofluorescence limits penetration depth by creating a background floor that obscures weak signals from deeper structures [18] [24]. As excitation light travels to reach fluorophores at depth, it generates autofluorescence throughout the entire optical path. The emitted fluorescence from deep targets must then travel back through tissue, undergoing additional attenuation. The combined effect of signal attenuation and constant autofluorescence background reduces the contrast-to-noise ratio (CNR) for deeper targets [18]. When the CNR falls below a detection threshold of approximately 3, the target becomes undetectable [18].
Table 2: Depth Detection Limits Under Various Conditions
| Condition | Typical Detection Limit | Primary Limiting Factors |
|---|---|---|
| High autofluorescence background | 1-2 mm | Strong superficial AF, absorption by blood |
| Optimized near-infrared imaging | 4-6 mm | Reduced scattering/absorption in NIR [18] [21] |
| Multiple fluorescent sources | 2-3 mm | Signal crosstalk, overlapping emissions [21] |
| Through highly absorbing media (blood) | <1 mm | Strong absorption of visible light [18] |
| Through highly scattering media | 2-4 mm | Loss of signal directionality [18] |
What advanced techniques can help overcome autofluorescence limitations?
Fluorescence Lifetime Imaging (FLIM) can differentiate specific signals from autofluorescence based on their distinct fluorescence decay characteristics, even when their emission spectra overlap [19] [22]. This technique is particularly powerful because while autofluorescence and specific fluorophores may share similar emission spectra, their fluorescence lifetimes (typically on the nanosecond scale) often differ significantly [19].
Multispectral imaging approaches allow mathematical separation of signal components based on their complete spectral signatures rather than single emission peaks [17]. This enables more sophisticated unmixing of specific fluorescence from autofluorescence background.
Two-photon excitation provides inherent optical sectioning and can reduce out-of-focus autofluorescence by limiting excitation to a small focal volume [22]. However, it's important to note that two-photon excitation can also excite additional endogenous fluorophores that aren't accessible with single-photon excitation [22].
Photobleaching of autofluorescence before adding specific fluorophores can be an effective strategy [19]. By exposing samples to high-intensity light prior to imaging, endogenous fluorophores can be selectively bleached, reducing their contribution to background during actual data acquisition.
Experimental Protocols & Methodologies
Protocol 1: Establishing Autofluorescence Baseline and Spectral Profiling
Purpose: To characterize the autofluorescence signature of your specific sample system as a critical first step in addressing penetration depth limitations.
Materials:
- Unlabeled control samples (identical preparation without fluorescent dyes)
- Fluorescence microscope with spectral detection capability
- Identical imaging dishes/media as used in experimental samples
Procedure:
- Prepare unlabeled control samples using identical protocols as experimental samples, omitting only the fluorescent dyes or markers [23].
- Image control samples using the same acquisition settings (exposure time, gain, excitation wavelengths) planned for experimental samples.
- Perform spectral lambda scanning across the entire emission range relevant to your experimental fluorophores [19].
- Document the autofluorescence intensity levels and spectral profile for each sample type.
- Use this baseline to optimize filter sets and detection windows for experimental imaging.
Expected Results: Autofluorescence profiles will vary significantly by tissue type, fixation method, and imaging media. Tissues rich in collagen/elastin typically show strong autofluorescence in the 400-500 nm range [16] [17].
Protocol 2: Fluorophore Titration for Optimal Signal-to-Background Ratio
Purpose: To determine the optimal concentration of fluorescent dyes that maximizes specific signal while minimizing nonspecific background.
Materials:
- Fluorescent dye stock solutions
- Labeled samples
- Wash buffers (e.g., PBS)
Procedure:
- Prepare a dilution series of your fluorescent dye covering concentrations both below and above the manufacturer's recommendation [19] [20].
- Label separate sample aliquots with each concentration using otherwise identical protocols.
- Perform thorough washing (2-3 times with buffered saline) after labeling to remove unbound dye [20].
- Image all samples using identical acquisition parameters.
- Quantify both specific signal intensity and background autofluorescence for each concentration.
Expected Results: There will be an optimal concentration range that maximizes the signal-to-background ratio. Too low concentrations yield weak specific signal; too high concentrations increase nonspecific binding and background [20].
Protocol 3: Chemical Reduction of Autofluorescence in Fixed Samples
Purpose: To reduce existing autofluorescence in stored or fixed samples using chemical treatments.
Materials:
- Fixed tissue samples or cells
- Sodium borohydride solution (1 mg/mL in PBS) or Sudan black B (0.1-0.3% in 70% ethanol)
- Staining containers
- Wash buffers
Procedure:
- After fixation and before immunolabeling, incubate samples with sodium borohydride solution for 10-30 minutes [19].
- Alternatively, treat samples with Sudan black B solution for 20-30 minutes [19].
- Wash samples thoroughly with buffer before proceeding with standard labeling protocols.
- Compare treated samples with untreated controls to assess autofluorescence reduction.
Expected Results: Sodium borohydride specifically reduces aldehyde-induced autofluorescence, while Sudan black B quenches broad-spectrum autofluorescence, particularly from lipofuscin-like pigments [19].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Autofluorescence Management
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Phenol red-free media | Reduces media autofluorescence | Essential for live-cell imaging; contains necessary nutrients without fluorescent pH indicator [19] [20] |
| Sodium borohydride | Chemical reduction of aldehyde-induced AF | Particularly effective for samples fixed with formaldehyde or glutaraldehyde [19] |
| Sudan black B | Broad-spectrum autofluorescence quenching | Effective against lipofuscin and other autofluorescent pigments [19] |
| Far-red fluorescent dyes (e.g., Alexa Fluor 647) | Spectral separation from AF | AF is typically weaker in far-red region; enables deeper penetration [19] [21] |
| Glass-bottom imaging dishes | Reduce substrate autofluorescence | Plastic dishes exhibit strong autofluorescence; glass provides lower background [20] |
| Modern synthetic dyes (Alexa Fluor, Dylight, Atto) | Bright, stable, specific labeling | Narrow emission bands facilitate separation from AF; higher quantum yield improves detection [19] |
| Mounting media with antifade reagents | Preserve fluorescence, reduce bleaching | Prolongs signal stability during extended imaging sessions |
| F9170 | F9170, MF:C100H135N21O22, MW:1983.3 g/mol | Chemical Reagent |
| 2-Ketodoxapram-d4 | 2-Ketodoxapram-d4, MF:C24H28N2O3, MW:396.5 g/mol | Chemical Reagent |
Advanced Methodologies for Depth Resolution
How can I quantitatively characterize my system's depth sensitivity?
Use tissue-simulating optical phantoms with well-characterized materials and fluorescent contrast agents to evaluate imaging system performance [18]. These phantoms incorporate obscuring layers of tissue-mimicking material above a uniform fluorescent layer, allowing systematic quantification of depth detection capabilities.
Depth sensitivity characterization protocol:
- Image tissue-equivalent depth targets under typical operating conditions (working distance, ambient lighting, system settings) [18].
- Measure pixel intensity for each well with varying thickness of scattering/absorbing material above fluorescent layer.
- Plot mean pixel intensity versus tissue-equivalent depth.
- Fit data to an exponential equation to estimate fluorescence signal at any depth.
- Calculate contrast-to-noise ratio (CNR), where CNR ≥ 3 is typically considered the limit of detection [18].
This systematic approach allows researchers to establish the practical penetration depth limits of their specific imaging system and optimize parameters for deep-tissue applications.
FAQs and Troubleshooting Guides
Q1: How can I minimize photobleaching and phototoxicity during live-cell fluorescence imaging?
- Reduce Light Exposure: Use lower light intensities, shorter exposure times, and activate illumination only during image acquisition using fast shutters [25] [26].
- Use Near-Infrared (NIR) Fluorophores: NIR light is less energetic, experiences less scatter and absorption in tissue, and is therefore less damaging to cells and provides better depth penetration [21] [18] [26].
- Employ Antifading Reagents: Add antifading reagents to your mounting medium to slow the photobleaching process [2] [3].
- Choose Stable Dyes: Select photostable fluorescent dyes, such as rhodamine-based dyes, and avoid those known to bleach quickly, like some blue fluorescent dyes [2].
- Utilize Sensitive Detection Systems: Use cameras with high quantum efficiency (QE) and confocal systems designed for fast, low-light imaging to capture sufficient signal with minimal light input [26].
Q2: What are the main causes of low signal-to-noise ratio (SNR) when imaging deep tissues, and how can I improve it?
- Causes: Light is attenuated by absorption (e.g., by blood) and scattering as it travels through tissue, which dims the signal. Autofluorescence and optical system limitations contribute to background noise [21] [2] [18].
- Solutions:
- Optimize Your System: Use high-numerical aperture (NA) objective lenses to gather more light and ensure they are clean and properly corrected. Oil-immersion objectives can minimize light loss [3].
- Increase Signal Generation: Ensure your fluorophore is bright and used at an optimal concentration. For low-expression targets, use signal amplification methods like indirect immunofluorescence or tyramide signal amplification (TSA) [25] [2].
- Suppress Background: Use blocking agents designed for fluorescent applications to reduce non-specific binding. Quench tissue autofluorescence with products like TrueBlack Lipofuscin Autofluorescence Quencher, especially when working in blue wavelengths [2].
Q3: My fluorescence signal is faint or absent. What should I check?
- Confirm Antibody and Dye Validity: Ensure your primary antibody is validated for your specific application (e.g., immunofluorescence) and that it is used at an appropriate concentration. Perform a titration to find the optimal dilution [2].
- Check Target Accessibility: For intracellular targets, confirm that your staining protocol makes the epitope accessible (e.g., through permeabilization). Verify that the antibody binds to an extracellular domain for cell surface staining [2].
- Verify Imaging Settings: Use the correct excitation and emission filters for your dye. Remember that far-red dyes like Alexa Fluor 647 must be detected with a camera and are not visible by eye [2].
- Assess Photobleaching: If the signal was present but faded quickly, your sample may have undergone photobleaching. Implement the strategies listed in Q1 [2] [26].
Q4: How can I characterize my imaging system's depth sensitivity? You can characterize depth sensitivity using tissue-simulating optical phantoms [21] [18]. The general protocol is:
- Acquire Images: Image a phantom with a uniform fluorescent layer buried at progressively deeper levels of tissue-mimicking material under your standard operating conditions [18].
- Measure Intensity: For each depth, measure the mean fluorescence pixel intensity within a region of interest [18].
- Plot and Analyze: Plot the normalized intensity versus depth. The depth at which the signal drops below a detectable level (e.g., where the contrast-to-noise ratio, CNR, falls below 3) is your system's limit of detection [18].
Troubleshooting Common Problems
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| High Background | Tissue autofluorescence | Use autofluorescence quenchers; switch to red/NIR dyes [2]. |
| Non-specific antibody binding | Titrate antibody concentration; use highly cross-adsorbed secondary antibodies [2]. | |
| Insufficient washing | Increase wash frequency and volume [2]. | |
| Photobleaching | Excessive light exposure | Reduce intensity/exposure time; add antifade reagent [2] [26]. |
| Unstable fluorophore | Choose a more photostable dye (e.g., rhodamine-based) [2]. | |
| Low Signal in Deep Tissue | Signal attenuation | Use NIR fluorophores; optimize imaging system sensitivity [21] [18] [26]. |
| Fluorophore concentration too low | Increase concentration if possible; use signal amplification techniques [21] [2]. |
Experimental Protocols
Protocol 1: Characterizing Depth Sensitivity Using Tissue-Mimicking Phantoms This methodology allows you to quantify how well your fluorescence imaging system can detect signals at different depths [21] [18].
Materials:
Procedure: a. Place the phantom at the standard working distance for your imaging system. b. Under typical imaging conditions (e.g., standard exposure time, gain, ambient lighting), acquire fluorescence images of the phantom [18]. c. For each well or region representing a different depth, measure the mean pixel intensity within a central region of interest (ROI) that covers about half the diameter of the well [18]. d. Calculate the Contrast-to-Noise Ratio (CNR) for each depth if required. A CNR of 3 is typically considered the limit of detection [18]. e. Plot the normalized mean intensity (or CNR) versus the depth of the tissue-mimicking material. f. Fit an exponential curve to the data to model signal attenuation and estimate the detection limit for your system [18].
Protocol 2: Optimizing Signal-to-Noise Ratio in Live-Cell Imaging This protocol provides steps to maximize signal while preserving cell health [25] [26].
Materials:
Procedure: a. Minimize Photodamage: * Use the lowest light intensity and shortest exposure time that yield a usable signal. * Utilize a system with "active blanking" to ensure the light source is only on during camera exposure [26]. * Consider using a multi-point scanning confocal system, which distributes light exposure more efficiently than point scanners [26]. b. Maximize Signal Capture: * Use an objective lens with high numerical aperture (NA) and optimal chromatic correction [3]. * For dim samples, use a camera with high QE (>80%) to detect more photons [26]. c. Validate Cell Health: Throughout the experiment, monitor cells for signs of phototoxicity such as membrane blebbing, vacuolation, or cessation of division [25] [26].
Table 1: Optical Properties of Biological Tissues and Phantom Components This table summarizes key parameters that affect light propagation in tissues, as used in experimental phantoms [21].
| Parameter | Description | Typical Range in Brain Tissue [21] | Common Phantom Components [21] |
|---|---|---|---|
| Absorption Coefficient (µa) | Likelihood of light being absorbed per unit distance. | 0.001 to 0.05 mmâ»Â¹ | metHb (methemoglobin) |
| Reduced Scattering Coefficient (µs') | Likelihood of light being scattered per unit distance, accounting for forward direction. | 0.5 to 2.5 mmâ»Â¹ | Intralipid |
| Anisotropy (g) | Measure of forward scattering tendency. | 0.80 to 0.95 [18] | Not typically specified in phantom studies |
Table 2: Depth Estimation Techniques for Fluorescent Inclusions A summary of algorithms for estimating the depth of a fluorescent object based on reflectance and fluorescence measurements [21].
| Technique | Input Parameters | Calculation of Slope (m) for Depth Estimation | Limitations |
|---|---|---|---|
| 1. Diffusion Equation Solution | µa, µs' (optical properties) | ( m = \frac{1}{\delta{\lambda2}} - \frac{1}{\delta{\lambda1}} ) where ( \delta{\lambda} = \sqrt{\frac{D}{\mua}} ), ( D = \frac{1}{3(\mua + \mus')} ) | Requires precise knowledge of optical properties [21]. |
| 2. Empirical Scattering Correction | µs', Diffuse Reflectance (Rd) | ( m = \frac{ \ln \left( \frac{Rd{\lambda1}}{Rd{\lambda2}} \right) }{ \mu_s'(\text{700 nm}) \times 3.28 } ) | Requires knowledge of reduced scattering coefficient [21]. |
| 3. Diffuse Reflectance Correction | Diffuse Reflectance (Rd) only | ( m = \ln \left( \frac{Rd{\lambda1}}{Rd{\lambda2}} \right) ) | Simpler but may be less accurate for some optical properties [21]. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Alexa Fluor 647 (AF647) | A biochemically stable near-infrared fluorescent dye used in phantoms to simulate fluorophores like PpIX due to its similar emission when excited at 635 nm [21]. |
| metHb (Methemoglobin) | A stable form of hemoglobin used in phantoms to simulate the absorption properties of blood in tissue [21]. |
| Intralipid | A fat emulsion used in optical phantoms to simulate the scattering properties of biological tissues [21]. |
| TrueBlack Lipofuscin Autofluorescence Quencher | A reagent used to suppress tissue autofluorescence, a major source of background noise, particularly in formalin-fixed paraffin-embedded (FFPE) tissues [2]. |
| EverBrite Mounting Medium | An antifade mounting medium that helps preserve fluorescence signal and reduce photobleaching during microscopy [2]. |
| Tungsten Halogen Lamp | A broadband white light source used for acquiring diffuse reflectance images, which are necessary for calibrating and correcting fluorescence depth measurements [21]. |
| Liquid Crystal Tunable Filter (LCTF) | A wavelength filter placed in front of a camera that allows for the sequential acquisition of spectral images at specific, narrow wavelength bands [21]. |
| Deferoxamine-DBCO | Deferoxamine-DBCO, MF:C44H61N7O10, MW:848.0 g/mol |
| CTB probe-1 | CTB probe-1, MF:C46H60N10O8S2, MW:945.2 g/mol |
Experimental Workflow and System Diagrams
Systematic Troubleshooting Approach
Depth Sensitivity Characterization Workflow
Multimodal Strategy for Imaging Challenges
Breakthrough Imaging Windows and Advanced Fluorophores for Enhanced Penetration
Troubleshooting Guides
FAQ 1: Why is my in vivo fluorescence signal weak and background high despite using an NIR-I dye?
Problem: Weak target signal and high background autofluorescence in deep-tissue imaging.
Explanation: In the traditional NIR-I window (700–900 nm), photon scattering remains significant, and biological tissues exhibit noticeable autofluorescence. Although superior to visible light, NIR-I penetration depth is practically limited to about 0.2 mm in brain tissue, for instance [27]. Scattering distorts the signal path and reduces the number of ballistic photons that can be collected, while autofluorescence from biomolecules creates a competing background noise.
Solution:
- Transition to NIR-II Imaging: Shift your imaging and detection to the NIR-II window (1000–1700 nm). The reduced photon scattering (scaling with λ-α) and minimal tissue autofluorescence in this region significantly enhance the signal-to-background ratio (SBR) [28] [29].
- Leverage "Off-Peak" Imaging: If your equipment is limited to NIR-I fluorophores like Indocyanine Green (ICG) or IRDye800CW, try detecting their long emission tails in the NIR-II region (e.g., using a 1500 nm long-pass filter). This "off-peak" method can provide some of the benefits of NIR-II imaging with clinically available dyes [29].
- Verify Probe Brightness: Ensure your fluorescent probe has sufficient brightness to overcome the inherent signal attenuation over longer path lengths. For NIR-II, this may require bright inorganic nanomaterials or novel organic dyes with high quantum yields [30] [27].
FAQ 2: My NIR-II fluorescent probes lack target specificity and show poor biocompatibility. How can this be improved?
Problem: Non-specific probe accumulation and potential long-term toxicity.
Explanation: Many high-performance NIR-II probes, particularly inorganic nanomaterials like quantum dots and rare-earth-doped nanoparticles, face challenges in biodegradability and can have potential long-term toxicity [30]. Furthermore, complex synthesis processes can hinder functionalization for specific targeting.
Solution:
- Employ Organic Dyes and Surface Engineering: Utilize organic small-molecule NIR-II dyes (e.g., those with a donor-acceptor-donor (D-A-D) structure), which generally have better renal clearance profiles [29]. For inorganic probes, implement surface modifications with polymers (like PEG) or targeting ligands (e.g., peptides, antibodies) to enhance biocompatibility, improve water solubility, and confer active targeting capabilities [30] [27].
- Develop Activatable Probes: Design "smart" probes that remain fluorescently "off" until they encounter a disease-specific biomarker (e.g., enzymes, pH, reactive oxygen species). This strategy dramatically reduces background signal from non-target tissues and improves imaging specificity [30] [31]. The "off-on-off" probe design is a advanced example that further minimizes background upon probe clearance from normal tissues [31].
FAQ 3: How can I achieve precise imaging of brain tumors considering the blood-brain barrier?
Problem: The blood-brain barrier (BBB) prevents efficient delivery of imaging probes to glioblastoma (GBM) and other brain tumors.
Explanation: The BBB is a major obstacle for diagnostic and therapeutic agents. Conventional probes cannot cross this barrier, leading to poor imaging contrast for brain diseases [27].
Solution:
- Utilize Targeted Nanoplatforms: Develop NIR-II nanoprobes functionalized with ligands that can undergo receptor-mediated transcytosis to cross the BBB [27].
- Multimodal Imaging Guidance: Use NIR-II fluorescence imaging in conjunction with other techniques like MRI to guide and validate the delivery of probes across the BBB [27].
- Explore Passive Targeting: Leverage the Enhanced Permeability and Retention (EPR) effect, which allows nanoparticles of a certain size to accumulate preferentially in tumor tissues due to their leaky vasculature, although this is less effective for intact BBB [32].
Key Experimental Protocols
Protocol 1: NIR-II Fluorescence Imaging for In Vivo Tumor Detection and Photothermal Therapy
This protocol outlines the use of NIR-II AIE dots for imaging-guided photothermal ablation of lesions, such as endometriosis [32].
Workflow Diagram:
Materials:
- NIR-II AIE Dots: Aggregation-induced emission luminogens with emission in 1000-1700 nm [32].
- Animal Disease Model: e.g., murine model of endometriosis or glioblastoma [32] [27].
- NIR-II Imaging System: Includes an 808 nm laser for excitation and an InGaAs camera for detection in the 1000-1700 nm range [32] [28].
- Histology Reagents: Hematoxylin and Eosin (H&E) for post-treatment validation [32].
Step-by-Step Procedure:
- Probe Preparation: Synthesize and characterize AIE dots. Ensure they exhibit high fluorescence brightness in the NIR-II window and a photothermal conversion efficiency sufficient for therapy (e.g., ~40%) [32].
- Animal Administration: Intravenously inject the AIE dots into the animal model via the tail vein.
- Passive Accumulation: Allow sufficient time (e.g., several hours to a day) for the nanoparticles to accumulate at the tumor/lesion site through the Enhanced Permeability and Retention (EPR) effect [32].
- NIR-II Imaging: Anesthetize the animal and position it under the NIR-II imaging system. Excite the probe with an 808 nm laser and collect the emitted fluorescence using the InGaAs camera. Acquire high-resolution images to locate the lesion.
- Photothermal Therapy: Once the lesion is located, increase the power density of the 808 nm laser at the target site. Maintain irradiation until the local temperature reaches the required ablation threshold (e.g., 50°C) for the necessary duration to induce cell death [32].
- Validation: Sacrifice the animal and extract the target tissue. Perform H&E staining and immunofluorescence analysis to confirm the histological reduction of the lesion post-therapy [32].
Protocol 2: Evaluating NIR-II "Off-On-Off" Probes for High-Contrast Molecular Imaging
This protocol details the use of advanced activatable probes for sensitive imaging of early-stage diseases with minimal background [31].
Signaling Pathway Diagram:
Materials:
- "Off-On-Off" Probe (NDP): A naphthalene diimide-based probe that is activated by a specific biomarker (e.g., Hâ‚‚S) and deactivated by another (e.g., ROS) [31].
- NIR-II Excitation Source: 1064 nm laser [31].
- Spectrometer with InGaAs Detector: For measuring the absorption shift and NIR-II emission turn-on/off.
- Orthotopic Liver Tumor Model: Animal model for validating sensitive early cancer detection [31].
Step-by-Step Procedure:
- Probe Validation:
- Zero Initial Fluorescence: Confirm that the NDP probe has near-ideal zero fluorescence upon 1064 nm excitation in a buffer solution.
- Turn-On Response: Incubate the probe with the target biomarker (e.g., Hâ‚‚S). Use spectroscopy to verify a large absorption redshift (e.g., to 1066 nm) and the turn-on of NIR-II fluorescence (e.g., emission at 1138 nm).
- Turn-Off Response: Further incubate the activated probe with the deactivating agent (e.g., ROS). Confirm the fluorescence is quenched, returning to the "off" state.
- In Vivo Imaging:
- Inject the NDP probe into animal models bearing the target disease (e.g., orthotopic liver tumor) and healthy controls.
- Acquire NIR-II fluorescence images over time using 1064 nm excitation.
- Observe fluorescence turning on specifically in the disease tissue and turning off as the probe migrates to normal tissues, resulting in exceptionally low background.
Table 1: Comparison of Near-Infrared Bioimaging Windows
| Parameter | NIR-I Window | NIR-II Window | NIR-IIb/IIx Sub-Window |
|---|---|---|---|
| Wavelength Range | 700–900 nm [29] | 1000–1700 nm [30] [28] | 1500–1700 nm (IIb) [28] / 1400–1500 nm (IIx) [28] |
| Tissue Penetration Depth | ~0.2 mm (in brain tissue) [27] | Up to 3–4 mm [27] [28] | Deeper than broad NIR-II [28] |
| Spatial Resolution | Lower due to higher scattering | Superior, higher resolution [30] [29] | Highest (e.g., FWHM declines with μa) [28] |
| Signal-to-Background Ratio (SBR) | Moderate, affected by autofluorescence | 2–4 fold higher than NIR-I for tumors [29] | Vastly improved contrast [28] |
| Tissue Autofluorescence | Noticeable | Minimal/negligible [27] [29] | Very low [28] |
| Key Fluorophore Examples | ICG, IRDye800CW [29] | CH1055-PEG, AIE Dots, Quantum Dots [30] [29] | PbS/CdS QDs (emitting at ~1450 nm) [28] |
Table 2: Performance Metrics of Different NIR-II Fluorescent Probes
| Probe Type | Example | Key Advantages | Key Limitations | Excretion / Biocompatibility |
|---|---|---|---|---|
| Organic Small Molecules | CH1055-PEG [29] | High renal excretion (>90%), tunable optical properties [29] | Relatively low quantum yield (e.g., 0.03%) [29] | Favorable (renal) [29] |
| Inorganic Nanomaterials | Quantum Dots, Rare-Earth Nanoparticles [30] [27] | High brightness, high photostability, multifunctionality [30] [27] | Poor biodegradability, potential long-term toxicity, liver/spleen accumulation [30] [27] | Unfavorable (hepatic, slow) [30] [27] |
| Aggregation-Induced Emission (AIE) Dots | AIE Luminogen Dots [32] | High brightness, high photostability, good photothermal conversion efficiency (e.g., 40%) [32] | Complex synthesis, need for surface modification [30] | Can be engineered for improved biocompatibility [32] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for NIR Fluorescence Imaging Experiments
| Item Name | Function / Application | Key Characteristics |
|---|---|---|
| Indocyanine Green (ICG) | FDA-approved NIR-I dye for clinical angiography; can be used for its NIR-II emission tail [29]. | Absorption: ~805 nm; Emission: ~830 nm (peak) with a long tail to >1500 nm [29]. |
| Donor-Acceptor-Donor (D-A-D) Dyes | Organic NIR-II small molecule fluorophores (e.g., CH1055) [29]. | Systematic molecular tuning, emission at 900-1600 nm, potential for high renal excretion [29]. |
| PbS/CdS Core-Shell Quantum Dots (CSQDs) | Bright, wavelength-tunable inorganic probes for high-performance NIR-II imaging [28]. | Size-tunable emission (e.g., 1100–1450 nm), high quantum yield, PEG coating for hydration [28]. |
| AIE Luminogen (AIEgen) Dots | Nanoparticles for NIR-II imaging and photothermal therapy [32]. | High brightness in aggregated state, high photostability, high photothermal conversion efficiency [32]. |
| "Off-On-Off" Probes (e.g., NDP) | Activatable molecular probes for ultra-sensitive imaging with minimal background [31]. | Near-ideal zero initial fluorescence, ultra-high turn-on/off ratio, biomarker-responsive (e.g., Hâ‚‚S) [31]. |
| InGaAs Camera | Essential detector for NIR-II and SWIR light. | Sensitive in the 900-1700 nm range (standard) or beyond (up to 2500 nm for advanced systems) [28]. |
| 16,17-EDT | 16,17-EDT, MF:C22H36O3, MW:348.5 g/mol | Chemical Reagent |
| Carmichaenine A | Carmichaenine A, MF:C31H43NO7, MW:541.7 g/mol | Chemical Reagent |
Troubleshooting Common NIR-II Experimental Challenges
This guide addresses specific technical issues you might encounter during NIR-II fluorescence imaging experiments, providing targeted solutions to ensure data quality and experimental success.
FAQ 1: My NIR-II fluorescence signal is unexpectedly weak. What are the primary causes and solutions?
A weak signal can stem from the fluorophore itself or the imaging setup. The table below outlines common causes and corrective actions.
| Primary Cause | Root Issue | Corrective Action |
|---|---|---|
| Low Fluorophore Quantum Yield | Innately low radiative transition efficiency in NIR-II window [10]. | Select fluorophores with S-D-A-D-S molecular design or AIEgens to reduce aggregation-caused quenching [33] [34]. |
| Environmental Quenching | Interaction with water molecules increases non-radiative decay [33]. | Encapsulate organic dyes in nanoparticles or serum albumin to shield from aqueous environment [10]. |
| Insufficient Excitation Power | Power density is too low to generate sufficient fluorescence. | Increase laser power within safe limits for living tissue (typically <100 mW/cm² for in vivo studies). |
| Suboptimal Imaging Setup | Use of inappropriate filters or detector inefficiency. | Confirm long-pass emission filter cutoff and ensure InGaAs detector is optimized for 1000-1700 nm range [35] [36]. |
FAQ 2: How can I differentiate between specific and non-specific fluorescence signals in deep tissue?
Non-specific signals can be addressed through probe design and advanced imaging techniques.
| Challenge | Solution | Experimental Implementation |
|---|---|---|
| High Background Signal | Use brighter probes and target-specific ligands. | Conjugate targeting moieties (e.g., peptides, antibodies) to fluorophores; employ conjugated polymers for higher brightness [33] [37]. |
| Unclear Signal Origin | Leverage lifetime imaging. | Use time-gated detection or TCSPC to measure luminescence lifetime, which is concentration-independent and discriminates against autofluorescence [38]. |
FAQ 3: My NIR-II probe shows poor biocompatibility or cellular toxicity. How can this be mitigated?
Biocompatibility is closely tied to a probe's physicochemical properties and clearance pathway.
| Observation | Potential Cause | Mitigation Strategy |
|---|---|---|
| Acute Toxicity | Cytotoxicity from probe materials (e.g., heavy metals in QDs). | Prioritize organic small molecules or rare-earth nanoparticles with low toxicity profiles [33] [39]. |
| Chronic Toxicity / Long-term Retention | Slow bodily clearance, leading to organ accumulation. | Design small hydrodynamic diameter (<6 nm) probes for rapid renal clearance [39]. Apply hydrophilic PEG coatings to reduce MPS uptake [39]. |
Essential Experimental Protocols
Protocol 1: Rationally Designing an Organic Small Molecule NIR-II Fluorophore
This protocol outlines the synthesis of high-performance organic NIR-II fluorophores based on established molecular engineering principles [33] [10] [34].
Key Reagents:
- Donor (D) Units: Strong electron-donating groups (e.g., triphenylamine, phenothiazine).
- Acceptor (A) Units: Strong electron-accepting groups (e.g., benzobisthiadiazole, thienothiadiazole).
- Shielding (S) Units: Bulky, twisted groups (e.g., bulky alkyl chains, xylyl) to reduce intermolecular interactions.
Methodology:
- Scaffold Selection: Construct a D-A-D or S-D-A-D-S molecular backbone. The S-D-A-D-S structure is superior for suppressing fluorescence quenching in aqueous environments [33].
- Energy Level Tuning: Adjust the intramolecular charge transfer (ICT) strength by modifying the electron-donating/accepting capabilities of D and A units. A stronger ICT leads to a longer emission wavelength [10].
- Aggregation Control: For NIR-II Aggregation-Induced Emission Luminogens (AIEgens), introduce molecular rotors/vibrons into a D–A–D–A–D–A–D scaffold. This creates an AIE–ACQ–AIE architecture that balances brightness and redshift [34].
- Water Solubilization: Covalently link hydrophilic polymers (e.g., PEG) or sulfonate groups to the conjugated skeleton to ensure biocompatibility and facilitate renal clearance [39].
Protocol 2: Conducting a High-Contrast In Vivo NIR-II Angiography
This procedure details the steps for visualizing blood vessels with high spatial resolution in live animals [35] [36].
Key Reagents:
- NIR-II Fluorophore: IR-1048 dye, Ag2S Quantum Dots, or organic dye-loaded nanoparticles (e.g., MTBTMT-BBT NPs [34]).
- Anesthesia: Isoflurane or ketamine/xylazine mixture.
- Physiological Saline: For probe dilution and injection.
Methodology:
- Probe Preparation: Dilute the NIR-II fluorophore in sterile physiological saline to a working concentration (e.g., 100-500 µM). Filter the solution through a 0.22 µm membrane.
- Animal Preparation: Anesthetize the animal and secure it on a heated imaging stage to maintain body temperature. Remove hair from the imaging area as needed.
- System Setup: Use a preclinical NIR-II imaging system (e.g., IR VIVO) with an InGaAs camera. Set excitation laser to 808 nm or 1064 nm and place a long-pass emission filter (e.g., LP1250 or LP1500) appropriate for the probe's emission [35].
- Image Acquisition:
- Acquate a baseline image before injection.
- Intravenously inject the probe solution via the tail vein.
- Start continuous image acquisition immediately post-injection. Use short exposure times (e.g., 20-100 ms) to capture dynamic blood flow.
- Data Analysis: Use region-of-interest (ROI) analysis to calculate signal-to-background ratios (SBR) and generate time-intensity curves for hemodynamic analysis.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogs essential materials used in advanced NIR-II experiments, along with their critical functions.
| Research Reagent | Category | Primary Function & Application Notes |
|---|---|---|
| CH1055-PEG | Organic Small Molecule | First reported D-A-D structured NIR-II dye; used for tumor-targeted molecular imaging when conjugated to antibodies (e.g., anti-EGFR) [33]. |
| IR-BEMC6P@RGD | Targeted Organic Probe | S-D-A-D-S structured probe with high quantum yield; RGD peptide conjugation enables specific imaging of integrin-positive tumors [33]. |
| Ag2S Quantum Dots (QDs) | Inorganic Nanoparticle | Low-toxicity inorganic option; used in dual-modal probes (e.g., Gd-DOTA-Ag2S QDs) for MRI and NIR-II image-guided surgery [37]. |
| CC-LnNPs | Biomimetic Nanoprobes | Lanthanide-doped nanoparticles coated with a brain tumour cell membrane; enables immune escape and homologous targeting for precise glioma imaging and resection [37]. |
| MTBTMT-BBT NPs | AIEgen Nanoparticles | Multidimensional engineered fluorophore for dual NIR-II imaging and photothermal therapy (57.9% PCE); excitable at 808, 980, and 1064 nm [34]. |
| ICG (Indocyanine Green) | Clinical NIR-I/II Dye | FDA-approved dye with a fluorescence tail in NIR-II; serves as a benchmark; modified versions (e.g., 64Cu DOTA-FA-ICG) used for NIR-II guided surgery [37] [35]. |
| Dazdotuftide | Dazdotuftide | TRS01 Immunomodulator Research Compound | |
| Anticancer agent 58 | Anticancer agent 58, MF:C39H55NO5, MW:617.9 g/mol | Chemical Reagent |
Workflow and Signaling Pathway Visualizations
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What are the primary factors that limit penetration depth in fluorescence imaging, and how can probe selection help overcome them? The primary factors are tissue absorption and scattering of light. Different tissue components, or chromophores, absorb light, while scattering occurs when light changes direction after bouncing off tissue structures [18]. Selecting probes that emit in the Near-Infrared (NIR) windows, particularly NIR-II (1000-1700 nm) and NIR-IIb (1500-1700 nm), is a key strategy. In these windows, light experiences significantly less absorption and scattering from biological tissues, enabling deeper penetration and higher-resolution imaging [18] [40].
Q2: My fluorescent signal is too weak for detection through tissue. What should I check? First, verify the fundamental properties of your probe and system:
- Emission Wavelength: Ensure your probe emits in the NIR-I or NIR-II region. Visible light probes (e.g., blue, green) are heavily attenuated by tissue [18].
- Probe Brightness: Check the quantum yield (QY) of your probe. A higher QY indicates a brighter probe. For example, some AIEgens are engineered to maintain a QY of over 11% even in the NIR-II region, which is exceptional for organic dyes [40].
- System Settings: Confirm that your imaging system's excitation source and camera are optimized for the excitation and emission wavelengths of your probe [18] [2].
Q3: I am using an organic dye, but its fluorescence is quenched when it aggregates in aqueous solution. How can I prevent this? This is a classic case of Aggregation-Caused Quenching (ACQ). Consider switching to probes based on Aggregation-Induced Emission Luminogens (AIEgens). Unlike conventional dyes, AIEgens are non-emissive in solution but become highly fluorescent in their aggregated state due to the restriction of intramolecular motion, making them ideal for forming bright nanoparticles for bioimaging [40].
Q4: I am getting high background noise during in vivo imaging. What could be the cause? High background is often due to tissue autofluorescence, where native tissue components emit light, typically in the blue-green spectrum [2] [41]. To minimize this:
- Use NIR-II Probes: Autofluorescence is significantly reduced in the NIR-II window, leading to a much higher signal-to-background ratio [40].
- Employ Quenchers: Use commercial autofluorescence quenchers if you are stuck working in the visible spectrum [2].
- Check Probe Specificity: Ensure your probe is effectively targeting the area of interest and not binding non-specifically [41].
Troubleshooting Guide
| Problem | Potential Cause | Solution |
|---|---|---|
| No or Weak Signal | Probe emission wavelength is in the visible spectrum. | Switch to a NIR-emitting probe (e.g., NIR-II AIEgen or cyanine dye) [18] [40]. |
| The probe's quantum yield is too low for deep-tissue detection. | Use a brighter probe with a higher QY (e.g., Carbon Quantum Dots or high-QY AIEgens) [42] [40]. | |
| Probe concentration is too low. | Perform a titration experiment to determine the optimal concentration for your application [2]. | |
| High Background Noise | Tissue autofluorescence. | Image in the NIR-IIb (1500-1700 nm) window where autofluorescence is nearly zero [40]. |
| Non-specific binding of the probe. | Functionalize the probe with targeting ligands (e.g., antibodies, peptides) for specific accumulation [41]. | |
| Signal Quenching in Water | Aggregation-Caused Quenching (ACQ) of conventional organic dyes. | Use probes with inherent AIE properties that turn on upon aggregation [40]. |
| Poor Photostability | Fluorophore is being degraded by the excitation light (photobleaching). | Use mounting media with antifade reagents or choose more photostable dyes (e.g., rhodamine-based dyes or Carbon Dots) [2] [42]. |
| Inability to Resolve Deep Targets | Excessive light scattering at the imaging wavelength. | Utilize probes with longer emission wavelengths (e.g., NIR-II/J-aggregate BODIPY) to reduce scattering [21] [43]. |
Quantitative Data and Probe Performance
The following table summarizes key performance metrics for various next-generation fluorescence probes, which are critical for selecting the right agent to overcome penetration depth limitations.
Table 1: Comparison of Next-Generation Fluorescence Imaging Probes
| Probe Category | Examples | Typical Emission Range | Key Advantages | Documented Penetration Depth / Application |
|---|---|---|---|---|
| Organic Dyes (Cyanines) | ICG, Cy7 [44] | NIR-I (∼800 nm) | FDA-approved (ICG), high absorption coefficients [44]. | Widely used for clinical imaging and angiography. |
| BODIPY Dyes | PCP-BDP2 J-aggregates [43] | NIR-II (1010 nm) | Tunable structure, high stability; J-aggregates enable NIR-II emission [43]. | Lymph node imaging and guided surgery in mice [43]. |
| AIEgens | 2TT-oC26B nanoparticles [40] | NIR-II up to 1600 nm | Bright in aggregate state (AIE), high QY (11.5%), low background [40]. | High-resolution imaging of blood vessels and deeply-located intestinal tract in live mice [40]. |
| Carbon-Based Nanomaterials | Carbon Quantum Dots (CQDs) [45] [42] | Tunable, visible to NIR | Biocompatibility, low toxicity, ease of functionalization [45] [42]. | Used for bioimaging, drug delivery, and phototherapy [42]. |
| Inorganic Nanomaterials | Quantum Dots, Rare-Earth Nanoparticles [40] | NIR-II & NIR-IIb | High brightness, photostability [40]. | Deep-tissue and tumor imaging with high resolution [40]. |
Essential Experimental Protocols
Protocol 1: Characterizing Imaging System Depth Sensitivity Using Tissue-Mimicking Phantoms
This protocol is essential for quantitatively evaluating the performance of any fluorescence imaging system and probe combination for deep-tissue applications [18].
Materials Needed:
- Fluorescence imaging system
- Tissue-mimicking depth sensitivity reference target (e.g., phantom with wells of varying depths above a fluorescent layer)
- Standardized fluorescent solution (e.g., ICG)
Methodology:
- Image Acquisition: Using your fluorescence imaging system, capture an image of the depth target under standard clinical conditions (e.g., typical working distance, ambient lighting, and system settings) [18].
- Intensity Measurement: For each well in the phantom, measure the mean pixel intensity within a region of interest (ROI) that covers about half the diameter of the well. This can be automated with analysis software [18].
- Data Analysis & Plotting: Plot the measured mean pixel intensity (or the Contrast-to-Noise Ratio, CNR) against the known tissue-equivalent depth of each well [18].
- Fit and Interpret: Fit the data to an exponential decay equation. The depth at which the CNR drops below a threshold (commonly 3) is considered the system's limit of detection for that specific probe and tissue type [18].
This advanced protocol allows for depth estimation of fluorescent targets in turbid media [21].
Materials Needed:
- sCMOS camera with a liquid crystal tunable filter (LCTF)
- Broadband white light source (e.g., tungsten halogen lamp) for reflectance.
- Diode laser for fluorescence excitation (e.g., 635 nm for AF647 dye).
- Tissue-simulating phantoms with embedded fluorescent inclusions.
Methodology:
- Dual-Modality Image Acquisition:
- Calculate Dual-Wavelength Fluorescence Ratio (DWFR): For each pixel, calculate the ratio of fluorescence intensities at two carefully selected wavelengths (e.g., 670 nm and 700 nm) [21].
- Depth Estimation: Use a pre-calibrated linear relationship between the DWFR and the fluorophore depth to convert the ratio values into a depth map. This technique can resolve fluorescent sources up to 6 mm deep, even when multiple sources are present [21].
Research Reagent Solutions
Table 2: Essential Reagents and Materials for Deep-Tissue Fluorescence Imaging Research
| Item | Function in Research |
|---|---|
| Tissue-Mimicking Phantoms | Contains materials with well-characterized absorption (μa) and reduced scattering (μs') coefficients to simulate human tissue for standardized system testing and validation [18] [21]. |
| Indocyanine Green (ICG) | An FDA-approved NIR-I cyanine dye used as a clinical benchmark and for validating new imaging systems and surgical guidance protocols [44]. |
| NIR-II AIEgen Nanoparticles | Organic nanoparticles (e.g., based on 2TT-oC26B) that provide bright, red-shifted emission for high-resolution, deep-tissue imaging with minimal background [40]. |
| J-Aggregating BODIPY Dyes | BODIPY dyes (e.g., PCP-BDP2) engineered to form J-aggregates, which shift emission into the NIR-II window for applications like lymph node mapping [43]. |
| Carbon Quantum Dots (CQDs) | Biocompatible, low-toxicity nanoprobes used for bioimaging, sensing, and drug delivery, often with tunable emission wavelengths [45] [42]. |
| TrueBlack Lipofuscin Autofluorescence Quencher | A commercial reagent used to suppress tissue autofluorescence, a major source of background noise, particularly in the visible light spectrum [2]. |
Signaling Pathways and Experimental Workflows
Diagram: Molecular Design Logic for NIR-IIb AIEgens
Diagram: Workflow for Depth Sensitivity Characterization
Frequently Asked Questions (FAQs) & Troubleshooting Guides
General Questions on FDA-Approved Fluorescent Probes
Q1: What are the key FDA-approved fluorescent agents for clinical imaging? Currently, the primary FDA-approved fluorescent agents for clinical imaging are Indocyanine Green (ICG), Methylene Blue (MB), and 5-Aminolevulinic Acid (5-ALA) [46] [47].
Q2: What are the main advantages of optical imaging over other modalities like PET? Optical imaging is non-invasive and does not involve ionizing radiation, making it safer for patients. It also offers the potential for real-time imaging and provides high molecular sensitivity, which can assist in clinical decision-making [46].
Q3: Why is penetration depth a significant limitation in fluorescence imaging? Biological tissues scatter and absorb light. Components like hemoglobin, water, and lipids absorb photons, which reduces the light that can penetrate deeply and return to the detector, thus limiting effective imaging depth [46] [10].
Technical and Experimental Troubleshooting
Q1: The fluorescence signal in my clinical image is weak or has poor contrast. What could be the cause? This is a common challenge in clinical translation. Potential causes and solutions include [46] [2] [48]:
- Cause: The fluorophore's emission wavelength is in the visible spectrum, where tissue autofluorescence and light absorption are high.
- Solution: Utilize fluorophores that emit in the Near-Infrared (NIR) windows (e.g., NIR-I: 700-900 nm; NIR-II: 1000-1700 nm) where tissue autofluorescence is minimal, and penetration is deeper [46] [10]. ICG, which emits around 820-840 nm, is a prime example [46].
- Cause: Photobleaching of the fluorophore during imaging.
- Solution: Ensure your imaging device uses appropriate light intensity and exposure times. Using highly photostable fluorescent scaffolds (e.g., BODIPYs) can also help, though these are largely still in preclinical stages [46] [14].
- Cause: High background signal from non-specific binding or tissue autofluorescence.
- Solution: For tissue samples, include an unstained control to gauge autofluorescence levels. Using autofluorescence quenchers can also improve the signal-to-background ratio [2].
Q2: Why do only a few targeted fluorescent probes achieve clinical translation? The translation of molecular optical agents to the clinic is challenging due to three interconnected areas [46]:
- Fluorophore Development: It is difficult to develop molecular fluorophores with long-wavelength emission, high brightness, and limited photobleaching. Most clinical imaging devices are designed for the wavelengths of ICG [46].
- Biological Target Selection: The target must be selectively associated with the disease and expressed at a high enough level to generate sufficient contrast. Common targets are cancer-associated surface receptors and enzymes [46].
- Hardware and Software: Clinical imaging devices must be sensitive, compatible with NIR wavelengths, and have ergonomic designs for use in operating rooms or clinics [46].
Q3: How can I improve the specificity of a fluorescent probe for my target? Nonspecific agents like ICG rely on the Enhanced Permeability and Retention (EPR) effect for accumulation in tumors. To increase specificity, research focuses on ligand-based targeting strategies. This involves conjugating fluorophores to targeting moieties like peptides (e.g., EMI-137 targeting c-MET), antibodies (e.g., cetuximab-IRDye800CW), or vitamins (e.g., OTL38 targeting the folate receptor) [46] [47].
Comparison of Key FDA-Approved Fluorescent Probes
The table below summarizes the critical characteristics of the main FDA-approved fluorescent imaging agents [46] [47] [49].
Table 1: Summary of FDA-Approved Fluorescent Probes for Clinical Imaging
| Imaging Agent | Excitation/Emission (nm) | Primary Mechanism | Key Clinical Applications | Reported Limitations |
|---|---|---|---|---|
| Indocyanine Green (ICG) | Exc: ~780 nmEm: ~820 nm [46] | Nonspecific; accumulates via the Enhanced Permeability and Retention (EPR) effect; based on blood supply and lymphatic drainage [46] [49]. | Sentinel lymph node mapping [46]; evaluation of tissue perfusion (e.g., gastric conduit after esophagectomy) [49]; imaging of bullous lesions and the thoracic duct [49]. | Nonspecific; insufficient for high signal-to-background ratios in some tumors [46]. |
| 5-Aminolevulinic Acid (5-ALA) | Exc: 405 nmEm: 635 nm (as PpIX) [47] | Metabolic precursor to fluorescent Protoporphyrin IX (PpIX); accumulates in glioma cells due to reduced ferrochelatase activity [47]. | Visualization and resection of high-grade gliomas (WHO Grade III/IV) [47]. | Limited to surfaces due to visible light emission; less effective in low-grade gliomas [47]. |
| Methylene Blue (MB) | Exc: ~665 nmEm: ~685 nm [46] | Nonspecific; can accumulate in certain tumor types. | Identification of small intestine neuroendocrine tumors (SI-NETs) [46]. | Emission in visible spectrum limits penetration depth and contrast [46]. |
Experimental Protocols & Workflows
Protocol: Intraoperative Fluorescence-Guided Tumor Resection using 5-ALA
This protocol is standard for the resection of high-grade gliomas [47].
- Objective: To achieve real-time visualization and improved resection of malignant glioma tissue.
- Materials:
- 5-ALA hydrochloride (commercially available formulation)
- A neurosurgical microscope equipped with a blue light source (~405 nm) and appropriate filters for detecting red fluorescence (~635 nm)
- Procedure:
- Administration: Approximately 3 hours before induction of anesthesia, administer 20 mg per kg of body weight of 5-ALA orally to the patient [47].
- Metabolic Conversion: Endogenous enzymes in the tumor cells convert 5-ALA into the fluorescent compound Protoporphyrin IX (PpIX). Due to reduced levels of the enzyme ferrochelatase in glioma cells, PpIX accumulates and cannot be efficiently converted to non-fluorescent haem [47].
- Intraoperative Imaging: During craniotomy, illuminate the surgical field with blue light (~405 nm).
- Tumor Visualization: Viable tumor tissue will display strong red fluorescence (emission at ~635 nm), while healthy brain tissue will appear blue. This allows the surgeon to delineate tumor margins and identify residual disease [47].
Protocol: Assessing Tissue Perfusion with Indocyanine Green (ICG)
This protocol is commonly used in surgeries, such as esophagectomy with gastric tube reconstruction, to assess blood flow and reduce anastomotic leak risk [49].
- Objective: To intraoperatively evaluate blood perfusion in reconstructed tissue.
- Materials:
- Procedure:
- Reconstitution: Prepare ICG solution according to the manufacturer's instructions.
- System Setup: Ensure the NIR imaging system is calibrated and positioned over the surgical field (e.g., the gastric conduit).
- ICG Injection: Inject a bolus of ICG (dose as per institutional protocol) intravenously.
- Real-Time Imaging: Observe the surgical field through the NIR imaging system. Well-perfused tissue will show a rapid inflow and washout of ICG fluorescence.
- Assessment: Poorly perfused or ischemic tissue will show delayed inflow, delayed outflow, or no fluorescence, indicating compromised blood supply. This information can guide the surgeon to resect non-viable tissue before anastomosis [49].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for Fluorescence Imaging Research
| Item | Function/Description | Examples/Categories |
|---|---|---|
| Fluorescent Dyes & Probes | Emit light upon excitation; the core of fluorescence imaging. | Clinical: ICG, MB, 5-ALA [46]. Preclinical: BODIPY (high quantum yield), Cyanine dyes (Cy5, Cy7), Alexa Fluor dyes [14]. |
| Targeting Moieties | Enhances probe specificity by binding to disease-specific biomarkers. | Peptides (e.g., c-MET binding peptide in EMI-137) [47], antibodies (e.g., cetuximab) [46], vitamins (e.g., folate in OTL38) [47]. |
| Imaging Systems & Hardware | Devices for exciting fluorophores and detecting emitted light. | Standalone systems, hand-held devices, and goggles for surgeons; systems must be sensitive and compatible with NIR wavelengths [46]. |
| Contrast Agents for OCT | Enhances visualization of specific tissues and microvascular structures in optical coherence tomography. | ICG, Methylene Blue, fluorescein sodium, gold nanoparticles (AuNPs) [14]. |
| Antitumor agent-56 | Antitumor agent-56, MF:C28H28N2O10S, MW:584.6 g/mol | Chemical Reagent |
| mGluR2 modulator 3 | mGluR2 Modulator 3 | Explore mGluR2 Modulator 3, a key compound for studying neurological disorders like schizophrenia and depression. For research use only. Not for human consumption. |
Fluorescence-guided surgery (FGS) is an innovative and rapidly expanding field in modern surgical practice. It adds a critical new dimension to the surgeon's ability to perceive anatomy, physiology, and pathology by making the invisible visible [50]. This technique employs near-infrared (NIR) fluorescent contrast agents and compatible imaging systems to provide real-time intraoperative guidance beyond the capabilities of the human eye alone [51] [50].
The core principle involves a fluorescent probe that absorbs light at one wavelength and emits it at a longer, near-infrared wavelength. A dedicated camera system captures this fluorescence and overlays it onto the standard white-light view of the surgical field [52] [50]. FGS is particularly valuable in surgical oncology, where its primary applications include tissue perfusion assessment, lymph node mapping, visualization of vital anatomical structures like bile ducts and ureters, and most notably, tumor margin delineation [50]. By providing real-time, visual feedback on the location of cancerous tissue, FGS holds the promise of enabling more complete tumor resections while sparing healthy tissue, which can directly improve patient outcomes [51] [53].
Technical FAQs and Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: What are the primary clinical applications of Fluorescence-Guided Surgery? FGS has four well-established indications [50]:
- Tissue Perfusion Assessment: Visualizing blood flow and tissue viability in real-time, crucial for assessing anastomotic perfusion in procedures like colorectal surgery [50].
- Lymph Node Assessment: Mapping the lymphatic system for cancer staging, particularly in cancers like breast cancer and melanoma [50].
- Anatomic Structure Identification: Illuminating vital structures such as the extrahepatic bile ducts during cholecystectomy and the ureters during pelvic surgery to prevent iatrogenic injury [50].
- Tumor Tissue Imaging: Delineating malignant tissue from healthy tissue to guide complete surgical resections, which is the focus of this article [53] [50].
Q2: What is the "tumor-to-background ratio" (TBR) and why is it critical? The Tumor-to-Background Ratio (TBR) is a quantitative measure of fluorescence contrast. It is calculated by dividing the fluorescence intensity of the tumor by the fluorescence intensity of the surrounding normal tissue [53]. A TBR greater than 2.0 is often considered a robust indicator of sufficient contrast to guide surgical resections effectively [53]. A low TBR can lead to false positives or an inability to distinguish the tumor margin clearly.
Q3: Can an imaging device designed for one fluorophore be used with another? Yes, this strategy, known as "repurposing," can be a viable and efficient path to clinical translation. If a new fluorophore has excitation and emission spectra that overlap with the optical range of an already approved device, it can often be successfully imaged [53]. For example, the LUNA system (designed for indocyanine green) was successfully repurposed to image cetuximab-IRDye800CW due to spectral overlap. This approach can save significant time and cost associated with developing and gaining regulatory approval for a new device [53].
Q4: What are the main limitations of current FGS technology? Despite its promise, FGS faces several technical challenges [52]:
- Penetration Depth: Light scatter and absorption in tissue limit effective imaging to superficial depths (typically a few centimeters) [51] [52].
- Background Autofluorescence: Natural fluorescence from tissues can create a high background, reducing the signal-to-noise ratio [2] [52].
- Photobleaching: Fluorophores can lose their ability to fluoresce after prolonged exposure to excitation light [52] [48].
- Quantification Challenges: Fluorescence intensity is influenced by factors like camera distance and angle, making absolute quantification difficult without standardization [50].
Troubleshooting Common Experimental and Clinical Problems
Problem: Weak or Dark Fluorescence Signal
A dim signal can prevent accurate margin assessment. The causes and solutions are often related to the equipment and agent used.
- Potential Cause 1: Suboptimal camera settings or type.
- Solution: Use a cooled CCD monochrome camera for high-sensitivity observations with low noise [48]. Adjust brightness settings by increasing exposure time (while being mindful of increased dark current noise) or using binning (which increases signal at the cost of resolution). Avoid using only the gain setting, as it amplifies noise along with the signal [48].
- Potential Cause 2: Mismatch between filter set and fluorophore.
- Solution: Verify that the excitation and emission spectra of your fluorophore significantly overlap with the bandpass of your microscope's or imaging system's filters. Check the manufacturer's spectral data for both [48].
- Potential Cause 3: Inappropriate agent dose or timing.
- Solution: The timing between agent administration and imaging is critical. For tumor targeting agents, peak fluorescence contrast (TBR) may be achieved hours or days after injection. Perform pilot studies to establish the optimal dose and imaging time window for your specific agent [53].
Problem: High Background or Non-Specific Staining
High background fluorescence obscures the specific signal from the target, making margin delineation difficult.
- Potential Cause 1: Tissue autofluorescence.
- Potential Cause 2: Non-specific binding of the fluorescent agent.
- Solution: Optimize the dosage of the targeting agent (e.g., antibody conjugate). Titrate the antibody concentration to find a level that maximizes specific signal while minimizing background [2]. For complex experiments, consider "paired-agent" methods that use a control, non-targeted agent to normalize for non-specific uptake [51].
Problem: Photobleaching During Imaging
The fluorescent signal fades during prolonged observation, limiting the time available for surgery.
- Potential Cause: Excessive excitation light intensity or duration.
- Solution: Reduce the intensity of the excitation light source to the minimum required to obtain a clear signal [48]. For microscopy, use mounting media with antifade compounds. When selecting dyes, choose photostable varieties (e.g., rhodamine-based dyes) for applications requiring prolonged imaging [2].
Quantitative Data and Performance Metrics
The performance of FGS systems and contrast agents is quantified using specific metrics. The following table summarizes key quantitative findings from clinical and pre-clinical studies.
Table 1: Quantitative Performance Metrics in Fluorescence-Guided Surgery
| Metric | Description | Reported Value / Range | Context & Technique |
|---|---|---|---|
| Detection Sensitivity [54] | Minimum moles of contrast agent detectable | ~100 femtomoles (fmol) | Frequency-domain photon migration (FDPM) imaging of ICG at 3 cm depth in tissue-simulating phantom [54]. |
| Tumor-to-Background Ratio (TBR) [53] | Fluorescence intensity ratio of tumor to normal tissue | 2.2 – 14.1 (Peak TBR >2.0) | Intraoperative imaging of head and neck squamous cell carcinoma using a repurposed LUNA system and cetuximab-IRDye800CW [53]. |
| Optimal Imaging Time [53] | Time post-injection for peak fluorescence contrast | Greatest TBR on day 1 after infusion | Preclinical clinical trial measuring TBR daily after infusion of cetuximab-IRDye800CW [53]. |
| Depth Penetration [54] | Maximum depth for robust signal detection | Up to 3-4 cm | FDPM area illumination and collection in a 1% Liposyn phantom. FDPM enabled greater depth than continuous wave (CW) methods [54]. |
| Excitation Light Intensity [54] | Illumination power for deep tissue imaging | 5.5 mW/cm² | Sufficient for detecting 100 fmol of ICG at 3 cm depth using 785 nm light [54]. |
The choice of imaging technology directly impacts performance. The table below compares two primary methods for light detection in deep tissue.
Table 2: Comparison of Photon Migration Imaging Techniques
| Characteristic | Continuous Wave (CW) | Frequency-Domain Photon Migration (FDPM) |
|---|---|---|
| Principle | Measures the intensity of light attenuated through tissue. | Measures the phase shift and amplitude decay of intensity-modulated light. |
| Background Rejection | Limited ability to reject scattered light. | Superior rejection of scattered photon background. |
| Noise Floor | Higher noise floor. | Lower noise floor. |
| Sensitivity & Depth Penetration | Lower sensitivity and shallower penetration compared to FDPM. | Greater sensitivity and depth penetration; can detect 100 fmol of ICG at 3 cm depth [54]. |
Experimental Protocols and Workflows
Standard Protocol for Ex Vivo Margin Assessment (xFIND)
The Ex Vivo Fluorescence Imaging for Neoplastic Detection (xFIND) is a protocol designed to provide rapid, real-time information about the presence and location of cancer in a resected specimen immediately after excision.
Objective: To intraoperatively identify cancer-containing tissue on the surface of a resected specimen to guide further resection if necessary, without significantly interrupting the surgical workflow [53].
Materials:
- NIR fluorescence imaging system (e.g., repurposed LUNA or other approved device).
- Targeted NIR fluorescent agent (e.g., cetuximab-IRDye800CW).
- Specimen collection tray.
Procedure:
- Agent Administration: The patient receives a microdose (e.g., 1-25% of therapeutic dose) of the targeted fluorescent agent (e.g., cetuximab-IRDye800CW) intravenously 1-3 days before surgery [53].
- Resection: The surgeon performs the standard gross resection of the primary tumor.
- Ex Vivo Imaging: Immediately after resection, the primary specimen is placed on a table within the operating room and imaged with the NIR fluorescence system [53].
- Analysis: Fluorescence is quantified using the system's integrated software. Relative Fluorescence Units (RFU) are measured for suspected tumor regions and background normal tissue. The Tumor-to-Background Ratio (TBR) is calculated [53].
- Decision & Action: A TBR greater than 2.0 is a strong indicator of tumor tissue. If high fluorescence is detected at a surgical margin, the surgeon can be alerted to perform an additional resection of that specific area in the patient's wound bed [53].
- Validation: The resected specimen is sent for standard histopathological processing (e.g., hematoxylin and eosin staining) to confirm the presence of cancer in the fluorescent areas [53].
Diagram 1: Ex Vivo Margin Assessment (xFIND) Workflow. This protocol allows for rapid intraoperative assessment of resection margins.
Protocol for Intraoperative Fluorescence-Guided Resection
This protocol describes the direct, real-time use of FGS to guide the main resection of a tumor.
Objective: To use fluorescence imaging intraoperatively to visually distinguish tumor tissue from normal tissue in the surgical field, guiding the resection boundaries in real-time [53] [50].
Materials:
- NIR-capable laparoscopic stack or open-field camera system.
- Fluorescent contrast agent (e.g., ICG, or a targeted agent like cetuximab-IRDye800CW).
Procedure:
- Preoperative Planning: Based on the agent's pharmacokinetics, administer the fluorescent agent at the optimal time before surgery (e.g., for some targeted agents, this is 1-3 days prior) [53].
- System Setup: Position the fluorescence camera for an ergonomic view of the surgical field. Standardize camera settings (e.g., distance, gain, exposure) for consistent qualitative or quantitative assessment [50].
- Real-Time Resection Guidance:
- The surgeon performs the resection under standard white light.
- Intermittently or continuously, the fluorescence overlay mode is activated.
- Areas with significantly higher fluorescence (TBR > 2.0) are considered tumor tissue and are resected [53].
- Wound Bed Assessment: After the initial resection is deemed complete by white-light inspection, the wound bed is imaged with fluorescence.
- Success: Fluorescence in the wound bed is significantly less than the preresection tumor fluorescence [53].
- Failure: Residual fluorescence hotspots indicate potential positive margins, prompting further resection.
- Margin Confirmation: The resected specimen and any additional shavings from the wound bed are imaged ex vivo (xFIND) and sent for histopathological confirmation [53].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents and Materials for Fluorescence-Guided Surgery Research
| Item | Function / Description | Example(s) |
|---|---|---|
| Non-Targeted Fluorophores | Provides nonspecific contrast based on perfusion and vascular permeability. Often used for perfusion and lymphatic imaging. | Indocyanine Green (ICG), Methylene Blue (MB) [50]. |
| Targeted Bioconjugates | Antibody or peptide conjugated to a fluorophore. Binds to specific molecular targets (e.g., EGFR) on cancer cells, enabling specific detection. | Cetuximab-IRDye800CW (targets EGFR) [53]. |
| Metabolic Agents | A prodrug that accumulates in metabolically active tumor cells and is converted into a fluorescent molecule. | 5-aminolevulinic acid (5-ALA), which is metabolized to fluorescent Protoporphyrin IX (PpIX) in glioma cells [51] [50]. |
| Imaging Devices | Camera systems capable of exciting NIR fluorophores and detecting their emission. Can be open-field or closed-field systems. | LUNA (Novadaq), systems from major surgical imaging companies [53] [50]. |
| Autofluorescence Quenchers | Chemical reagents used to reduce nonspecific background signal from tissue autofluorescence, improving the signal-to-noise ratio. | TrueBlack Lipofuscin Autofluorescence Quencher [2]. |
| 3-Deaza-xylouridine | 3-Deaza-xylouridine, MF:C10H13NO6, MW:243.21 g/mol | Chemical Reagent |
Practical Strategies to Boost Signal, Reduce Noise, and Improve Image Fidelity
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: My fluorescence images have a very low signal-to-noise ratio (SNR), especially when imaging deep tissues. What algorithmic solutions can improve this? A1: Frequency-Domain Denoising (FDD) is a powerful technique for this. It separates the signal from noise in the frequency domain rather than the spatial domain. This method can improve the signal-to-background ratio (SBR) by more than 2,500-fold and the SNR by over 300-fold, which is crucial for deep-tissue imaging where signals are weak [55].
Q2: What are the primary technical challenges limiting penetration depth in fluorescence imaging? A2: The main challenges are related to the interaction of light with tissue. As light travels, it is scattered by tissue structures and absorbed by biomolecules like hemoglobin and water [10]. This results in a weak signal, high background autofluorescence, and a poor signal-to-noise ratio for features located deep within a specimen [56].
Q3: I am using an ICCD detector for video-rate FLIM, but my images are noisy. Are there denoising methods that do not blur image details? A3: Yes, specific denoising algorithms for full-field frequency-domain FLIM data have been developed. These routines effectively eliminate random photon noise and intensifier amplification noise without blurring or smoothing the image, thereby preserving spatial resolution and improving the accuracy of fluorescence lifetime measurements [57].
Q4: Can I use FDA-approved contrast agents for high-precision NIR-II imaging and surgical navigation? A4: Yes, research demonstrates that advanced computational techniques like Frequency-Domain Denoising enable high-quality NIR-II imaging with FDA-approved agents such as Indocyanine Green (ICG). This approach achieves an SBR that far exceeds the Rose criterion, making it feasible for clinical applications like visualizing tumor margins [55].
Troubleshooting Common Experimental Issues
| Problem | Cause | Solution |
|---|---|---|
| Dark or No Fluorescence Image | Microscope shutter closed or ND filter in light path [58]. | Open the shutter and remove unnecessary ND filters [58]. |
| Incorrect filter cube for the fluorophore [58]. | Rotate the correct filter cube into the light path and verify filter combinations match the fluorochrome [58]. | |
| Excessive Background Noise | Insufficient denoising for weak deep-tissue signals [55]. | Apply a frequency-domain denoising (FDD) algorithm during image processing to enhance SBR and SNR [55]. |
| Optical elements (objectives, filters) are dirty [58]. | Clean objectives and filters gently with appropriate solvents like absolute ethanol [58]. | |
| Poor Contrast & Blurred Image | Inappropriate objective lens numerical aperture (NA) [48]. | Use a high-NA objective; image intensity in reflected light fluorescence is proportional to the fourth power of the objective's NA [58]. |
| Thickness of coverslip is incorrect for the objective [58]. | Use coverslips of standard thickness (0.17 mm) and adjust the objective's correction collar if available [58]. |
Detailed Experimental Protocols
Protocol 1: Frequency-Domain Denoising for In Vivo NIR-II Imaging
This methodology enhances fluorescence imaging quality by processing data in the frequency domain to drastically improve signal-to-background ratios [55].
1. Experimental Setup
- Imaging System: A setup capable of NIR-II (900-1880 nm) fluorescence imaging.
- Light Source: A laser source at the appropriate excitation wavelength for your fluorophore.
- Detector: A camera sensitive in the NIR-II window (e.g., an InGaAs camera).
- Subjects: Mice or other animal models.
- Contrast Agent: Indocyanine Green (ICG) or other NIR-II fluorophores [55].
2. Data Acquisition
- Administer the contrast agent (e.g., ICG) to the animal model. The FDD technique can reduce the required dosage by up to 95% [55].
- Acquire a time-series of fluorescence images or video (e.g., at 600 Hz for real-time visualization) of the process of interest, such as vascular flow or agent diffusion [55].
- Critical Step: Ensure the raw image data is saved in a format suitable for post-processing (e.g., 16-bit TIFF stacks).
3. Frequency-Domain Denoising Processing
- Transformation: Convert the acquired image sequence from the spatial domain into the frequency domain using a Fourier Transform.
- Denoising: Apply a custom denoising filter within the frequency domain. This algorithm isolates and suppresses noise components while preserving the signal components corresponding to the genuine fluorescence emission.
- Reconstruction: Perform an Inverse Fourier Transform to reconstruct the denoised image sequence back into the spatial domain.
4. Data Analysis
- Quantify the improvement by calculating the Signal-to-Background Ratio (SBR) and Signal-to-Noise Ratio (SNR) in the processed images versus the raw data. This protocol has been shown to enhance SBR by >2,500-fold and SNR by >300-fold [55].
- Use the denoised video to analyze dynamic processes, such as differentiating arteries from veins based on contrast agent arrival time [55].
Protocol 2: Optimizing Microscope Configuration for Maximum Signal
This protocol outlines steps to configure a fluorescence microscope to maximize image brightness and resolution, which is a prerequisite for effective computational enhancement [58] [48].
1. Objective Lens Selection
- Use an objective with the highest possible Numerical Aperture (NA). Image brightness in epifluorescence microscopy is proportional to the fourth power of the NA (I ∠NAâ´/Mag²) [58].
- For quantitative work, use objectives with high chromatic and spherical correction (e.g., plan-apochromats) that are certified to have low autofluorescence [58].
2. Filter and Light Source Configuration
- Verify that the excitation filter, dichroic mirror, and emission filter (the filter cube) are optimally matched to the excitation and emission spectra of your fluorophore [48].
- Ensure the microscope's light source (e.g., metal halide lamp) provides sufficient intensity at the fluorophore's excitation peak [48].
3. Camera Settings
- For a cooled CCD monochrome camera: Use the following settings to optimize the signal [48]:
- Exposure Time: Increase to collect more light, but be aware this can also increase dark current noise.
- Gain: Amplifies the signal electronically, but also amplifies noise. Use judiciously.
- Binning: Combining adjacent pixels increases signal intensity and speed at the cost of spatial resolution.
Table 1: Performance Metrics of Frequency-Domain Denoising in NIR-II Imaging
| Metric | Raw Data Performance | Post-FDD Performance | Enhancement Factor |
|---|---|---|---|
| Signal-to-Background Ratio (SBR) | Baseline | >2,500x improvement [55] | >2,500-fold [55] |
| Signal-to-Noise Ratio (SNR) | Baseline | >300x improvement [55] | >300-fold [55] |
| Penetration Depth | Baseline | 2x improvement [55] | Doubled [55] |
| Contrast Agent Dosage | 100% | 5% | 95% reduction possible [55] |
Table 2: Key Wavelength Windows for Fluorescence Imaging
| Imaging Window | Wavelength Range | Key Characteristics & Challenges |
|---|---|---|
| Visible | 400 - 700 nm | High photon energy but strong tissue scattering and absorption, leading to very shallow penetration [10]. |
| NIR-I | 700 - 900 nm | Deeper penetration than visible light; used with FDA-approved dyes like ICG and Methylene Blue [10]. |
| NIR-II | 1000 - 1700 nm | Superior penetration depth and contrast due to reduced scattering and autofluorescence [55] [10]. |
| NIR-IIa | 1300 - 1400 nm | Sub-region of NIR-II with further reduced scattering [10]. |
| NIR-IIb | 1500 - 1700 nm | Sub-region of NIR-II offering the highest penetration depth [10]. |
Experimental Workflow and Signaling Pathways
Frequency Domain Denoising Workflow
Problem-Solution Logic for Imaging Depth
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Advanced Fluorescence Imaging
| Item | Function & Rationale |
|---|---|
| Indocyanine Green (ICG) | An FDA-approved fluorophore for NIR-I imaging. When combined with FDD, it can be used for high-contrast NIR-II surgical navigation, visualizing tumor margins and vasculature [55]. |
| NIR-II Fluorophores (e.g., single-walled carbon nanotubes, quantum dots) | Specialized probes that emit light in the NIR-II window (1000-1700 nm). They suffer from reduced scattering and autofluorescence, enabling deeper tissue penetration, but often require computational enhancement to overcome low quantum yield [10]. |
| High-NA Objective Lenses | Microscope objectives with a large Numerical Aperture (NA) are critical for collecting the maximum amount of emitted light. Image brightness in epifluorescence scales with the fourth power of the NA [58]. |
| Cooled CCD Monochrome Camera | The detector of choice for fluorescence microscopy. Cooling reduces dark current noise, and a monochrome sensor typically has higher sensitivity and resolution than a color sensor [48]. |
| Frequency-Domain Denoising (FDD) Algorithm | A computational tool that separates signal from noise in the frequency domain. It is not a physical reagent but is an essential "solution" for achieving order-of-magnitude improvements in SBR and SNR [55]. |
Troubleshooting Guide: Common Probe Design Challenges
This guide addresses frequent issues encountered when designing and optimizing fluorescent probes for deep-tissue imaging, providing targeted solutions to enhance performance.
Problem: Low Quantum Yield (QY) and Brightness
| Challenge | Root Cause | Proposed Solution | Key Experimental Validation |
|---|---|---|---|
| Low Fluorescence Efficiency | Non-radiative decay pathways; Aggregation-caused quenching (ACQ). | Structural rigidification: Incorporate steric hindrance groups (e.g., bulky side chains) to suppress molecular vibration and rotation [59]. Utilize Aggregation-Induced Emission (AIE) gens: Design probes that emit brightly in the aggregated state [59]. | Measure photoluminescence quantum yield (PLQY) using an integrating sphere. Compare PLQY in buffer vs. albumin-containing solutions to assess environmental enhancement [59]. |
| Solvent-/Environment-Dependent Quenching | Polarity-induced twisted intramolecular charge transfer (TICT). | Molecular shielding: Encapsulate hydrophobic cores in nanoparticles or attach hydrophilic polymers (e.g., PEG) to isolate from aqueous environment [60] [61]. Design with hybridized local and charge-transfer (HLCT) states [60]. | Perform solvent-dependent fluorescence spectroscopy in solvents of varying polarity. A red-shift and quenching with increasing polarity indicates TICT [59]. |
Problem: Poor Biocompatibility and Stability
| Challenge | Root Cause | Proposed Solution | Key Experimental Validation | ||
|---|---|---|---|---|---|
| Cytotoxicity | Use of heavy metals (e.g., Cd, Pb in QDs); Reactive functional groups. | Choose organic scaffolds: Use purely organic TADF molecules or NIR-II small molecules [60] [59]. Inorganic shell passivation: For QDs, grow an inert shell (e.g., ZnS) around the core to isolate toxic elements [61]. | Conduct MTT or CellTiter-Glo assays on relevant cell lines (e.g., HEK293, HeLa) over 24-48 hours. Compare IC50 values to established probes. | ||
| Colloidal Instability in Buffer | Surface charge shielding by salts; Hydrophobic aggregation. | Surface functionalization: Graft charged ligands (e.g., COO-, NH3+) or hydrophilic polymers (e.g., PEG, zwitterions) to enhance hydration and electrostatic repulsion [61]. | Use dynamic light scattering (DLS) to monitor hydrodynamic diameter and zeta potential over 7 days in PBS or cell culture media at 37°C. Stable size and | > -15 mV | indicate good colloidal stability [61]. |
| Photobleaching | Oxidative damage from singlet oxygen; Chemical bond breakdown. | Use robust dyes: Choose cyanine derivatives with cyclizable structures or BODIPY dyes known for photostability [59]. Add antifade reagents to mounting media for fixed samples [2]. | Perform continuous irradiation experiments. Measure fluorescence decay half-life (t1/2) under constant illumination and compare to standards like Alexa Fluor dyes [2]. |
Problem: Inefficient Metabolic Clearance and Potential Long-Term Toxicity
| Challenge | Root Cause | Proposed Solution | Key Experimental Validation |
|---|---|---|---|
| Prolonged Body Retention | Large hydrodynamic diameter (>6 nm); Resistance to biodegradation. | Size control: Design small-molecule probes (<5 nm) or biodegradable nanoparticles to enable renal clearance [59]. PEGylation tuning: Use shorter PEG chains (e.g., PEG5k vs. PEG20k) to balance circulation and eventual clearance [61]. | In vivo pharmacokinetics: Inject probe intravenously in mice. Collect blood at time points (e.g., 1 min, 30 min, 2h, 24h, 7d) and measure fluorescence in serum. Calculate half-lives (t1/2α, t1/2β). Ex vivo biodistribution: Quantify fluorescence in organs (liver, spleen, kidneys) at 24h and 7 days post-injection to assess clearance [61] [59]. |
| Reticuloendothelial System (RES) Uptake | Opsonization of nanoparticles by serum proteins. | Stealth coating: Use dense PEG brushes or CD47-mimetic peptides to minimize protein adsorption and mask from macrophages [61]. | Inject probe and image liver/spleen fluorescence intensity over time using NIR-II imaging [62] [59]. A low, rapidly decreasing signal indicates effective evasion of RES. |
Frequently Asked Questions (FAQs)
Q1: My probe has a high QY in organic solvent but it plummets in aqueous buffer. What can I do? This is classic aggregation-caused quenching. Solutions include: (1) Encapsulation: Incorporate the dye into amphiphilic polymer nanoparticles (e.g., DSPE-PEG) that provide a protective hydrophobic pocket [60]. (2) Chemical modification: Attach hydrophilic groups (e.g., sulfonate, PEG) directly to the fluorophore core to enhance water solubility and disrupt π-π stacking [59]. (3) Switch strategy: Consider designing a probe based on Aggregation-Induced Emission (AIE), where fluorescence is enhanced in the aggregate state [59].
Q2: How can I definitively confirm if my probe's low signal is due to rapid metabolic clearance versus poor targeting? You need to dissociate pharmacokinetics from targeting efficiency. Conduct a dual-time point imaging study. Image animals at a very early time point (e.g., 5-15 minutes post-injection) to capture the initial distribution and blood pool signal. Then image again at a later time point (e.g., 4-24 hours). If the signal is high initially but drops rapidly everywhere, the issue is rapid clearance. If the signal is low at both time points, the problem is likely poor targeting or low quantum yield in vivo.
Q3: What are the most critical parameters to balance for achieving deep-tissue penetration? The following parameters are critically linked and must be optimized together, often involving trade-offs:
- Emission Wavelength: Longer wavelengths in the NIR-II window (1000-1350 nm) significantly reduce tissue scattering and autofluorescence, enabling deeper penetration and higher resolution [62] [59].
- Quantum Yield (QY): A high QY is essential for generating a detectable signal from deep tissues, but it must be maintained in the biological environment, not just in solution [63] [59].
- Brightness: This is the product of extinction coefficient and QY. A very bright probe allows for lower dosing, which can improve biocompatibility and clearance profiles [59].
Q4: My probe shows excellent in vitro performance but fails in vivo due to background. What advanced imaging techniques can help? Leverage time-resolved imaging modalities to separate your probe's signal from short-lived autofluorescence.
- Time-Gated Detection: If your probe has a long fluorescence lifetime (e.g., TADF probes with microsecond-millisecond lifetimes), use a delay between excitation and detection. This allows the short-lived (nanosecond) autofluorescence to decay completely, capturing only the specific probe signal [60].
- Fluorescence Lifetime Imaging (FLIM): FLIM can distinguish probes based on their distinct decay lifetimes, even if they emit at similar wavelengths, providing an additional dimension for contrast and multiplexing [60] [64].
Experimental Data and Protocols
Quantitative Impact of Wavelength and QY on Penetration Depth
Monte Carlo simulations reveal the complex interplay between wavelength, quantum yield, and penetration depth, critical for probe design [63].
| Wavelength (nm) | Representative QY (Alexa Fluor) | Relative Detected Emission (at 1 cm depth) | Optimal Use Case |
|---|---|---|---|
| 500 | 0.92 | High, but limited to superficial layers | Surface imaging, cell culture |
| 600 | 0.66 | Moderate | Superficial tissue imaging |
| 700 | 0.36 | Lower than 600nm, but deeper penetration | NIR-I in vivo imaging |
| 800 | 0.12 | Lowest detected signal, but deepest potential penetration | NIR-II / Deep tissue imaging [63] |
Key Insight: The highest QY does not guarantee the best deep-tissue performance. The transition around 600-700 nm is critical, where the trade-off between QY and reduced scattering/absorption begins to favor longer wavelengths for depth [63]. The most significant impact of QY on detected signal occurs in the 600–700 nm range [63].
Protocol: Evaluating Probe Performance in a Deep-Tissue Phantom
This methodology is adapted from the DOLPHIN imaging system to validate probe performance through scattering media [62].
- Phantom Preparation: Create a breast-mimic tissue phantom using Intralipid or similar lipid solution to mimic tissue scattering, and India ink to mimic absorption. Characterize its reduced scattering (μs') and absorption (μa) coefficients.
- Probe Placement: Embed a capillary tube containing your probe solution at a known depth (e.g., 1 cm to 8 cm) within the phantom.
- Imaging Setup: Use a trans-illumination geometry. Illuminate the phantom from the bottom with a NIR laser (e.g., 980 nm). Use a liquid nitrogen-cooled InGaAs camera for NIR-II detection (1000-1700 nm) [62].
- Data Acquisition & Analysis:
- Acquiate hyperspectral cubes (x, y, λ) and diffuse profile images.
- Apply spectral unmixing algorithms to distinguish the probe signal from any phantom autofluorescence or scattering artifacts.
- Reconstruct the 3D location of the probe based on the diffuse light profile.
- Success Metric: The system should be able to locate and resolve a 0.1 mm-sized probe through several centimeters of tissue phantom, a benchmark for detecting small cell clusters [62].
The Scientist's Toolkit: Key Reagents & Materials
| Item | Function | Example Application |
|---|---|---|
| Liquid Nitrogen-Cooled InGaAs Camera | High-sensitivity detection in the NIR-II window (1000-1700 nm). Essential for capturing weak signals from deep tissue [62]. | Deep-tissue optical imaging in live mice [62]. |
| DSPE-PEG (Lipid-Polymer) | Amphiphilic polymer used to encapsulate hydrophobic probes into biocompatible, water-dispersible nanoparticles, improving solubility and circulation time [61]. | Creating stable, clear formulations of organic NIR-II dyes for in vivo injection [59]. |
| Trioctylphosphine Oxide (TOPO) | A coordinating solvent and ligand used in the high-temperature synthesis of quantum dots, providing initial passivation and size control [61]. | Synthesis of high-quality, monodisperse CdSe/ZnS core-shell QDs. |
| Cyanine Dye Derivatives (e.g., IR-26, IR-1061) | Classic organic NIR-II fluorophore scaffolds. Their structures can be modified with targeting moieties and solubility-enhancing groups [59]. | Serving as the core structure for developing targeted NIR-II probes for tumor imaging. |
| TADF Core Molecules (e.g., 4CzIPN, AI-Cz) | Pure organic molecules exhibiting thermally activated delayed fluorescence. Enable time-gated detection to eliminate autofluorescence [60]. | Building blocks for creating organelle-specific (mitochondria, lysosome) probes for high-contrast live-cell imaging. |
Workflow and Strategy Diagrams
Probe Optimization Workflow
Probe Design Strategy Map
Conceptual Foundations: Overcoming Penetration Depth Limits
What are the primary technological principles used to enhance penetration depth in fluorescence imaging of 3D models?
Imaging thick 3D samples, such as tissue models and organoids, presents a significant challenge in fluorescence microscopy. The primary limitation is the presence of out-of-focus light, which creates blur and reduces image contrast, effectively limiting how deep into a sample one can image with clarity. The core principle for overcoming this is optical sectioning—the ability to isolate and collect light only from a thin, in-focus plane within the sample. The table below summarizes how different advanced microscopy techniques achieve this.
Table: Core Principles for Enhancing Penetration Depth in Fluorescence Imaging
| Technique | Core Principle for Optical Sectioning | Key Mechanism for Depth Enhancement |
|---|---|---|
| Confocal Microscopy [65] | Physical rejection of out-of-focus light | A pinhole aperture is placed in front of the detector to block light that is not from the focal plane. |
| Light-Sheet Microscopy [66] | Selective illumination of a single plane | Only a thin "sheet" of light is used to illuminate the sample, ensuring that regions above and below the focal plane are not excited. |
| Multi-Photon Microscopy [66] | Non-linear excitation confined to a tiny volume | Fluorophores are only excited at the focal point where photon density is highest, providing inherent optical sectioning. |
| FLIM (Functional Imaging) [67] | Lifetime-based contrast, independent of intensity | Measures the fluorescence lifetime, which is sensitive to the local microenvironment (e.g., pH, ion concentration), providing functional contrast in deep tissue. |
These principles form the foundation for the specific instrumentation and troubleshooting guidance detailed in the following sections.
Troubleshooting Guides & FAQs
A. Confocal Microscopy for 3D Models
Q1: My confocal images from deep tissue sections appear hazy with low contrast. What are the primary causes and solutions?
Haze and low contrast are typically caused by out-of-focus light and scattered photons reaching the detector [65].
- Cause 1: Incorrect pinhole adjustment. A pinhole opened too wide will allow out-of-focus light to contribute to the image.
- Solution: Reduce the pinhole diameter to the minimum practical size, ideally to 1 Airy Unit (AU), to optimize optical sectioning and lateral resolution [65]. Be aware that this will reduce signal intensity, which may require compensating with higher laser power or detector gain.
- Cause 2: Scattering and aberration in thick samples. As light penetrates deeper into tissue, it scatters, and refractive index mismatches can distort the point spread function (PSF).
- Solution: Use objectives with a high Numerical Aperture (NA) and consider those with correction collars to compensate for coverslip thickness and sample-induced spherical aberrations [68]. Mounting samples in media with a refractive index matched to the tissue is also critical.
- Cause 3: Insufficient signal-to-noise ratio (SNR). To combat haze, you may close the pinhole, but this sacrifices signal.
- Solution: Optimize the trade-off between resolution and light collection efficiency. For dim samples, a slightly larger pinhole may be necessary to collect enough photons for a usable image at the cost of some sectioning quality [65].
Q2: What are the key considerations when choosing between a Laser Scanning Confocal (LSCM) and a Spinning Disk Confocal (SDCM) for live 3D model imaging?
The choice hinges on the balance between speed, light efficiency, and resolution.
- Laser Scanning Confocal (LSCM):
- Best for: High-resolution, multi-dimensional imaging (e.g., 3D z-stacks, 4D time-lapse, 5D spectral) where versatility is key [65].
- Advantages: Excellent optical sectioning, adjustable pinhole, and easy integration with spectral detectors and other modalities like FLIM [65].
- Disadvantages: Slower scanning speed and higher intensity of light per voxel, which can lead to photobleaching and phototoxicity in live samples [65].
- Spinning Disk Confocal (SDCM):
- Best for: High-speed imaging of dynamic processes in live cells or tissues (e.g., calcium signaling, membrane dynamics) [65].
- Advantages: Much faster acquisition rates (video rate) and significantly reduced light dose per voxel, minimizing photodamage [65].
- Disadvantages: The pinhole size is fixed and not adjustable, and there can be issues with pinhole crosstalk in very thick or bright samples [65].
Table: Comparison of Confocal Modalities for 3D Model Imaging
| Feature | Laser Scanning Confocal (LSCM) | Spinning Disk Confocal (SDCM) |
|---|---|---|
| Imaging Speed | Slower (point scanning) | Very Fast (multi-point parallel scanning) |
| Light Efficiency / Phototoxicity | Lower / Higher | Higher / Lower |
| Pinhole Adjustment | Adjustable | Fixed |
| Optimal Use Case | High-resolution, multi-dimensional imaging of fixed or robust live samples | High-speed, low-light live-cell imaging |
B. Fluorescence Lifetime Imaging (FLIM)
Q3: Why is FLIM particularly advantageous for functional imaging in thick 3D tissues, and what is its key synergy with FRET?
FLIM provides a readout that is independent of fluorophore concentration, excitation light intensity, and detection path losses, which are all variables that plague intensity-based measurements in scattering tissues [67].
- Advantage 1: Microenvironment Sensing. The fluorescence lifetime is sensitive to the local environment of the fluorophore, including pH, ion concentration (e.g., Ca²âº), temperature, and viscosity. This allows for direct functional readouts of metabolic state (e.g., via NADH autofluorescence) in deep tissue [67].
- Advantage 2: Synergy with FRET. FLIM is a robust method to measure Förster Resonance Energy Transfer (FRET). When FRET occurs, the donor fluorophore's lifetime decreases. FLIM-FRET measures this change, providing a precise and quantitative way to monitor protein-protein interactions, conformational changes, and biosensor activity deep within 3D samples, free from artifacts related to signal intensity or spectral bleed-through [67].
Q4: My FLIM data from deep within an organoid is noisy. What acquisition and analysis strategies can improve data quality?
Noise in FLIM can stem from low photon counts and scattering.
- Strategy 1: Maximize Photon Collection. Use highly sensitive detectors (like HyD or PMT). Increase the signal by using bright, photostable dyes or higher expression levels of fluorescent proteins, if possible. In living samples, balance laser power and acquisition time to maximize photons while minimizing phototoxicity.
- Strategy 2: Utilize Phasor Analysis. The phasor approach to FLIM is a fitting-free, graphical method that is more robust to noise and allows for easy visualization and separation of multiple lifetime components within a pixel, which is highly beneficial for complex samples like organoids [67].
- Strategy 3: Leverage Modern Integrated Systems. New commercial systems (e.g., Leica's STELLARIS 8 FALCON) seamlessly integrate FLIM into standard confocal workflows, offering video-rate FLIM acquisition and user-friendly analysis tools like TauSense, which simplifies extracting lifetime-based contrast [67].
C. High-Throughput Screening (HTS) Systems
Q5: How do I select the appropriate microplate and detection method for a 3D cell-based assay in an HTS environment?
The choice of labware and reader is critical for assay performance and data quality.
- Microplate Selection:
- Material: Use Cyclic Olefin Copolymer (COC) or clear Polypropylene (PP) plates for compound storage and assays involving DMSO, as they are DMSO-resistant and less prone to breakage [69].
- Well Bottom: For high-resolution imaging with high-NA objectives, use plates with an optically clear, flat glass bottom to minimize aberrations [69].
- Surface Treatment: Ensure the plate is tissue culture-treated to promote cell attachment and spheroid formation [69].
- Detection Method Selection:
- Absorbance: Rarely used for 3D models due to low sensitivity and scattering.
- Fluorescence Intensity: Common, but susceptible to interference from autofluorescence and inner filter effects.
- Luminescence: Highly sensitive with a large dynamic range and low background, ideal for reporter assays in dense 3D models.
- Fluorescence Polarization (FP) & Time-Resolved FRET (TR-FRET): Excellent for binding assays, as they are homogeneous (no washing) and less prone to compound autofluorescence interference, making them robust for HTS [69] [70].
- High-Content Imaging (HCI): Systems like the PerkinElmer Operetta combine confocal-like optical sectioning with automation, allowing for morphological analysis of 3D models in an HTS format [70].
Q6: What are the common configuration errors in HTS readers that can lead to poor data quality in 3D model screens?
- Error: Incorrect Read Direction.
- Problem: Using "Top Read" for assays where cells are adherent to the bottom of the plate can result in a weak and variable signal due to the long path length through the media and spheroid.
- Solution: For adherent cells or spheroids, always use "Bottom Read" configuration with a clear-bottom plate to maximize signal collection efficiency [69].
- Error: Lack of Environmental Control.
- Problem: Long screening runs without control of temperature and COâ‚‚ can affect cell viability and gene expression in 3D models, leading to unreliable data.
- Solution: Use HTS systems with integrated environmental chambers (temperature & COâ‚‚ control) for any live-cell assay lasting more than a few minutes [70].
Quantitative Data & Instrument Comparison
Table: Key Performance Metrics for Advanced Imaging Techniques
| Technique | Lateral Resolution | Axial Resolution | Reported Imaging Depth in Tissue | Key Detection Technology |
|---|---|---|---|---|
| Widefield Fluorescence | ~0.2 μm [65] | ~0.6 μm [65] | Very Limited | CCD/CMOS Camera |
| Laser Scanning Confocal | ~0.2 μm (can be improved) [65] | ~0.6 μm (can be improved) [65] | Moderate (~100 μm) | Photomultiplier Tube (PMT) |
| C2SD-ISM (Advanced Confocal) | 144 nm [71] | 351 nm [71] | Up to 180 μm [71] | sCMOS Camera |
| FLIM (as a contrast method) | Dependent on base microscope (Confocal, Multi-photon) | Dependent on base microscope | Deep (when combined with Multi-photon) | Time-Correlated Single Photon Counting (TCSPC) or Fast Gating |
Experimental Protocols & Workflows
Protocol: C2SD-ISM for High-Fidelity Deep-Tissue Super-Resolution
This protocol is adapted from a recent study demonstrating a novel dual-confocal system for deep tissue [71].
1. Principle: Confocal² Spinning-Disk Image Scanning Microscopy (C2SD-ISM) integrates a physical spinning-disk (first confocal level) to eliminate out-of-focus light, with a Digital Micromirror Device (DMD) for sparse multifocal illumination and a computational pixel reassignment algorithm (second confocal level) to achieve super-resolution.
2. Materials:
- Microscope: Custom-built C2SD-ISM system [71].
- Light Source: High-power multi-mode laser (e.g., 405 nm, 488 nm, 561 nm) coupled with a square homogenizing fiber for uniform illumination [71].
- Modulator: Digital Micromirror Device (DMD) for generating programmable multifocal patterns.
- Confocal Component: Spinning-disk (SD) unit with a multi-concentric spiral pinhole pattern.
- Detector: sCMOS camera.
- Sample: Fixed or live thick tissue samples (up to 180 μm).
3. Procedure:
1. System Alignment: Conjugate the sample focal plane, the SD pinhole array, the DMD, and the sCMOS sensor plane.
2. DMD Pattern Design: Program the DMD to project a sparse, periodic lattice of excitation spots. Each spot is formed by a 4x4 block of "ON" DMD pixels.
3. Raw Data Acquisition:
* The SD disk rotates, scanning the pinhole array across the field of view.
* For each SD position, the DMD pattern is shifted across the sample in 108 nm steps (on-sample), acquiring a stack of raw images (I_i).
* The image formation is described by: I_i = [Obj(r,z) · I_i(r,z)] ⊗_3D PSFsys(r,z), where Obj is the sample, I_i is the illumination, and PSFsys is the system PSF [71].
4. Image Reconstruction:
* Apply the Dynamic Pinhole Array Pixel Reassignment (DPA-PR) algorithm. This algorithm corrects for non-ideal conditions like Stokes shifts and optical aberrations.
* The reconstruction reassigns the light from each scanning spot to its true origin, effectively doubling the resolution and producing a final super-resolution image with high fidelity (92% linear correlation to original confocal data reported) [71].
C2SD-ISM System Workflow: A dual-confocal strategy for deep-tissue super-resolution imaging.
Protocol: Enhancing Polarization Contrast with Double-Tagged FPs
This protocol details a method to improve contrast in Fluorescence Polarization Microscopy (FPM) for living cells, a technique that can provide orientational information in 3D structures [72].
1. Principle: Standard fluorescent proteins (FPs) linked to structures by a single tag (st-FPs) can rotate, blurring polarization data. Double-tagging (dt-FPs) rigidly anchors the FP, locking its transition dipole moment to the sample's structure and dramatically enhancing polarization contrast.
2. Materials:
- Microscope: Standard or confocal fluorescence microscope capable of modulating/rotating the polarization of the excitation laser.
- Plasmids: Constructs for double-tagged, reversibly photoswitchable FPs (dt-rsFPs), e.g., p-Kohinoor-F (farnesylated and palmitoylated) [72].
- Research Reagent Solutions:
- dt-rsFPs (e.g., p-Kohinoor-F, p-rsGreenF-F): Engineered fluorescent proteins with two membrane anchoring motifs (farnesylation + palmitoylation) to rigidly lock orientation [72].
- Cell Lines: HeLa cells or primary hippocampal neurons for transfection and expression of dt-rsFPs [72].
- Imaging Buffer: Standard live-cell imaging buffer compatible with the chosen FPs.
- Research Reagent Solutions:
- Cells: Living HeLa cells or hippocampal neurons expressing the dt-rsFPs.
3. Procedure:
1. Sample Preparation: Transfert your cell line with the dt-rsFP plasmid and culture for 24-48 hours to allow for expression and proper membrane localization.
2. Data Acquisition with FrExPAN:
* Employ a Frame-separated Excitation Polarization Angle Narrowing (FrExPAN) scheme. This novel pulse scheme uses a primary excitation beam and a secondary, perpendicularly polarized de-excitation beam to selectively excite only fluorophores with a very narrow range of orientations [72].
* Acquire a stack of images while rotating the polarization angle (α).
3. Data Analysis:
* For each pixel, plot fluorescence intensity (I_Fl) against the polarization angle (α).
* For dt-FPs, the signal will closely follow a sharp I_Fl(α) = y_0 + A cos²(α - x) function, indicating high orientation contrast.
* Perform a Fast Fourier Transform (FFT) on the modulation signal for each pixel. The resulting phase (x) and amplitude (A) can be color-coded to create an orientation map of the underlying cellular structure [72].
Polarization Contrast Enhancement: Rigid anchoring of fluorophores via double-tagging significantly improves signal quality for FPM.
A core challenge in fluorescence imaging research is the fundamental limitation of light penetration depth in biological tissues. The interaction of photons with tissue components—through absorption by molecules like hemoglobin and water, and scattering by cellular structures—severely attenuates both the excitation light and the emitted fluorescence signal [73]. This attenuation is inversely related to wavelength; longer wavelengths in the near-infrared (NIR) regions, particularly the second near-infrared window (NIR-II, 1000–1700 nm), experience significantly reduced scattering and absorption, thereby enabling greater penetration depth and higher resolution imaging compared to visible light [73]. This technical note, framed within the context of overcoming penetration depth limitations, provides a targeted troubleshooting guide for optimizing the use of fluorescent agents to achieve a strong signal output while minimizing reagent consumption—a critical balance for both cost-effectiveness and reducing potential background noise or toxicity in sensitive experiments.
Troubleshooting Guides
Guide 1: Addressing Suboptimal Fluorescence Signal
Problem: The fluorescence signal from your sample is too dim or absent, making detection and analysis difficult.
| Problem Area | Possible Cause | Recommended Solution | Supporting Protocol / Data |
|---|---|---|---|
| Agent Dosage & Staining | Antibody or dye concentration is too low [2]. | Perform a titration experiment to find the optimal concentration. Start with 1 µg/mL for primary antibodies [2]. | A clinical dose-ranging study found a strong correlation (R²=0.54) between dose (mg/kg) and Mean Fluorescence Intensity (MFI), with optimal signal around 0.75 mg/kg for a weight-based dose [74] [75]. |
| Intracellular target not accessible for surface staining [2]. | Confirm antibody epitope is extracellular. If not, perform intracellular staining with permeabilization [2]. | Ensure the antibody immunogen is in an extracellular domain for cell surface staining applications [2]. | |
| Imaging Setup | Incorrect filter set for the dye [48]. | Verify that the excitation/emission spectra of your dye overlap with the transmission bands of your filter set [48]. | Check manufacturer websites for spectral data. For example, a filter labeled "470/40" transmits the 470 nm ±20 nm band [48]. |
| Inappropriate camera settings or type [48]. | Use a cooled monochrome CCD camera for high S/N. Adjust exposure time first, then gain (which amplifies noise) [48]. | For weak signals, use camera binning to increase signal intensity at the cost of resolution [48]. | |
| Low Numerical Aperture (NA) lens [48]. | Switch to a lens with a larger NA, which gathers more light and produces a brighter image [48]. | A larger NA provides higher resolution but a shallower depth of field [48]. | |
| Agent & Sample | Photobleaching during microscopy [2]. | Use an antifade mounting medium. Reduce light exposure intensity and duration. Choose photostable dyes (e.g., rhodamine-based) [2]. | Adding antifade reagent to samples allowed clear fluorescence imaging even after 30 seconds of exposure [3]. |
| Fluorophore is not being efficiently excited [48]. | Ensure your light source (e.g., mercury, metal halide, LED) generates strong output at the excitation peak of your dye [48]. | LED and laser sources are specific to wavelengths; ensure compatibility with your dye's spectrum [48]. |
Guide 2: Addressing High Background or Poor Contrast
Problem: The fluorescence signal is present, but a high background or poor contrast obscures the specific signal, leading to a low signal-to-noise ratio (SNR) or tumor-to-background ratio (TBR).
| Problem Area | Possible Cause | Recommended Solution | Supporting Protocol / Data |
|---|---|---|---|
| Agent Dosage & Specificity | Antibody concentration is too high [2]. | Titrate the antibody concentration to find the level that maximizes specific signal while minimizing background [2]. | A clinical study found no direct correlation between TBR and dose, highlighting that more agent does not automatically improve contrast [74] [75]. |
| Non-specific binding of the fluorescent agent [2]. | Use highly cross-adsorbed secondary antibodies. Optimize blocking buffers (e.g., use IgG-free BSA) [2]. | Charged dyes (e.g., Alexa Fluor 647) can cause non-specific binding; specialized blockers can mitigate this [2]. | |
| Sample Properties | Tissue autofluorescence [2]. | Include an unstained control. Use far-red or NIR dyes to avoid blue-wavelength autofluorescence. Use autofluorescence quenchers [2]. | Tissue autofluorescence is significantly reduced in the NIR-II region (>1000 nm) compared to visible light, drastically improving SNR [73]. |
| Blood absorbing excitation light [76]. | Remove surface blood from the wound bed or tissue before imaging, as it absorbs light and can mask fluorescence [76]. | Blood does not fluoresce and its presence can prevent the excitation light from reaching the underlying fluorescent agent [76]. | |
| Imaging Parameters | Fluorescence cross-talk in multicolor experiments [2]. | Image single-stain controls in all channels to check for bleed-through. Choose dyes with well-separated spectra [2]. | For flow cytometry, apply fluorescence compensation. For confocal microscopy, optimize scanning settings to minimize cross-talk [2]. |
| Administration Timing | Long circulation time leading to high background [74]. | Optimize the time between agent administration and imaging (infusion-to-surgery window). | In a clinical study, MFI significantly increased when the infusion-to-surgery window was reduced to within 2 days compared to 3 days or more (p < 0.05) [74] [75]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental advantage of NIR-II imaging over visible light fluorescence? NIR-II light (1000-1700 nm) experiences significantly reduced scattering and absorption in biological tissues compared to visible light. This results in deeper tissue penetration, higher spatial resolution, and a greatly improved signal-to-background ratio due to minimal tissue autofluorescence in this wavelength window [73].
Q2: Should I use a fixed dose or a weight-based dose for my fluorescent agent in an animal study? The choice depends on the agent and model. A clinical study on panitumumab-IRDye800CW found that both fixed and weight-based dosing could be effective. The data suggested that a fixed dose of 50 mg or a weight-based dose of 0.75 mg/kg provided optimal Mean Fluorescence Intensity (MFI), with no significant difference in performance between the two dosing strategies [74] [75].
Q3: Why must fluorescence imaging with devices like the MolecuLight i:X be performed in the dark? Ambient light can overwhelm the relatively weak fluorescence signals emitted by bacteria and tissues. A dark environment ensures that these fluorescence signals are clearly visualized and accurately interpreted by the imaging device [76].
Q4: How can I prevent photobleaching of my fluorescent sample? Implement several strategies: 1) Add antifading reagents to your mounting medium; 2) Reduce the intensity of the excitation light; 3) Limit the sample's exposure to light by using shutters to block excitation when not capturing data; and 4) Select fluorophores known for high photostability [3] [2].
Q5: Besides bacteria, what else can cause fluorescence in a wound? Many biological and non-biological sources can fluoresce. Biological sources include collagen (green) and fibrin (green) in tissues. Non-biological sources can include tattoo inks, certain bedding materials, and other fluorescent dyes. It is crucial to compare fluorescence images with standard white light images for accurate interpretation [76].
Workflow and Signaling Pathway Diagrams
Fluorescence Imaging Optimization Workflow
Dose Optimization Decision Pathway
The Scientist's Toolkit: Key Research Reagents & Materials
The following table details essential materials and reagents used in fluorescence imaging experiments, along with their critical functions for achieving optimal results.
| Item | Function & Purpose | Key Considerations |
|---|---|---|
| NIR-II Fluorophores [73] | Fluorescent probes (e.g., lanthanide nanoparticles, quantum dots, organic small molecules) that emit light in the 1000-1700 nm range for deep-tissue imaging. | Enable high-resolution imaging with superior penetration depth and reduced autofluorescence compared to visible/NIR-I probes [73]. |
| Targeted Antibody-Dye Conjugates [74] [75] | Antibodies (e.g., anti-EGFR) conjugated to NIR dyes (e.g., IRDye800CW) for specific molecular targeting of cancer cells. | Dosing (e.g., 50 mg fixed dose) and administration timing (1-2 days pre-surgery) are critical for optimal signal and TBR [74] [75]. |
| Indocyanine Green (ICG) [77] | An FDA-approved, water-soluble tricarbocyanine dye used as a marker for vascular perfusion and angiography. | Binds to plasma proteins; excitation/emission in the NIR region allows for deeper tissue visualization [77]. |
| Antifade Mounting Media [3] [2] | A reagent added to samples to slow the photobleaching of fluorophores during microscopy. | Essential for preserving fluorescence signal intensity over multiple or long-duration imaging sessions [3] [2]. |
| Autofluorescence Quenchers [2] | Chemical reagents used to reduce the innate background fluorescence of tissues (e.g., from lipofuscin or elastin). | Particularly important when using blue fluorescent dyes, as autofluorescence is highest in blue wavelengths [2]. |
| High-NA Objective Lenses [48] | Microscope lenses with a high Numerical Aperture that gather more light, resulting in brighter images and higher resolution. | A larger NA provides a brighter signal but a shallower depth of field; correct cover glass thickness is critical [48]. |
| Cooled Monochrome CCD Camera [48] | A camera type that cools its sensor to reduce dark current noise, enabling high-sensitivity detection of weak fluorescence signals. | Ideal for fluorescence microscopy due to its high signal-to-noise ratio, especially compared to color cameras [48]. |
Core Challenges & Multimodal Solutions
Fluorescence imaging is a powerful tool for biomedical research, offering high sensitivity and specificity for visualizing molecular and cellular processes. However, its effectiveness is limited by fundamental physical constraints. The table below summarizes the primary challenges and how integrating fluorescence with other imaging modalities provides powerful solutions.
| Challenge | Description | Multimodal Solution |
|---|---|---|
| Limited Penetration Depth | Visible light scatters strongly in biological tissues, restricting high-resolution fluorescence imaging to superficial structures (typically < 1 cm) [14] [78]. | Combination with PET, MRI, or Photoacoustics leverages modalities (sound, radio waves) that experience less attenuation, enabling deep-tissue imaging [79] [80]. |
| Background Autofluorescence | Endogenous molecules in tissues can fluoresce under excitation light, creating a high background signal that reduces the signal-to-noise ratio [14] [78]. | Spectral Unmixing in Multimodal Imaging allows researchers to distinguish the probe's signal from background autofluorescence by analyzing multiple data channels [79] [81]. |
| Low Quantitative Accuracy | Light scattering distorts the fluorescence signal intensity, making it difficult to obtain accurate, quantifiable data on biomarker concentration from deep tissues [14]. | Complementary Data Fusion uses high-contrast, quantitative data from PET or MRI to contextualize and refine fluorescence findings, improving overall quantification [79] [81]. |
| Lack of Anatomical Context | Fluorescence images often show molecular activity but provide poor detail of surrounding anatomical structures [79]. | Hybrid Anatomical/Molecular Imaging overlays fluorescence data onto high-resolution anatomical images from MRI or CT, providing precise spatial context [79] [81]. |
Troubleshooting Multimodal Integration
This section addresses common experimental issues encountered when integrating fluorescence with other imaging modalities.
Fluorescence & PET Integration
Issue: Misalignment between high-sensitivity PET signal and fluorescence molecular target.
- Potential Cause 1: Differential probe pharmacokinetics. The fluorescent and radioactive moieties of a multimodal probe may have different in vivo stability, binding affinities, or clearance rates.
- Solution: Perform rigorous preclinical validation of the conjugated probe to ensure the fluorescence and PET signals co-localize over time. Use size-exclusion chromatography to check probe stability in serum [81].
- Potential Cause 2: Spatial resolution mismatch. PET's spatial resolution (1-2 mm) is lower than modern fluorescence imaging, which can cause apparent misregistration.
- Solution: Use image fusion algorithms that account for the intrinsic resolution differences of each modality. High-resolution CT or MRI, often bundled with PET, can serve as an intermediary for accurate co-registration with fluorescence.
Issue: Low signal-to-noise ratio for fluorescence component in deep tissues.
- Potential Cause: Suboptimal fluorophore choice. Using fluorophores that excite and emit in the visible light spectrum, which is highly scattered.
- Solution: Switch to Near-Infrared-II (NIR-II, 1000-1700 nm) fluorophores. Imaging within this biological window significantly reduces scattering and autofluorescence, providing greater penetration and a higher signal-to-noise ratio [79] [78].
Fluorescence & MRI Integration
Issue: Fluorescence signal is quenched or altered by the MRI contrast agent.
- Potential Cause: Energy transfer between probes. If the fluorescent dye and MRI contrast agent (e.g., gadolinium chelate, iron oxide nanoparticle) are in close proximity, paramagnetic effects can quench the fluorescence.
- Solution: Optimize the probe design by increasing the molecular spacer between the fluorophore and the MRI-active moiety. Test the probe's fluorescence quantum yield before and after conjugation to the MRI agent [81].
Issue: Inability to correlate real-time fluorescence dynamics with MRI anatomy.
- Potential Cause: Temporal resolution disparity. MRI acquisitions can be slow, while fluorescence dynamics may occur on a seconds-to-minutes timescale.
- Solution: Implement interleaved or sequential imaging protocols. Acquire a high-resolution anatomical MRI scan first, then perform the fluorescence time-series acquisition. The MRI data provides a static anatomical map onto which the dynamic fluorescence data is overlaid.
Fluorescence & Photoacoustic Imaging Integration
Issue: Strong photoacoustic background from hemoglobin obscures specific fluorescent probe signal.
- Potential Cause: Spectral coloring and dominant endogenous contrast. The strong optical absorption from hemoglobin (an endogenous chromophore) can mask the photoacoustic signal from an exogenous fluorescent probe.
- Solution: Employ multispectral photoacoustic imaging. Acquire PA signals at multiple wavelengths and use spectral unmixing algorithms to isolate the unique absorption signature of the fluorescent probe from that of hemoglobin [80] [82].
Issue: Weak photoacoustic conversion efficiency of the fluorescent probe.
- Potential Cause: Poor photothermal conversion. The fluorescent probe may have high quantum yield but low efficiency in converting absorbed light into heat, which is essential for generating a photoacoustic signal.
- Solution: Develop or select probes specifically engineered for photoacoustics. Organic dyes with strong donor-acceptor structures and high non-radiative decay rates, or nanoparticles with strong NIR absorption (e.g., gold nanorods), are excellent candidates [78].
Experimental Protocols
Protocol: Co-registration of Fluorescence and Photoacoustic Images for Vasculature Imaging
This protocol details the steps to visualize vascular structures by leveraging the endogenous contrast of hemoglobin in photoacoustic imaging and validating it with a fluorescent dye.
Principle: Photoacoustic imaging can detect oxygenated and deoxygenated hemoglobin based on their distinct optical absorption spectra, providing high-resolution deep-tissue images of blood vessels. A fluorescent dye (e.g., Indocyanine Green, ICG) is used to confirm the vascular nature of the PA signal and provide complementary information [80].
Diagram Title: Workflow for Fluorescence and Photoacoustic Co-registration
Materials:
- Photoacoustic Imaging System: Equipped with a tunable laser (e.g., 680-900 nm range) and an ultrasonic transducer [82].
- Fluorescence Imager: For NIR imaging (e.g., ICG: Ex ~780 nm, Em ~820 nm).
- Animal Model: Mouse or rat.
- Contrast Agent: Indocyanine Green (ICG) solution [80] [78].
- Software: For spectral unmixing (e.g., MATLAB-based scripts) and image co-registration (e.g., AMIRA, 3D Slicer).
Procedure:
- Animal Preparation: Anesthetize the animal according to institutional protocols. Secure the animal in the imaging chamber and maintain body temperature.
- Baseline PA Imaging: Acquire a multi-wavelength PA image dataset (e.g., at 750, 800, and 850 nm) of the region of interest before contrast agent injection. This provides a baseline of endogenous hemoglobin contrast.
- Contrast Agent Administration: Intravenously inject ICG via a tail vein catheter (e.g., 100 µL of 100 µM solution).
- Multimodal Image Acquisition:
- PA Imaging: Immediately after injection, acquire another multi-wavelength PA dataset at the same locations and wavelengths as step 2.
- Fluorescence Imaging: Simultaneously or immediately following PA acquisition, capture a fluorescence image of the same field of view using the appropriate filters for ICG.
- Image Processing:
- PA Data: Use spectral unmixing algorithms on the post-injection dataset to separate the contributions of ICG from oxygenated and deoxygenated hemoglobin [80].
- Fluorescence Data: Apply flat-field correction and background subtraction to the fluorescence image.
- Image Co-registration: Use the fiduciary markers or the animal's anatomical features to align the processed PA image (showing hemoglobin and ICG) with the fluorescence image (showing ICG) into a single, multi-channel dataset.
Troubleshooting Notes:
- Weak ICG PA Signal: Ensure the laser is tuned to one of ICG's peak absorption wavelengths (e.g., ~800 nm).
- Poor Image Registration: Incorporate fiducial markers filled with a contrast agent (e.g., India ink) that is visible in both modalities to facilitate accurate alignment.
Protocol: Validating a Multimodal (Fluorescence/MRI) Nanoprobe In Vivo
This protocol describes how to validate the targeting efficiency and biodistribution of a nanoparticle probe that contains both a fluorescent tag and an MRI contrast agent.
Principle: A single nanoprobe is functionalized with a NIR fluorophore and an MRI-active component (e.g., superparamagnetic iron oxide, SPIO). MRI is used for non-invasive, whole-body tracking of the probe's biodistribution, while fluorescence imaging ex vivo provides high-sensitivity validation of its localization at the cellular level [79] [81].
Diagram Title: Workflow for Validating a Fluorescence/MRI Nanoprobe
Materials:
- Multimodal Nanoprobe: e.g., SPIO nanoparticle conjugated to a Cy5.5 or similar NIR dye.
- MRI Scanner: Preclinical system (e.g., 7T or higher).
- Fluorescence Imager: For whole-organ and histological slide imaging.
- Animal Model: Disease model (e.g., tumor-bearing mouse) and healthy controls.
- Tools: For tissue harvesting and processing (cryostat, etc.).
Procedure:
- Probe Characterization: Prior to in vivo use, characterize the probe's size (via dynamic light scattering), fluorescence quantum yield, and MRI relaxivity (R2 or R2*).
- Pre-injection Baseline MRI: Place the animal in the MRI scanner and acquire a set of baseline T2-weighted or T2*-weighted images. This will serve as a reference for contrast-induced signal changes.
- Probe Administration: Intravenously inject the multimodal nanoprobe.
- In Vivo MRI Time-Course: Acquire MRI scans at multiple time points post-injection (e.g., 1, 4, 24, 48 hours) using the same parameters as the baseline scan. The accumulation of the SPIO-based probe will cause a decrease in signal (darkening) in T2-weighted images at the target site.
- Ex Vivo Validation:
- At the final time point, euthanize the animal and harvest the target organs and major organs (liver, spleen, kidneys, etc.).
- Image the whole organs using a fluorescence imager to visualize the distribution of the probe.
- Quantify the fluorescence intensity in each organ to determine the biodistribution profile.
- Histological Correlation: Embed organs in OCT medium and section them. Image the tissue sections using fluorescence microscopy to confirm probe localization at the cellular level, co-registering with histological stains (e.g., H&E).
Troubleshooting Notes:
- High Non-specific Liver/Spleen Uptake: This is common for nanoparticles. Modify the probe's surface with polyethylene glycol (PEG) to prolong circulation time and enhance targeting [81].
- No MRI Signal Change: Confirm the probe's relaxivity is sufficient for in vivo detection and that the MRI sequence parameters (e.g., TE) are optimized to detect T2 changes.
Research Reagent Solutions
The following table lists key reagents and their functions for developing and implementing multimodal imaging studies.
| Reagent / Material | Function in Multimodal Imaging | Key Considerations |
|---|---|---|
| Indocyanine Green (ICG) | Clinically approved NIR-I fluorescent dye; also acts as a photoacoustic contrast agent due to its strong NIR absorption [80] [78]. | Limited photostability; binds to plasma proteins. |
| NIR-II Fluorophores (e.g., Rare Earth-Doped NPs) | Fluorophores emitting in the second biological window (1000-1700 nm) for dramatically reduced scattering and deeper tissue fluorescence imaging [79]. | Requires specialized NIR-II detectors; synthesis can be complex. |
| o-Phenylenediamine-based Probes | A common chemical scaffold for constructing "activatable" fluorescent probes for biomarkers like Nitric Oxide (NO). The reaction with NO forms a triazole, switching the fluorescence on [78]. | Provides high specificity but requires careful probe design to minimize background. |
| Superparamagnetic Iron Oxide Nanoparticles (SPIOs) | MRI contrast agent that causes strong T2/T2* signal darkening; can be conjugated to fluorophores for multimodal (Fluorescence/MRI) imaging [81]. | Core size and surface coating critically determine biodistribution and MRI relaxivity. |
| DNA-PAINT / RESI Kits | Super-resolution fluorescence microscopy kits that enable angstrom-level resolution by using transient DNA binding and sequential imaging [83]. | Used for fixed cells, not live imaging; requires multiple rounds of staining and imaging. |
Frequently Asked Questions (FAQs)
Q1: Can I perform true simultaneous fluorescence and photoacoustic imaging? Yes, it is technically feasible. Some advanced systems integrate a pulsed laser for photoacoustic excitation and a continuous-wave laser for fluorescence excitation, with a shared ultrasonic detector for PA and optical detection for fluorescence. However, most setups perform sequential acquisition to avoid signal interference, which is sufficient for many applications if the time between acquisitions is minimized [80] [82].
Q2: What is the single most critical factor for successful fluorescence-PET probe co-registration? The most critical factor is the biological stability and integrity of the dual-labeled probe. The chemical link between the fluorophore and the radionuclide must be stable in circulation to ensure that both signals originate from the same target. Differential cleavage or metabolism will lead to misregistration and erroneous data [81].
Q3: We see a good MRI contrast change with our probe but a weak fluorescence signal in deep tissues. Should we abandon fluorescence? Not necessarily. This is a common scenario that highlights the strength of multimodal imaging. The MRI provides the deep-tissue, anatomical context. You can then use the MRI data to guide subsequent ex vivo fluorescence imaging of excised tissues. This allows you to validate the probe's location with the high sensitivity and resolution of fluorescence microscopy on tissue sections, confirming cellular-level localization [79] [81].
Q4: How does spectral unmixing work in multispectral photoacoustic imaging? Multispectral photoacoustic imaging involves acquiring PA signals at multiple wavelengths across the absorption spectrum of your target chromophore (e.g., your probe) and interfering chromophores (e.g., hemoglobin). Advanced algorithms then analyze the unique spectral signature of each chromophore at each pixel, mathematically separating their contributions to generate a pure map of your probe's distribution, free from background hemoglobin contrast [80].
Q5: What are the key advantages of using organic dyes over quantum dots for multimodal probes? Organic dyes are generally preferred for clinical translation due to their potential for better biocompatibility and biodegradability. They offer exceptional structural versatility, allowing chemists to tune their optical properties and incorporate specific activation mechanisms. However, they can suffer from lower photostability compared to quantum dots. The choice depends on the specific application and the trade-off between brightness, stability, and biocompatibility requirements [78].
Benchmarking Fluorescence Solutions Against Clinical Standards and Modalities
This technical support center provides a structured comparison of four pivotal molecular imaging technologies: Fluorescence Imaging (FI), Positron Emission Tomography (PET), Magnetic Resonance Imaging (MRI), and Computed Tomography (CT). Understanding the strengths and limitations of each modality is crucial for selecting the appropriate tool for specific biomedical research and clinical applications, particularly in drug development. The following sections offer a detailed technical breakdown, troubleshooting guides, and FAQs, framed within the critical context of penetration depth limitations, a primary challenge in fluorescence imaging research.
Technical Specifications and Comparison
The table below summarizes the core technical parameters of each imaging modality for a direct, head-to-head comparison. These specifications are key to determining the suitability of a technique for a given experimental or clinical goal.
| Feature | Fluorescence Imaging (FI) | Positron Emission Tomography (PET) | Magnetic Resonance Imaging (MRI) | Computed Tomography (CT) |
|---|---|---|---|---|
| Imaging Principle | Detection of emitted light from excited fluorophores [14] | Detection of gamma rays from radioactive tracers [14] | Measurement of radiofrequency signals from protons in a magnetic field [14] | Measurement of X-ray attenuation through tissue [14] |
| Penetration Depth | Superficial (µm to a few mm) [14] | Whole body (unlimited) | Whole body (unlimited) | Whole body (unlimited) |
| Spatial Resolution | High (for superficial tumors) [14] | Low (several mm) | High (sub-mm) | High (sub-mm) |
| Temporal Resolution | Real-time imaging [14] | Minutes to hours | Minutes to hours | Seconds to minutes |
| Key Advantage(s) | Non-radioactive, real-time, high sensitivity & specificity for superficial targets [14] | High sensitivity, deep-tissue quantitative molecular data [14] | Excellent soft-tissue contrast, no ionizing radiation | Fast, excellent for bone anatomy and lung imaging |
| Primary Limitation(s) | Limited penetration, background autofluorescence, photobleaching [14] | Use of ionizing radiation, lower spatial resolution, cost [14] | Long scan times, high cost, sensitive to motion | Use of ionizing radiation, poor soft-tissue contrast |
| Molecular Sensitivity | Very High | Very High | Low | Very Low |
| Common Applications | Cellular & superficial tumor imaging, intraoperative guidance [14] | Oncology, neurology, cardiology, drug distribution studies [14] | Neuroimaging, musculoskeletal imaging, oncology | Trauma, oncology (metastasis detection), lung imaging |
Troubleshooting Guides and FAQs
This section addresses common practical challenges researchers face, with a focus on fluorescence imaging.
Fluorescence Imaging Troubleshooting
Frequently Asked Questions: Fluorescence Imaging
Q: My fluorescence signal is very weak or absent. What should I check first? A: Begin by verifying your primary antibody is validated for your specific application (e.g., flow cytometry, immunofluorescence) and has confirmed species reactivity. Always include a positive control. Next, perform an antibody titration to optimize concentration, as too little antibody will result in weak signal. Finally, confirm the accessibility of your target; an antibody for an intracellular epitope requires permeabilization for staining [2].
Q: How can I reduce high background and non-specific staining? A: High background often stems from tissue autofluorescence or antibody cross-reactivity [2].
- Autofluorescence: Use an unstained control to determine baseline levels. Consider using far-red dyes instead of blue dyes, as autofluorescence is typically higher in blue wavelengths. Products like TrueBlack Lipofuscin Autofluorescence Quencher can be highly effective [2].
- Cross-reactivity: Perform a control with the secondary antibody alone. For multiplex experiments, use highly cross-adsorbed secondary antibodies and stain with primary-secondary pairs separately to detect unexpected interactions [2].
Q: My fluorophores are photobleaching too quickly. How can I preserve my signal? A: Photobleaching is the loss of fluorescence upon light exposure [14]. To mitigate it:
- Use Antifade Reagents: Incorporate mounting media with antifade properties, such as ProLong Diamond for fixed samples or ProLong Live for live-cell imaging. These contain antioxidants that scavenge free radicals [84].
- Choose Stable Dyes: Select more photostable dyes like many Alexa Fluor dyes [84].
- Reduce Light Exposure: Lower the intensity of the light source (laser power), use neutral density filters, and minimize the sample's viewing time by closing the shutter when not acquiring images [3] [84].
Q: What are the best practices for maintaining my fluorescence microscope to ensure optimal image quality? A:
- Brightness & Lamps: Use high-energy light sources (mercury or xenon lamps) and ensure they are replaced when flickering or illumination becomes uneven [3].
- Lens Care: Clean objective lenses gently and regularly with appropriate solvents (absolute ethanol or distilled water) to remove dust and oil. Avoid corrosive solvents like ammonia [3].
- Environment: Keep the microscope in a clean, dark, vibration-free room and covered when not in use [3].
Cross-Modality Comparative FAQs
Q: When should I choose Fluorescence Imaging over PET for molecular studies? A: Fluorescence Imaging is superior for superficial tumors and real-time studies where no radioactivity is desired. It offers higher spatial resolution for accessible targets [14]. PET is necessary for whole-body, deep-tissue quantitative imaging to track biodistribution or target engagement in internal organs, despite its lower spatial resolution and use of radioactivity [14].
Q: How does the information from MRI and CT complement molecular data from FI or PET? A: CT provides high-resolution anatomical context (excellent for bone), while MRI offers superb soft-tissue contrast. Both are often combined with PET (as PET/CT or PET/MRI) to overlay the high-sensitivity molecular data from PET with detailed anatomical information. Similarly, fluorescence data can be fused with CT or MRI volumes for anatomical context [14] [85].
Essential Research Reagents and Materials
The following table details key reagents and materials critical for successful fluorescence imaging experiments.
| Reagent/Material | Function | Example Applications |
|---|---|---|
| BODIPY Dyes | Versatile fluorescent probes with high quantum yields and photostability; emission tunable from 500-700 nm [14]. | Cellular imaging; targeted cancer imaging when conjugated to ligands like folic acid [14]. |
| Alexa Fluor Dyes | A family of bright, photostable synthetic dyes covering a wide spectrum of excitation/emission wavelengths [14]. | General immunofluorescence, flow cytometry, and multiplexed imaging [2]. |
| Indocyanine Green (ICG) | A near-infrared (NIR) clinical-grade fluorophore. | Angiography, tracking tissue perfusion, and intraoperative imaging due to deeper tissue penetration of NIR light [14]. |
| Targeted Antibodies | Monoclonal or polyclonal antibodies conjugated to fluorophores for specific antigen binding. | Visualizing specific proteins (e.g., Trastuzumab for HER2 tumors) [14]. |
| Antifade Mounting Media | Reagents containing antioxidants to reduce photobleaching by scavenging free radicals. | Preserving fluorescence signal in fixed samples for long-term storage (e.g., ProLong Diamond) [84]. |
| Autofluorescence Quenchers | Reagents that chemically reduce endogenous background fluorescence from tissues. | Improving signal-to-noise ratio in tissue sections (e.g., TrueBlack Lipofuscin Autofluorescence Quencher) [2]. |
Experimental Protocol: Fluorescence Imaging with Cryo-Imaging for Validation
This protocol outlines a method for high-resolution validation of fluorescence distributions ex vivo, which can be used to confirm findings from in vivo imaging modalities like PET.
Title: Cryo-Imaging & 3D Fusion Workflow
1. Objective: To acquire microscopic-resolution 3D datasets of anatomical color and molecular fluorescence from a whole-mouse specimen, enabling precise localization of fluorescently labeled cells (e.g., cancer, stem cells) within an anatomical context for validation of in vivo imaging data [85].
2. Materials:
- Fresh or fixed tissue sample (e.g., mouse).
- Optimal Cutting Temperature (OCT) compound.
- Cryo-imaging system with motorized cryostat, bright-field/fluorescence stereo microscope, and robotic positioner [85].
- Liquid nitrogen.
3. Methodology:
- Sample Preparation: Embed the tissue sample in OCT compound and flash-freeze it in liquid nitrogen to preserve tissue structure and fluorescence [85].
- System Setup: Mount the frozen block onto the cryo-imaging system stage.
- Alternate Sectioning and Imaging: The automated system performs a cycle of: a. Imaging: Capturing a high-resolution, tiled color image and fluorescence image(s) of the block face. b. Sectioning: Precisely sectioning a thin slice (typically 10-40 µm) off the block face using the cryomicrotome. c. Repetition: This cycle is repeated hundreds or thousands of times, generating a stack of sequential images [85].
- 3D Reconstruction: The stack of 2D images is computationally reconstructed into a 3D volume for both color and fluorescence channels.
- Data Fusion and Visualization: The fluorescence volume is fused and co-registered with the color anatomy volume. Using volume rendering software (e.g., Amira), researchers can interactively explore the data, adjusting opacity transfer functions to enhance specific anatomical features or fluorescent signals. This allows for the clear visualization of, for example, metastatic cells within the context of an organ [85].
4. Data Analysis: This technique provides unique, multi-scale data, allowing zooming from a whole-mouse view down to the level of single cells. The fusion of fluorescence and anatomy enables direct, unambiguous analysis of the biodistribution of labeled cells or agents within their anatomical context [85].
Core Quantitative Metrics and Measurement Methodologies
This section details the key performance metrics used to evaluate fluorescence imaging systems. The following table summarizes standardized measurement protocols for quantitatively assessing these parameters.
Table 1: Standardized Metrics and Methodologies for Evaluating Fluorescence Imaging Performance
| Metric | Description | Quantitative Measurement Protocol |
|---|---|---|
| Signal-to-Noise Ratio (SNR) [86] [87] [88] | Ratio of the desired fluorescence signal to the total background noise. Critical for detecting faint signals and accurate quantification. | Calculate as the mean signal intensity from a fluorescent sample divided by the standard deviation of the background noise. System components like cameras contribute read noise, dark current, and clock-induced charge [86] [87]. |
| Spatial Resolution [88] | Ability to distinguish two adjacent point sources as separate entities. | Image a fluorescence resolution test phantom featuring straight grooves with spacings that gradually increase (e.g., from 0 mm to 2 mm). The smallest resolvable spacing defines the resolution [88]. |
| Penetration Depth [88] | Maximum depth within a scattering medium at which a usable fluorescence signal can be detected. | Use a test block with wells or channels of different depths filled with a fluorescent contrast agent (e.g., ICG). The deepest well from which a clear signal is obtained indicates the system's detection depth [88]. |
| Dynamic Response Range [88] | Range of fluorophore concentrations over which the signal response is linear. | Image a series of circular wells containing fluorescent contrast agents at different, known concentrations. The range where signal intensity scales linearly with concentration defines the dynamic response [88]. |
| Brightness Uniformity [88] | Consistency of illumination and signal detection across the entire field of view. | Image a test phantom with multiple identical wells distributed across the field of view (e.g., center and 0.7 times the field of view). Calculate the coefficient of variation (standard deviation/mean) of the signal intensities from these wells [88]. |
Experimental Protocols for Key Metrics
Protocol: Camera Noise Characterization
Accurately characterizing camera noise is foundational for quantifying SNR, as it validates the core components of the noise model [87].
- Purpose: To experimentally measure the individual noise contributions of a microscope camera (readout noise, dark current, clock-induced charge) and verify manufacturer specifications [87].
- Materials: Microscope with a cooled camera (EMCCD or sCMOS recommended), camera control software.
- Method:
- Read Noise (
σ_read): Acquire a "dark frame" image with the light path completely closed (shutter closed), using the shortest possible exposure time and no electron-multiplication (EM) gain. The standard deviation of the pixel intensities in this image is a direct measure of the read noise [87]. - Dark Current (
σ_dark): Acquire a series of dark frames with a long exposure time (e.g., several seconds). The increase in noise variance compared to the short-exposure dark frame is used to calculate the dark current noise [87]. - Clock-Induced Charge (
σ_CIC): Acquire dark frames with the EM gain enabled. The additional noise variance beyond the read noise and dark current is attributed to the clock-induced charge [87].
- Read Noise (
- Data Analysis: The total noise variance is the sum of the individual variances:
σ²_total = σ²_photon + σ²_dark + σ²_CIC + σ²_read. A validated noise model allows for precise SNR calculation and system optimization [87].
Protocol: Standardized Fluorescence Sensitivity and SNR Measurement
This protocol uses a standardized phantom to objectively quantify a system's fluorescence detection capabilities [88].
- Purpose: To quantitatively evaluate the sensitivity and Signal-to-Noise Ratio of a fluorescence imaging system using a calibrated test phantom.
- Materials:
- Method:
- Titrate a series of fluorescent contrast agent solutions with known, descending concentrations into the 16 wells of the phantom.
- Acquire fluorescence images of the phantom using the system under test.
- For each well, measure the mean signal intensity within the well.
- Select a region of the phantom with no fluorescent agent to measure the mean background intensity and the standard deviation of the background noise.
- Data Analysis:
- Sensitivity: The lowest concentration that produces a signal statistically significant above the background.
- SNR: For each well, calculate
SNR = (Mean Signal Intensity - Mean Background Intensity) / Standard Deviation of Background[88].
Troubleshooting FAQs: Addressing Common Experimental Challenges
FAQ 1: My fluorescence signal is too dim, and I have poor contrast. What are the primary factors I should check?
A dim signal and poor contrast often result from suboptimal component selection or configuration [89] [48].
- Check Filter Compatibility: Ensure the excitation and emission filter spectra have high transmissibility and properly overlap with the peak excitation and emission spectra of your fluorophore. A mismatch will drastically reduce signal [48].
- Use a High-NA Objective: Image brightness in reflected light fluorescence is proportional to the fourth power of the objective's Numerical Aperture (NA). A high-NA objective gathers significantly more light [89].
- Select an Appropriate Light Source: Verify that your light source (e.g., mercury, metal halide, LED) emits strong output at the specific wavelength needed to excite your fluorophore [48].
- Optimize Camera Settings: Use a cooled monochrome camera for high sensitivity and low noise. Increase exposure time first to collect more signal, but be aware of potential increased dark current. Use gain cautiously as it amplifies both signal and noise [48].
FAQ 2: I have verified my components, but my background noise is still high. How can I reduce it?
High background noise can be caused by external light contamination, camera heat, or sample preparation issues [86] [89].
- Eliminate Ambient Light: Perform microscopy in a darkened room and ensure the microscope is light-tight. Introduce a wait time in the dark before image acquisition to allow stray light to dissipate [86].
- Ensure Proper Sample Washing: Thoroughly wash your specimen to remove any unbound fluorochrome, which is a common source of high background and reduced contrast [89].
- Cool the Camera Sensor: Use the camera's cooling function (e.g., Peltier device) to reduce dark current, which is a temperature-dependent source of noise [48].
- Add Secondary Filters: Introducing extra emission or excitation filters can effectively block stray light and reduce excess background noise, which has been shown to improve SNR by up to 3-fold [86].
FAQ 3: My images are blurry and lack sharpness. How can I improve spatial resolution?
Image blurriness can be due to optical aberrations, improper setup, or scattering [89] [48].
- Use High-Quality, Clean Objectives: Choose plan-apochromatic objectives for superior chromatic and spherical correction. Ensure all optical elements, especially the objective front lens, are clean and free of dust, oil, or debris [89].
- Correct for Coverslip Thickness: Use the correct coverslip thickness (typically 0.17 mm) for your objective. If your high-NA dry objective has a correction collar, adjust it to compensate for any deviation in coverslip thickness [89].
- Optimize Microscope Alignment: Ensure the light source (arc lamp) is properly centered and aligned (Köhler illumination) for even, bright illumination without glare [89].
- Minimize Light Scattering: For deep tissue imaging, advanced techniques like wavefront shaping with a Bessel-Gauss (BG) beam can help counteract scattering-induced aberrations, thereby improving resolution and contrast at depth [90].
Workflow Visualization
The following diagram illustrates the logical workflow for diagnosing and resolving common issues in fluorescence imaging, based on the troubleshooting guides and experimental protocols.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table lists key materials and tools essential for conducting rigorous fluorescence imaging experiments and for the quantitative evaluation of system performance.
Table 2: Essential Research Reagents and Tools for Fluorescence Imaging
| Item | Function / Description | Application Example |
|---|---|---|
| Standardized Fluorescence Test Phantom [88] | A physical calibration tool with wells and patterns of known geometries and depths, used to standardize performance testing. | Quantitatively measuring system resolution, sensitivity, SNR, penetration depth, and brightness uniformity in a reproducible manner [88]. |
| Indocyanine Green (ICG) [88] | A near-infrared (NIR) fluorescent contrast agent approved for clinical use, known for its safety and excellent fluorescent properties. | Used as a standard fluorophore in performance testing of NIR fluorescence imaging systems and in preclinical/clinical applications [88]. |
| High-NA Objective Lens [89] | A microscope objective with a high Numerical Aperture, crucial for collecting maximum emitted light. | Increasing image brightness and resolution in reflected light fluorescence microscopy, where intensity is proportional to NAâ´ [89]. |
| Cooled Monochrome CCD/sCMOS Camera [48] [91] | A camera system where cooling reduces dark current noise, and a monochrome sensor provides higher sensitivity than a color sensor. | Essential for low-light fluorescence imaging to achieve a high SNR, allowing for the detection of faint signals [48] [91]. |
| Spectral Modeling Software (e.g., SearchLight) [92] | A free online tool for modeling and evaluating the spectral performance of fluorophores, filter sets, light sources, and detectors. | Predicting system performance, optimizing filter selection to maximize signal and minimize crosstalk before performing wet-lab experiments [92]. |
| Automated Signal Quantification Software (e.g., TrueSpot) [93] | An automated software tool designed for the robust detection and quantification of signal puncta in 2D and 3D fluorescent images. | Reducing subjectivity and improving consistency in the analysis of RNA-FISH, immunofluorescence, and other puncta-based assays [93]. |
Technical Support Center
Troubleshooting Guides
Issue 1: Inadequate Fluorescence Signal During 5-ALA Guided Surgery
Problem: Tumor fluorescence is weak or absent, compromising the surgeon's ability to distinguish tumor margins.
Potential Causes and Solutions:
- Insufficient 5-ALA dosing or timing: Administer 20 mg/kg body weight orally 3-4 hours before anesthesia to ensure optimal protoporphyrin IX (PpIX) accumulation [94] [95].
- Suboptimal microscope filter system: Use a surgical microscope equipped with a blue light source (370-440 nm) and appropriate long-pass filter to visualize the 635-704 nm emission peak of PpIX [94] [95].
- Photobleaching during procedure: Limit prolonged exposure of the surgical field to the excitation light. Use the microscope's shutter to block excitation light when not actively viewing fluorescence [3] [2].
- Inappropriate patient selection: Confirm high-grade glioma diagnosis preoperatively. 5-ALA-induced PpIX accumulation is most pronounced in WHO Grade 3-4 gliomas with blood-brain barrier disruption [94].
Issue 2: High Background or Non-Specific Fluorescence
Problem: Excessive background signal makes it difficult to distinguish tumor tissue from healthy brain parenchyma.
Potential Causes and Solutions:
- Autofluorescence from surgical materials: Ensure all surgical materials (cottonoids, gauze) are free of autofluorescent compounds. Use specialized non-fluorescent materials when available [2].
- Tissue autofluorescence: Distinguish specific PpIX fluorescence (peaks at 635-704 nm) from tissue autofluorescence, which is typically broader spectrum and most prominent in blue wavelengths [2] [96].
- Blood contamination: Maintain a clean surgical field through adequate hemostasis and irrigation, as blood can absorb both excitation and emission light [94].
Issue 3: Discrepancy Between Fluorescence and Tumor Histopathology
Problem: Intraoperative fluorescence findings don't correlate with postoperative histopathological analysis.
Potential Causes and Solutions:
- Infiltrative tumor regions with low fluorescence: Recognize that 5-ALA visualizes the solid tumor core most effectively. Use intraoperative sampling of weakly fluorescent regions at tumor margins for frozen section analysis [94].
- Non-neoplastic pathologies causing fluorescence: Consider that other pathologies with blood-brain barrier disruption (e.g., radiation necrosis, abscess) may cause nonspecific fluorescence [94].
- Incomplete molecular profiling: Incorporate WHO 2021 classification criteria including IDH mutation status, as 5-ALA efficacy varies across molecular subtypes of gliomas [94].
Frequently Asked Questions
Q: What is the evidence that 5-ALA improves surgical outcomes compared to white-light surgery? A: Multiple studies demonstrate that 5-ALA significantly increases gross total resection (GTR) rates. A 2025 retrospective analysis of 141 patients showed GTR rates of 28.17% in the 5-ALA group versus 12.86% in the conventional white-light group (p = 0.0245) [94]. A systematic review and network meta-analysis further confirmed that 5-ALA leads to significantly increased GTR rates compared to resections without intraoperative guidance [95].
Q: Does improved GTR with 5-ALA translate to survival benefits? A: The relationship is complex. While 5-ALA significantly increases GTR rates, and GTR itself is associated with improved survival (log-rank p = 0.0423), 5-ALA usage was not an independent predictor of survival (HR = 0.885, 95% CI: 0.554-1.413, p = 0.612) in multivariate analysis. Survival outcomes are influenced by multiple factors including adjuvant therapies and patient functional status [94].
Q: How does 5-ALA compare to other intraoperative guidance techniques like fluorescein sodium or intraoperative MRI? A: A network meta-analysis compared these modalities and found intraoperative MRI most efficacious for achieving GTR, followed by fluorescein sodium, then 5-ALA, though differences between them were not statistically significant. All three significantly increased GTR rates compared to surgeries without intraoperative guidance [95].
Q: What are the practical limitations of 5-ALA fluorescence in glioma surgery? A: Key limitations include:
- Limited penetration depth of excitation light and emitted fluorescence
- Decreasing fluorescence signal with increasing tissue depth
- Inability to visualize deeply located or extensively infiltrative tumor components
- Variable fluorescence intensity across different molecular subtypes of gliomas
- Need for specialized equipment including a fluorescence-capable surgical microscope [94]
Q: What safety considerations are associated with 5-ALA use? A: 5-ALA (Gliolan) carries a risk of skin photosensitivity for up to 24 hours after ingestion. Patients should be protected from direct sunlight and intense artificial light for 24-48 hours postoperatively. The compound is generally well-tolerated with few other reported side effects [95].
Quantitative Data Comparison
Table 1: Gross Total Resection Rates in 5-ALA vs. White-Light Guided Surgery
| Study Group | Number of Patients | GTR Rate | Statistical Significance | Reference |
|---|---|---|---|---|
| 5-ALA Group | 71 | 28.17% | p = 0.0245 | [94] |
| White-Light Group | 70 | 12.86% | [94] |
Table 2: Multivariate Predictors of Survival in Glioma Patients
| Factor | Hazard Ratio | 95% Confidence Interval | p-value |
|---|---|---|---|
| Radiotherapy | 0.291 | 0.166-0.513 | <0.001 |
| Karnofsky Performance Status | 0.962 | 0.942-0.982 | 0.0003 |
| Gross Total Resection | 0.476 | 0.272-0.834 | 0.0091 |
| 5-ALA Usage | 0.885 | 0.554-1.413 | 0.612 |
Experimental Protocols
Protocol 1: Standardized 5-ALA Administration and Surgical Procedure
- Preoperative Preparation: Administer 20 mg/kg body weight of 5-ALA orally dissolved in 50 mL of water 3-4 hours before induction of anesthesia [94].
- Anesthesia Considerations: Standard anesthetic protocols can be used without special modifications for 5-ALA.
- Surgical Equipment Setup:
- Utilize a fluorescence-capable surgical microscope (e.g., ZEISS BLUE 400)
- Ensure proper function of blue light source (370-440 nm) and emission filters
- Confirm white-light balance for conventional visualization [94]
- Intraoperative Workflow:
- Begin tumor resection under white-light illumination
- Switch to blue light excitation to visualize fluorescent tumor tissue
- Resect fluorescent areas while preserving non-fluorescent brain tissue
- Use final blue light inspection to confirm complete resection of fluorescent tissue [94]
Protocol 2: Postoperative Assessment of Extent of Resection
- Imaging Protocol: Perform contrast-enhanced MRI within 72 hours postoperatively [94].
- GTR Definition: Define gross total resection as complete absence of contrast-enhancing tumor on early postoperative MRI [94].
- Volumetric Analysis: Use dedicated software for precise quantification of residual tumor volume when present.
- Correlation with Histopathology: Ensure concordance between intraoperative fluorescence findings and histopathological diagnosis of tumor type and grade.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for 5-ALA Fluorescence Studies
| Item | Function/Application | Specifications/Notes |
|---|---|---|
| 5-aminolevulinic acid (5-ALA) | Precursor for protoporphyrin IX accumulation in tumor cells | Oral administration, 20 mg/kg body weight; FDA-approved as Gliolan [94] [95] |
| Fluorescence-capable Surgical Microscope | Visualization of PpIX fluorescence | Equipped with blue light source (370-440 nm) and appropriate emission filters [94] |
| Protoporphyrin IX (PpIX) | Endogenous fluorophore accumulated in tumor cells | Emission peaks at 635-704 nm; selectively accumulates in high-grade glioma cells [94] |
| High-grade Glioma Cell Lines | In vitro models for mechanism studies | Include various molecular subtypes (IDH-mutant, IDH-wildtype) [94] |
| Animal Glioma Models | In vivo testing of 5-ALA efficacy | Orthotopic implantation models best recapitulate clinical scenario |
Methodological Workflows
Evaluating Toxicity and Safety Profiles of Novel Probes for Clinical Readiness
The translation of novel fluorescent probes from laboratory research to clinical application is a complex process, with safety and toxicity profiling representing a critical gateway. Within the broader context of overcoming penetration depth limitations in fluorescence imaging, the chemical and biological properties of a probe directly influence its clinical viability [14]. Key challenges include ensuring probe biocompatibility, minimizing off-target effects, and achieving favorable pharmacokinetic profiles while maintaining optimal imaging performance deep within biological tissues [14] [97]. This technical support center provides structured guidance to help researchers navigate these challenges through robust experimental design and troubleshooting.
Technical FAQs: Addressing Common Experimental Challenges
Q1: Our initial toxicity screening in cell lines shows good biocompatibility, but we observe unexpected organ-level toxicity in murine models. What could be causing this discrepancy?
A1: Discrepancies between in vitro and in vivo toxicity often arise from factors not captured in simple cell culture models:
- Metabolic Transformation: The probe may be metabolized in the liver into a compound with different toxicity profiles [97]. It is essential to conduct in vitro studies using liver microsomes or hepatocytes to identify and characterize potential metabolites early in the development pipeline.
- Accumulation in Reticuloendothelial System (RES): Nanoparticles and some macromolecular probes can accumulate in the liver and spleen, leading to localized toxicity not evident in standard cell lines [98]. Histopathological analysis of these organs post-administration is crucial.
- Immune Response: The probe might be triggering an innate or adaptive immune response, such as complement activation [97]. Screening for immune markers and conducting studies in immunocompetent models can help identify this issue.
Q2: The fluorescence signal from our probe fades quickly during in vivo imaging, compromising data collection. Is this due to toxicity or a technical issue?
A2: Signal loss is typically a technical issue related to photostability, not immediate toxicity:
- Photobleaching: Continuous exposure to excitation light causes irreversible photochemical damage to the fluorophore [99] [48]. Mitigate this by reducing excitation light intensity, using a more photostable probe (e.g., BODIPY derivatives [14]), or incorporating anti-fading agents.
- Chemical Environment: Local pH or reactive oxygen species (ROS) in the cellular environment can quench fluorescence or degrade the probe [99]. Characterize your probe's stability under various pH and redox conditions.
- Clearance Kinetics: The signal loss may simply reflect the probe's normal biological clearance from the body [97]. Always correlate imaging data with pharmacokinetic studies to distinguish clearance from photobleaching.
Q3: How can we accurately assess the safety of a probe designed for deep-tissue imaging when our current models are superficial?
A3: Evaluating safety for deep-tissue applications requires models that account for unique physiological factors:
- Use Tissue Phantoms: Before moving to complex in vivo models, utilize tissue-simulating phantoms with controlled optical properties (scattering and absorption coefficients) to study probe behavior at depth [18] [21] [98].
- Choose Relevant Animal Models: Conduct safety and efficacy studies in animal models with spontaneous diseases (e.g., canine tumors), as their pathophysiology and tissue structure more closely mimic human conditions [97].
- Monitor Systemic Exposure: Ensure your toxicity studies administer the probe via the intended clinical route (e.g., intravenous) and measure biodistribution and retention in deep organs over time [97].
Quantitative Safety & Efficacy Profiling
Data from preclinical studies must be quantitatively summarized to make informed decisions about clinical readiness. The following table exemplifies key parameters for a hypothetical novel NIR probe, "DA364," based on a real-world study [97].
Table 1: Preclinical Safety and Imaging Efficacy Profile of a Novel NIR Fluorescent Probe (DA364) in a Canine Model
| Parameter | Results / Finding | Methodology / Notes |
|---|---|---|
| Tolerability | Well tolerated after IV administration | No adverse events reported in 24 dogs across tested doses [97] |
| Dose Range Tested | 0.06 mg/m² to 3.0 mg/m² | Escalating dose study to identify optimal imaging dose and maximum tolerated dose [97] |
| Tumor Types Imaged | Mammary tumors, mast cell tumors, sarcomas | Demonstrates potential for broad application [97] |
| Optimal Imaging Time (TI) | ~24 hours post-injection | Time interval for sufficient target accumulation and background clearance [97] |
| Tumor-to-Background Ratio (TBR) | Median TBR: 1.8 to 4.2 (depending on tumor type) | Measured in situ; TBR > 2 is generally considered desirable for clear delineation [97] |
| Residual Disease Detection | Identified residual fluorescence in wound beds with confirmed disease | Highlights potential for fluorescence-guided surgery to improve resection completeness [97] |
Essential Experimental Protocols
In Vitro Binding Affinity and Specificity Assay
This protocol is critical for confirming that the probe engages its intended target before moving to complex in vivo studies [97].
- Solid Phase Binding Assay: Immobilize the target protein (e.g., integrin αvβ3) on a microtiter plate.
- Competitive Binding: Incubate the immobilized target with a mixture of a known, labeled ligand (e.g., vitronectin) and increasing concentrations of your fluorescent probe.
- Measurement & Analysis: Measure the remaining bound labeled ligand. Fit the data to determine the half-maximal inhibitory concentration (IC₅₀) of your probe. A low nM IC₅₀ (e.g., 2.5 ± 0.2 nM for DA364 [97]) indicates high affinity.
- Specificity Test: Repeat the assay with related but off-target proteins to confirm specificity.
Cellular Uptake and Internalization Assay
This protocol evaluates whether the probe is internalized by target cells, which can impact signal strength and toxicity [97].
- Cell Culture: Use a cell line that overexpresses the target receptor (e.g., WM266 human melanoma cells for αvβ3 integrin [97]).
- Probe Incubation: Treat cells with the fluorescent probe at a predetermined concentration (e.g., 5 µM) for a set time (e.g., 4 hours).
- Competition Control: Include a control group pre-treated with an excess of an unlabeled competitor to demonstrate that uptake is receptor-specific.
- Analysis: Use fluorescence microscopy (e.g., confocal microscopy) or flow cytometry to quantify internalization. A significant reduction in signal (>85% inhibition) in the competed group confirms specificity [97].
Workflow for Preclinical Safety and Efficacy Evaluation
The following diagram outlines the logical progression from early development to clinical readiness, integrating the protocols and considerations discussed.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful evaluation of probe safety and efficacy relies on a suite of specialized reagents and materials.
Table 2: Essential Materials for Probe Toxicity and Efficacy Evaluation
| Category / Item | Function / Purpose | Specific Examples & Notes |
|---|---|---|
| Target-Specific Probes | Binds to overexpressed molecular targets on tumor cells for specific imaging. | DA364 (cRGD-Cy5.5 targeting integrin αvβ3) [97]; Folate-conjugated BODIPY for folate receptor-positive cancers [14]. |
| High-Performance Fluorophores | Provides the signal for detection; properties like brightness and stability are key. | Cy5.5 (higher quantum yield than ICG) [97]; BODIPY dyes (high quantum yield, photostability) [14]; Cypate, DTTCI (NIR dyes for FLIM) [100]. |
| Control Agents | Essential for validating the specificity of probe binding and uptake. | Unlabeled competitor (e.g., cRGD peptidomimetic for DA364) to block specific binding [97]. |
| Tissue Phantoms | Calibrate imaging systems and simulate light propagation in tissue at various depths. | Agarose phantoms with Intralipid (scattering) and metHb (absorption) [21] [98]; Multi-layered phantoms for depth sensitivity testing [18]. |
| Validated Cell Lines | Provide a controlled in vitro system for initial binding and toxicity assays. | WM266 cells (high integrin αvβ3 expression) [97]; Raw264.7 macrophage cells for uptake studies [100]. |
| Animal Models of Disease | Assess probe performance and safety in a physiologically relevant in vivo environment. | Rodent models of human cancers; canine patients with spontaneous tumors [97]. |
Frequently Asked Questions (FAQs)
What are the primary cost-benefit advantages of implementing wide-field fluorescent imaging in resource-limited settings?
The primary advantages are significant cost reduction, portability, and high throughput. One demonstrated platform uses a cell-phone-based microscope with cost-effective components: a simple lens (~$12), a plastic colour filter (~$1.10), LEDs (~$0.30 each), and a battery (~$0.50) [101]. The entire attachment weighs only ~28 grams, is compact, and can screen large sample volumes (>0.1 mL) over a wide field-of-view (~81 mm²), making it a high-throughput and accessible tool for locations with limited laboratory infrastructure [101].
How do penetration depth and wavelength selection impact fluorescence imaging quality in biomedical applications?
Light scattering and absorption in biological tissues significantly limit penetration depth and image quality. Imaging in the second near-infrared window (NIR-II, 1000-1700 nm) offers major advantages over visible light (400-700 nm) or NIR-I (700-900 nm) [10]. In the NIR-II window, photon scattering is reduced, and absorption by biomolecules like hemoglobin and water is lower, leading to deeper tissue penetration, higher resolution, and a superior signal-to-background ratio [10]. Notably, research has shown that even regions with high water absorption (e.g., 1880-2080 nm) can be exploited for high-contrast imaging, as absorption preferentially attenuates scattered background light [102].
What are common causes of fluorescent signal failure or high background, and how can they be addressed?
Common issues and their solutions are summarized in the table below.
Table: Troubleshooting Common Fluorescence Imaging Issues
| Problem | Possible Cause | Solution |
|---|---|---|
| No or Low Signal | Antibody not validated for the application [2]. | Check supplier information; validate with a positive control [2]. |
| Intracellular target not accessible [2]. | Confirm target localization; use intracellular staining protocols if needed [2]. | |
| Photobleaching during microscopy [2]. | Use mounting medium with antifade; choose photostable dyes (e.g., rhodamine-based) [2]. | |
| High Background | Sample autofluorescence [2]. | Use an unstained control; avoid blue fluorescent dyes; use autofluorescence quenchers [2]. |
| Secondary antibody cross-reactivity [2]. | Use highly cross-adsorbed secondary antibodies; optimize blocking buffers [2]. | |
| Antibody concentration too high [2]. | Perform an antibody titration to find the optimal concentration [2]. | |
| Dark or Poor Contrast | Inappropriate filter set [48]. | Ensure excitation/emission spectra of the filter match the fluorescent reagent [48]. |
| Weak light source or low NA lens [48]. | Use a bright light source (e.g., metal halide lamp) and a lens with a high Numerical Aperture (NA) [48]. | |
| Inappropriate camera settings [48]. | Optimize exposure time, gain, and binning settings on a cooled CCD camera [48]. |
Experimental Protocols & Methodologies
Protocol: Low-Cost, Wide-Field Fluorescent Imaging on a Cell-Phone
This protocol outlines the methodology for constructing and using a cost-effective fluorescent imaging attachment for a mobile phone, suitable for resource-limited settings [101].
1. Principle The sample is pumped by side-coupled LEDs, where the excitation light is guided within the sample cuvette to uniformly illuminate the specimen. The fluorescent emission is collected by an external lens, and a simple plastic colour filter provides the dark-field background necessary for detection [101].
2. Materials and Equipment
- Imaging Platform: A mobile phone with a camera.
- Optical Attachment: Mechanical housing for components.
- Light Source: Battery-powered LEDs (e.g., 3 LEDs for multi-color imaging) [101].
- Emission Filter: Inexpensive plastic colour filter [101].
- External Lens: A single, simple lens positioned in front of the phone's camera lens [101].
- Sample Holder: A cuvette or similar chamber to hold the liquid sample.
3. Procedure 1. Assembly: Mechanically attach the housing unit to the phone's camera. Secure the external lens, emission filter, and LEDs in their respective positions. 2. Sample Preparation: Place the fluorescently labeled sample (e.g., stained white blood cells, water-borne parasites) into the cuvette [101]. 3. Excitation: Activate the battery-powered LEDs, which are butt-coupled to the side of the sample cuvette, guiding light through the sample. 4. Image Acquisition: Use the phone's camera to capture the fluorescent emission from the sample through the external lens and filter. 5. Image Processing (Optional): Apply digital processing algorithms, such as those based on compressive sampling theory, to the captured images to improve the resolving power (e.g., from ~20 μm to ~10 μm) [101].
4. Analysis The raw spatial resolution is approximately 20 μm, which can be digitally enhanced to about 10 μm. This provides a large field-of-view (~81 mm²) suitable for screening large volumes of blood, urine, or water samples [101].
Workflow: Enhancing NIR-II Fluorescence Imaging Contrast
The following diagram illustrates the logical workflow and key considerations for achieving high-contrast fluorescence imaging in the NIR-II window, particularly in challenging spectral regions.
The Scientist's Toolkit: Research Reagent Solutions
The table below details key materials and their functions for fluorescence imaging experiments, particularly in contexts ranging from basic microscopy to advanced in vivo applications.
Table: Essential Materials for Fluorescence Imaging Experiments
| Item | Function & Application | Example Use-Case |
|---|---|---|
| Fluorescent Dyes & Antibodies | Label specific proteins, cell organelles, or structures for visualization. | Immunofluorescence staining of cellular targets; labeling white blood cells in whole blood [101] [2]. |
| NIR-II Fluorophores (e.g., Quantum Dots, Single-Walled Carbon Nanotubes) | Enable deep-tissue in vivo imaging due to reduced scattering and autofluorescence in the NIR-II window [10]. | High-contrast imaging of vasculature or tumors in live animals [10] [102]. |
| Indocyanine Green (ICG) | An FDA-approved NIR-I fluorescent dye used for perfusion assessment and fluorescence-guided surgery [77]. | Real-time visualization of blood flow and tissue perfusion during surgical procedures [77]. |
| Nile Red | A fluorescent dye that stains neutral lipids and certain polymers [103]. | Staining microplastics for detection and classification in a low-cost, portable system [103]. |
| Antifade Mounting Medium | Presves fluorescence by reducing photobleaching caused by exposure to excitation light [2]. | Preparing microscope slides for prolonged or repeated observation. |
| Autofluorescence Quenchers | Reduces nonspecific background signal originating from the sample itself (e.g., lipofuscin in tissues) [2]. | Improving the signal-to-noise ratio in tissue section imaging. |
Data Presentation: Quantitative Comparisons
The following tables summarize key quantitative data from the cited research to facilitate comparison and decision-making.
Table 1: Performance and Cost Analysis of Fluorescence Imaging Platforms
| Platform / Method | Key Performance Metric | Cost Analysis | Reference |
|---|---|---|---|
| Cell-phone-based Wide-field Imager | Raw resolution: ~20 μm (can be improved to ~10 μm digitally). FOV: ~81 mm² [101]. | Component cost: Lens (~$12), Filter (~$1.10), LEDs (~$0.30 each), Battery (~$0.50). Total attachment: ~$14 [101]. | [101] |
| Portable Microplastic Detection System | Mean Average Precision: 94.8%. Processing time: 19 seconds per sample [103]. | Cost per sample: ~$0.10 (77.3% reduction vs. FTIR). Fixed system cost: ~$139 [103]. | [103] |
| Conventional FTIR Method | (Baseline for comparison) | Cost per sample: ~$0.44 [103]. | [103] |
Table 2: Characteristics of Near-Infrared Imaging Windows
| Imaging Window | Wavelength Range | Advantages / Characteristics | Key Challenge |
|---|---|---|---|
| Visible | 400 - 700 nm | Wide range of available fluorophores. | High scattering, strong tissue autofluorescence, shallow penetration [10]. |
| NIR-I | 700 - 900 nm | Deeper penetration than visible light; FDA-approved dyes (e.g., ICG) [10]. | Scattering and autofluorescence still present, limiting depth/resolution [10]. |
| NIR-II | 1000 - 1700 nm | Greatly reduced scattering & autofluorescence; millimeter penetration with micron resolution [10]. | Low quantum yield (QY) of many fluorophores; requires bright probes [10]. |
| NIR-IIb/c & Beyond | 1500 - 2080 nm | Further reduced scattering; strategic use of water absorption (e.g., ~1930 nm) can enhance contrast [102]. | Very high water absorption must be overcome with very bright fluorophores [102]. |
Conclusion
The relentless pursuit to overcome penetration depth limitations is fundamentally expanding the frontiers of fluorescence imaging. The synergistic combination of NIR-II technology, novel probe engineering, and sophisticated computational analysis has demonstrably doubled penetration depths and drastically reduced the required dosages of contrast agents. While challenges in probe biocompatibility and clinical accessibility remain, the validated successes in surgical navigation and preclinical models underscore a clear trajectory toward broader clinical adoption. Future progress hinges on the development of clinically approved NIR-II agents, the standardization of quantitative imaging protocols, and the deeper integration of fluorescence into multimodal and theranostic platforms. For researchers and drug developers, these advances promise not only more refined tools for discovery but also a direct pathway to impacting patient care through precise, real-time visualization of disease.
References
- 1. Fluorescence Fundamentals | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/molecular-probes-the-handbook/introduction-to-fluorescence-techniques.html]
- 2. Troubleshooting Tips for Fluorescence Staining [https://biotium.com/tech-tips-protocols/troubleshooting-tips-for-fluorescence-staining/]
- 3. Cellular Fluorescence Microscopy Troubleshooting & Best ... [https://www.aatbio.com/resources/application-notes/cellular-fluorescence-microscopy-troubleshooting-best-practices]
- 4. Slide scanning: Troubleshooting for fluorescence microscopy [https://www.mbfbioscience.com/help/neurolucida/Content/Ribbons/Acquire/SlideScanLegacy/SlideScan_TroubleshootFluo.htm]
- 5. In vivo fluorescence : success in preclinical imaging paves... imaging [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-022-01648-7]
- 6. High resolution imaging beyond the acoustic diffraction limit in deep... [https://www.nature.com/articles/srep04690?error=cookies_not_supported&code=0a52d958-90b8-46e2-819c-1f822eb3703a]
- 7. In vivo non-invasive confocal fluorescence beyond 1,700 nm... imaging [https://pubmed.ncbi.nlm.nih.gov/35606441/]
- 8. Live-cell fluorescence spectral imaging as a data science ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9043069/]
- 9. Absorption, scattering, and penetration [https://www.lasertherapyinstitute.org/post/absorption-scattering-and-penetration]
- 10. Enhancing the fluorescence emission of the NIR-II ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525000815]
- 11. A review of attenuation correction techniques for tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1618480/]
- 12. Penetration depth [https://en.wikipedia.org/wiki/Penetration_depth]
- 13. Attenuation artifacts in light sheet fluorescence microscopy ... [https://www.nature.com/articles/s41377-018-0068-z]
- 14. An update on recent advances in fluorescent materials for ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03102h]
- 15. Increasing the penetration depth of temporal focusing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7655118/]
- 16. Spectroscopy and Autofluorescence : A Tool for Biomedical... Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC4289852/]
- 17. - Wikipedia Autofluorescence [https://en.wikipedia.org/wiki/Autofluorescence]
- 18. Understanding Fluorescence Depth Sensitivity [https://blog.quelimaging.com/understanding-fluorescence-depth-sensitivity]
- 19. Learn how to Remove Autofluorescence from your ... [https://www.leica-microsystems.com/science-lab/life-science/learn-how-to-remove-autofluorescence-from-your-confocal-images/]
- 20. Background in Fluorescence Imaging [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/molecular-probes-school-of-fluorescence/imaging-basics/protocols-troubleshooting/troubleshooting/background-fluorescence.html]
- 21. Fluorescence depth estimation from wide-field optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5560832/]
- 22. Contribution of autofluorescence from intracellular proteins in... [https://www.nature.com/articles/s41598-022-20857-6?error=cookies_not_supported&code=93f521e9-b3cf-4ea8-a1d6-950332184c15]
- 23. A beginner's guide to rigor and reproducibility in fluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6080651/]
- 24. Signal-to-Noise Considerations [https://evidentscientific.com/en/microscope-resource/knowledge-hub/techniques/confocal/signaltonoise]
- 25. Live-cell fluorescence imaging [https://pubmed.ncbi.nlm.nih.gov/23931505/]
- 26. Overcoming Photobleaching and Phototoxicity in Imaging [https://www.oxinst.com/learning/view/article/how-to-overcome-photobleaching-and-phototoxicity-in-live-cell-imaging]
- 27. Inorganic and hybrid nanomaterials for NIR-II fluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068291/]
- 28. Perfecting and extending the near-infrared imaging window [https://www.nature.com/articles/s41377-021-00628-0]
- 29. Near-Infrared-II (NIR-II) Bioimaging via Off-Peak NIR-I ... [https://www.thno.org/v08p4141.htm]
- 30. Advances in the near-infrared â…¡ for in vivo fluorescence ... [https://www.sciencedirect.com/science/article/abs/pii/S003991402501121X]
- 31. NIR-II-excited off-on-off fluorescent nanoprobes for ... [https://www.nature.com/articles/s41467-024-55096-y]
- 32. Highly Stable and Bright NIR-II AIE Dots for Fluorescence ... [https://pubmed.ncbi.nlm.nih.gov/40500988/]
- 33. Recent Progress in Second Near-Infrared (NIR-II) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405640/]
- 34. Breaking Performance Limits of NIR-II AIEgens for Imaging ... [https://chemrxiv.org/engage/chemrxiv/article-details/68f24b175dd091524f0b2435]
- 35. Clinical Integration of NIR-II Fluorescence Imaging for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384335/]
- 36. Recent Progress in NIR-II Contrast Agent for Biological Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7002322/]
- 37. Nanoprobe-Based Near-Infrared II Optical Imaging for Guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212088/]
- 38. Near-infrared probes for luminescence lifetime imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC8671960/]
- 39. Clearance pathways of near-infrared-II contrast agents - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9706589/]
- 40. Design of AIEgens for near-infrared IIb imaging through ... [https://www.nature.com/articles/s41467-020-15095-1]
- 41. Advances in Optical Contrast Agents for Medical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942650/]
- 42. Carbon quantum dots in bioimaging and biomedicines - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10841552/]
- 43. J-aggregates of meso-[2.2]paracyclophanyl-BODIPY dye for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8062432/]
- 44. Organic dye-based photosensitizers for fluorescence ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854524002121]
- 45. Carbon dots as versatile nanomaterials in sensing and ... [https://www.sciencedirect.com/science/article/pii/S2405844024076655]
- 46. Fluorescent Probes for Imaging in Humans - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10604082/]
- 47. Approved and investigational fluorescent optical imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10442106/]
- 48. Fluorescence Imaging: Causes of Failures and Tips for ... [https://www.keyence.com/products/microscope/fluorescence-microscope/applications/fluorescence-microscope-applications/fluorescence-imaging.jsp]
- 49. Applications of indocyanine green based near-infrared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5179356/]
- 50. Fluorescence-guided surgery: comprehensive review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10183714/]
- 51. Trends and Challenges for the Clinical Adoption of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6581224/]
- 52. An update on recent advances in fluorescent materials for fluorescence molecular imaging: a review - RSC Advances (RSC Publishing) [https://pubs.rsc.org/en/Content/ArticleLanding/2025/RA/D5RA03102H]
- 53. Characterizing the Utility and Limitations of Repurposing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5288741/]
- 54. Sensitivity and depth penetration of continuous wave versus frequency-domain photon migration near-infrared fluorescence contrast-enhanced imaging - PubMed [https://pubmed.ncbi.nlm.nih.gov/12733654/]
- 55. Frequency-Domain Denoising-Based in Vivo Fluorescence ... [https://arxiv.org/abs/2508.02025]
- 56. An update on recent advances in fluorescent materials for ... [https://pubs.rsc.org/en/content/articlelanding/2025/ra/d5ra03102h]
- 57. Image analysis for denoising full-field frequency-domain ... [https://pubmed.ncbi.nlm.nih.gov/19659915/]
- 58. Fluorescence - Optimization and Troubleshooting [https://micro.magnet.fsu.edu/primer/techniques/fluorescence/troubleshoot.html]
- 59. Near-Infrared-II Fluorescence Imaging of Tumors with ... [https://www.mdpi.com/1424-8220/25/22/7080]
- 60. Enhancing biological imaging with high-performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494569/]
- 61. Quantum Dots in Biomedical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6642839/]
- 62. Deep-tissue optical imaging of near cellular-sized features | Scientific Reports [https://www.nature.com/articles/s41598-019-39502-w]
- 63. Exploring the Interplay of Wavelength, Quantum Yield, and Penetration Depth in In Vivo Fluorescence Imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476312/]
- 64. Emerging trends of fluorescence lifetime imaging ... [https://www.biophysics-reports.org/article/doi/10.52601/bpr.2025.250024]
- 65. Confocal Microscopy: Principles and Modern Practices - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6961134/]
- 66. Deriving high contrast fluorescence microscopy images ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8515974/]
- 67. A Guide to Fluorescence Lifetime Imaging Microscopy (FLIM) [https://www.leica-microsystems.com/science-lab/life-science/a-guide-to-fluorescence-lifetime-imaging-microscopy-flim/]
- 68. Troubleshooting Microscope Configuration and Other ... [https://evidentscientific.com/en/microscope-resource/knowledge-hub/photomicrography/errors]
- 69. Basics of Assay Equipment and Instrumentation for High ... [https://www.ncbi.nlm.nih.gov/books/NBK92014/]
- 70. High Throughput Screening Instrumentation [https://cidd.uthscsa.edu/core-facilities/hts-core/instrumentation/]
- 71. High-fidelity tissue super-resolution imaging achieved with confocal2 spinning-disk image scanning microscopy | Light: Science & Applications [https://www.nature.com/articles/s41377-025-01930-x]
- 72. High contrast fluorescence polarization microscopy ... [https://www.nature.com/articles/s44303-025-00094-y]
- 73. Recent advances of versatile fluorophores for multifunctional... [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d4tb01957a]
- 74. Optimal Dosing Strategy for Fluorescence-Guided Surgery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7017887/]
- 75. Optimal Dosing Strategy for Fluorescence-Guided Surgery ... [https://pubmed.ncbi.nlm.nih.gov/31054001/]
- 76. FAQ - MolecuLight US [https://us.moleculight.com/faq/]
- 77. Fluorescence Guided Surgery Frequently Asked Questions [https://diagnosticgreen.com/am/frequently-asked-questions/frequently-asked-questions-fluorescence-guided-surgery/]
- 78. Organic probes for NO-activatable biomedical imaging: NIR ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc03611a?page=search]
- 79. Advances in multimodal imaging techniques in nanomedicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308829/]
- 80. Photoacoustic clinical imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6595011/]
- 81. Molecular imaging using (nano)probes - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257482/]
- 82. Advancements in photoacoustic detection techniques for ... [https://www.nature.com/articles/s44384-025-00005-w]
- 83. Statistics further pushes the limits of optical microscopy [https://physicstoday.aip.org/news/statistics-further-pushes-the-limits-of-optical-microscopy]
- 84. Cell Imaging Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/cell-analysis-support-center/cell-imaging-support/cell-imaging-support-troubleshooting.html]
- 85. Visualization of Color Anatomy and Molecular Fluorescence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3049862/]
- 86. A framework to enhance the signal-to-noise ratio ... [https://pubmed.ncbi.nlm.nih.gov/40906681/]
- 87. A framework to enhance the signal-to-noise ratio for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330718]
- 88. Harmonized technical standard test methods for quality evaluation of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11723869/]
- 89. Optimization and Troubleshooting [https://evidentscientific.com/en/microscope-resource/knowledge-hub/techniques/fluorescence/troubleshoot]
- 90. Optimizing Fluorescence Imaging Through Scattering ... [https://www.sciencedirect.com/science/article/pii/S2589004225016906]
- 91. Fluorescence Microscopy Imaging Solutions [https://www.spotimaging.com/bioresearch-imaging/fluorescence-imaging-for-bioresearch/]
- 92. SearchLight Fluorescence Spectrum Modeling Tool from ... [https://searchlight.idex-hs.com/Welcome]
- 93. New algorithmic tool can improve microscopy image analysis ... [https://medschool.vanderbilt.edu/basic-sciences/2025/10/06/new-algorithmic-tool-can-improve-microscopy-image-analysis-making-improvements-across-fields/]
- 94. 5-ALA Fluorescence-Guided Surgery vs. Conventional White ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191055/]
- 95. Comparison of fluorescein sodium, 5-ALA, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0967586822000819]
- 96. Immunofluorescence Troubleshooting | Tips & Tricks [https://www.stressmarq.com/support/technical-support/troubleshooting/immunofluorescence-troubleshooting/?srsltid=AfmBOordBJaxti0bMozLxSmtOMmnsOFy1thrcVgY09QsIOI1JeIyFkvz]
- 97. Preliminary safety and imaging efficacy of the near-infrared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7299531/]
- 98. Gold nanoclusters performing as contrast agents for non- ... [https://pubs.rsc.org/en/content/articlelanding/2021/an/d1an01394g]
- 99. Fluorescence Microscopy Errors [https://evidentscientific.com/en/microscope-resource/knowledge-hub/photomicrography/fluorescenceerrors]
- 100. Fluorescence Lifetime Imaging Microscopy Using Near- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3607809/]
- 101. Cost-effective and compact wide-field fluorescent imaging on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3073081/]
- 102. High-contrast in vivo fluorescence imaging exploiting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075662/]
- 103. Low-cost portable microplastic detection system integrating ... [https://www.sciencedirect.com/science/article/pii/S2772416625001986]