Quantitative Light-Induced Fluorescence (QLF): A Comprehensive Guide for Researchers on Dental Biofilm Imaging and Analysis
This article provides a scientific overview of Quantitative Light-Induced Fluorescence (QLF) technology for dental biofilm imaging, tailored for researchers, scientists, and drug development professionals.
Quantitative Light-Induced Fluorescence (QLF): A Comprehensive Guide for Researchers on Dental Biofilm Imaging and Analysis
Abstract
This article provides a scientific overview of Quantitative Light-Induced Fluorescence (QLF) technology for dental biofilm imaging, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of QLF, focusing on its mechanism of detecting bacterial porphyrins and quantifying fluorescence. The scope covers methodological protocols for in vivo and in vitro applications, including analysis of key parameters like ΔF and ΔR. It addresses technological limitations and optimization strategies and offers a critical evaluation of QLF's diagnostic performance against established standards and conventional methods. The content synthesizes current evidence to validate QLF as a precise tool for oral biofilm quantification in clinical research and therapeutic development.
The Science of Red Fluorescence: Exploring QLF's Core Principles for Biofilm Detection
The interaction of light at a 405 nm wavelength with dental bioforms is the fundamental basis of Quantitative Light-induced Fluorescence (QLF) technology. This specific wavelength, situated in the blue-violet spectrum, is optimally absorbed by certain bacterial metabolites within the biofilm, primarily porphyrins [1] [2]. Following absorption, these molecules undergo a process whereby they emit light at longer, lower-energy wavelengths—a phenomenon known as biofluorescence [3] [1]. The emitted fluorescence manifests as red fluorescence (RF), which is visually distinct from the greenish autofluorescence of sound tooth structure [4] [2]. The primary optical principle exploited by QLF is that the intensity of this red fluorescence is directly correlated with the metabolic activity and quantity of cariogenic bacteria within the biofilm, allowing for quantitative assessment [3] [5].
Quantitative Performance Data
The diagnostic accuracy of 405 nm-induced biofluorescence for detecting various oral conditions has been validated across multiple studies. The tables below summarize key quantitative findings.
Table 1: Diagnostic Accuracy of QLF for Caries Detection (In Vivo Data) [4]
| Lesion Type & Location | Pooled Sensitivity | Pooled Specificity | AUC Range |
|---|---|---|---|
| Occlusal Caries | 0.86 | 0.82 | 0.94 - 0.98 |
| Approximal Caries | 0.74 | 0.82 | 0.67 - 0.91 |
| Incipient Occlusal Enamel Lesions | 0.76 - 0.91 | 0.74 - 0.93 | 0.81 - 0.93 |
Table 2: Correlation between Biofluorescence and Periodontal Indices [3]
| Gingival Health Index | Correlation with Fluorescent Biofilm Area (r-value) |
|---|---|
| Gingival Index (GI) | 0.422 |
| Bleeding on Probing (BOP) | 0.376 |
| Plaque Index (PI) | 0.499 |
Table 3: Red Fluorescence Intensity (ΔR) for Calculus Detection [6]
| Calculus Severity | Mean ΔR (%) |
|---|---|
| No Calculus | 2.75% |
| Initial Calculus | 6.06% |
| Advanced Calculus | 15.58% |
Experimental Protocols
Protocol: In Vivo Assessment of Dental Plaque and Gingival Health
This protocol details the use of QLF for correlating biofilm fluorescence with gingival health status [3].
- Subject Preparation: Participants should refrain from oral hygiene procedures (brushing, flossing) for a minimum of 4-8 hours prior to imaging to allow for initial plaque accumulation.
- Image Acquisition:
- Use a QLF imaging device such as the Qraycam Pro.
- Ensure the room lights are dimmed to minimize ambient light interference.
- Capture fluorescence images of the upper and lower anterior teeth. The device emits light at 405 nm and captures the resulting fluorescence through a specialized filter.
- Ensure the focal distance and angle are consistent across imaging sessions.
- Image Analysis:
- Transfer images to proprietary software for analysis.
- The software automatically calculates the percentage of the total anterior tooth surface area that exhibits red biofluorescence.
- Clinical Validation:
- A trained clinician performs standard clinical assessments, including the Silness-Löe Plaque Index (PI), Löe-Silness Gingival Index (GI), and Bleeding on Probing (BOP) at relevant sites.
- Data Correlation:
- Statistically correlate the calculated fluorescent biofilm area with the clinical indices (GI, BOP, PI) using Pearson's correlation analysis or logistic regression.
Protocol: Tongue Biofilm Quantification using the Tongue Biofilm Fluorescence Index (TBFI)
This protocol standardizes the assessment of tongue biofilm pathogenicity based on fluorescence [5].
- Baseline Imaging:
- Acquire a baseline (T0) intraoral scan (IOS) or QLF image of the clean dorsal tongue surface after professional prophylaxis.
- Plaque Regrowth:
- Instruct subjects to abstain from all mechanical and chemical oral hygiene for 4 days to allow for plaque regrowth.
- Post-Regrowth Imaging (T4):
- Capture a second QLF image or IOS of the dorsal tongue after the 4-day period.
- TBFI Scoring:
- Evaluate the fluorescence image based on two parameters:
- Coverage (C): The extent of the dorsal tongue surface covered by red fluorescent biofilm.
- 0: No coverage
- 1: ≤50% coverage
- 2: >50% coverage
- Intensity (I): The brightness of the red fluorescence, indicative of biofilm thickness and metabolic activity.
- 0: No fluorescence
- 1: Faint pink fluorescence
- 2: Bright red fluorescence
- Coverage (C): The extent of the dorsal tongue surface covered by red fluorescent biofilm.
- The final TBFI score is the sum of C and I, ranging from 0 to 4.
- Evaluate the fluorescence image based on two parameters:
- Validation:
- Validate TBFI scores by measuring concentrations of volatile sulfur compounds (H₂S and CH₃SH) using a portable gas chromatograph, which show a significant positive correlation with TBFI.
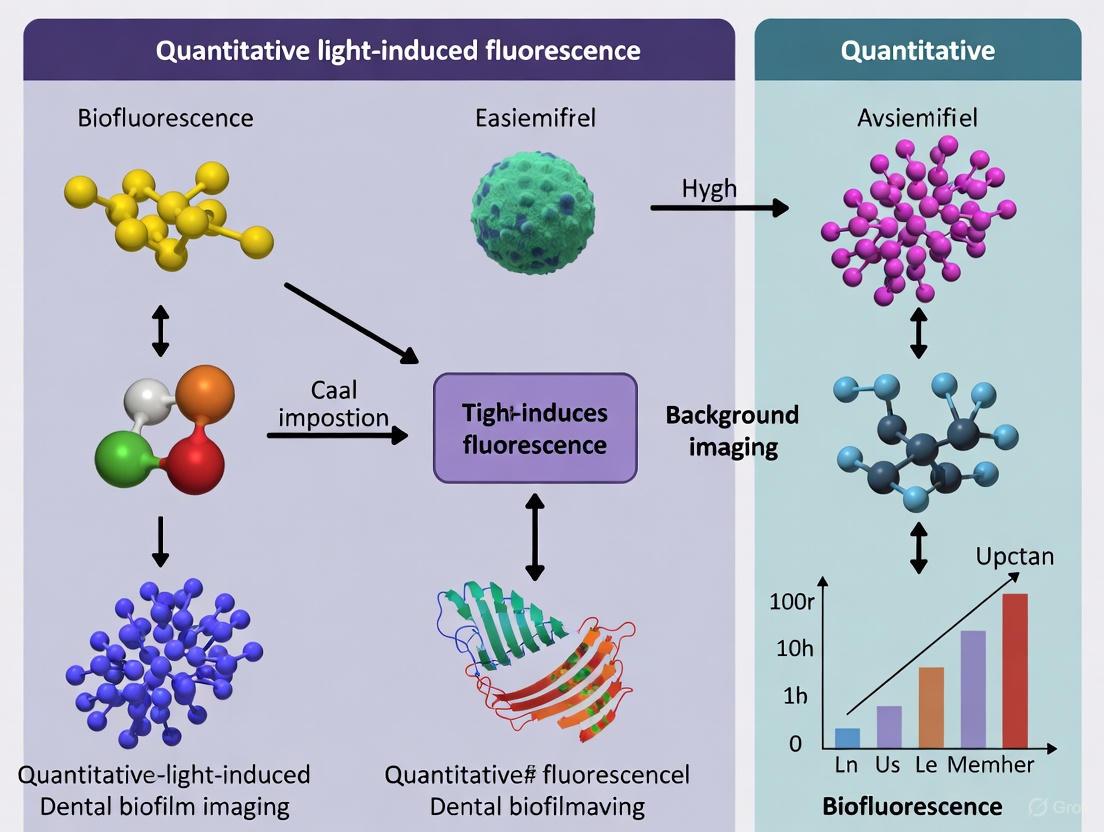
Visualization and Workflows
The following diagrams illustrate the core principles and experimental workflows.
Light-Biofilm Interaction at 405 nm
Plaque and Gingivitis Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Reagents for QLF Biofilm Research
| Item | Function / Application in Research |
|---|---|
| QLF-D Biluminator / Qraycam Pro | Core imaging device providing standardized 405 nm illumination and filtered capture of fluorescence for in vivo and in vitro studies [4] [3]. |
| Proprietary Analysis Software | Used for quantitative analysis of fluorescence parameters, including ΔF (fluorescence loss for caries) and ΔR (red fluorescence gain for biofilm) [4]. |
| Intraoral Scanner (IOS) | Enables 3D volumetric assessment of plaque accumulation by comparing superimposed scans taken at baseline and post-regrowth [7]. |
| Two-Tone Disclosing Agent | Used as a visual reference standard (e.g., for validating volumetric plaque indices) to distinguish between new (pink) and mature (blue/purple) plaque [7]. |
| Specialized Nucleases | Research tools for investigating the role of extracellular DNA (eDNA) in biofilm integrity. DNase I is ineffective against mature biofilms; experimental nucleases targeting Z-DNA/G-quadruplexes are used [8]. |
| Confocal Microscopy with Immunolabelling | Advanced technique for visualizing specific non-canonical DNA structures (e.g., Z-DNA, G-quadruplexes) within the biofilm matrix that confer resistance to degradation [8]. |
Porphyrins are a class of naturally occurring organic compounds that play a critical role in numerous biological processes, serving as the foundational structures for heme, chlorophyll, and vitamin B12. In many bacterial species, porphyrins are synthesized as intermediates in the heme biosynthesis pathway and subsequently accumulate as endogenous photosensitizers. These molecules exhibit a distinctive optical property: when illuminated with violet or blue light (typically around 405 nm), they emit a characteristic red fluorescence. This phenomenon serves as a key biomarker for detecting and visualizing bacterial presence in diverse environments, from carious dental lesions to infected wounds [9] [10] [11].
The underlying mechanism involves the excitation of the porphyrin's conjugated π-electron system. Specific bacterial metabolites, including protoporphyrin IX (PPIX) and coproporphyrin I (CPI), are primarily responsible for this fluorescence signal [10]. The detection of this red fluorescence has been successfully leveraged in clinical and research settings through technologies such as Quantitative Light-induced Fluorescence (QLF) for dental caries detection and various imaging systems for identifying wound pathogens [9] [11].
Metabolic Pathways and Bacterial Synthesis of Porphyrins
In bacteria, porphyrins are synthesized via the heme biosynthesis pathway. Heme serves as a prosthetic group in proteins involved in electron transport (cytochromes), catalase reactions, and oxygen sensing. The pathway begins with glycine and succinyl-CoA and proceeds through several enzymatic steps to produce the intermediate compounds that accumulate and fluoresce.
table 1: Key Bacterial Porphyrins and Their Fluorescent Properties
| Porphyrin Type | Role in Bacterial Metabolism | Excitation Peak (nm) | Emission Peak (nm) | Notable Producing Organisms |
|---|---|---|---|---|
| Protoporphyrin IX (PPIX) | Immediate precursor to heme | ~405 nm | ~635 nm & ~705 nm | Helicobacter pylori, various oral bacteria |
| Coproporphyrin I (CPI) | Tetrapyrrole intermediate | ~405 nm | ~615 nm & ~620 nm | Cutibacterium acnes, Streptococci |
| Uroporphyrin III | Early tetrapyrrole intermediate | ~405 nm | ~615 nm & ~620 nm | Various anaerobic bacteria |
The diagram below illustrates the core metabolic pathway leading to the accumulation of fluorescent porphyrins in bacteria.
Bacterial metabolism can be perturbed by environmental factors, leading to an accumulation of PPIX and CPI. When the metabolic flow to heme is disrupted—due to iron limitation, specific genetic mutations, or the action of antimicrobial agents—these porphyrin precursors build up within the cell. Once a critical concentration is reached, they can also be released into the extracellular matrix of a biofilm. This accumulation is the primary source of the red fluorescence signal exploited in diagnostic imaging [10] [12].
Detection Methodologies and Imaging Technologies
The unique spectral signature of bacterial porphyrins enables their detection through several advanced optical technologies. The fundamental principle involves exciting the molecules with violet light and capturing the resulting red fluorescence, which can then be quantified and analyzed.
Quantitative Light-Induced Fluorescence (QLF) in Dental Research
In the context of dental biofilm imaging, QLF technology utilizes a 405 nm blue-violet light source to illuminate the tooth surface. A specialized camera with a yellow high-pass filter (typically blocking light below 520 nm) captures the resulting fluorescence. Sound tooth enamel emits a strong green autofluorescence, while carious lesions appear as dark areas due to a loss of this signal (ΔF). Crucially, dental biofilms and certain caries exhibit red fluorescence (ΔR), which is quantitatively linked to the presence of porphyrin-producing bacteria within the plaque and lesions [9] [13] [14].
table 2: Key Parameters in QLF Analysis for Dental Biofilm and Caries Detection
| QLF Parameter | Description | Biological Correlation | Typical Range/Values |
|---|---|---|---|
| ΔF (Delta F) | Percentage loss of green autofluorescence | Demineralization and mineral loss in enamel | Can exceed 5% in early caries |
| ΔR (Delta R) | Gain of red fluorescence | Presence and concentration of bacterial porphyrins in biofilm | Positively correlated with carious lesion severity |
| AUROC (Area Under ROC) | Diagnostic accuracy for caries detection | Ability to distinguish sound vs. carious surfaces | Occlusal: 0.92-0.99 (in vivo); Approximal: 0.56-0.67 (in vivo) [9] |
The following workflow outlines the standard procedure for capturing and analyzing red fluorescence in a dental research context.
Fluorescence Lifetime Imaging Microscopy (FLIM)
Beyond intensity-based measurements, FLIM provides an additional layer of specificity by measuring the average time a fluorophore remains in its excited state. The fluorescence lifetime of porphyrins is sensitive to their molecular environment and aggregation state. For example, PPIX in an organic solution has a lifetime of about 16.4 ns, while in the complex milieu of a bacterial biofilm, its lifetime can be shorter and heterogeneous. FLIM-phasor analysis can map the distribution of different porphyrin species within a biofilm, distinguishing between those inside bacterial cells and those dispersed in the extracellular matrix [10] [15]. This technique is particularly powerful for optimizing antimicrobial Photodynamic Therapy (aPDT), as it precisely localizes the photosensitizers [10].
Wearable and Hands-Free Fluorescence Imaging
Recent technological advances have led to the development of compact, wearable imaging systems for point-of-care detection. These devices, such as the REVEAL FC system, incorporate a 405 nm violet excitation headlight and eyewear with 430 nm emission lenses, allowing for rapid, non-invasive assessment of wound infections based on bacterial porphyrin fluorescence [11]. Studies have demonstrated that this method can detect porphyrin-specific red fluorescence in a wide range of pathogenic bacteria, including those commonly associated with skin and oral infections [11].
Experimental Protocols
Protocol: In Vitro Detection of Bacterial Porphyrins on Agar Plates
This protocol is adapted from methods used to test a wearable fluorescence imaging system [11].
Research Reagent Solutions & Materials: table 3: Essential Reagents for Porphyrin Fluorescence Experiments
| Reagent/Material | Function/Description | Example Source/Type |
|---|---|---|
| Porphyrin Test Agar | Selective medium that enhances porphyrin production in bacteria. | Remel Porphyrin Test Agar |
| Blood Agar Plates | General-purpose medium supporting growth of various pathogens; allows comparison of porphyrin production. | Defibrinated sheep blood agar |
| Bacterial Strains | Test organisms of interest, e.g., from skin, oral, or wound infections. | Staphylococcus aureus, Pseudomonas aeruginosa, oral Streptococci |
| Wearable Fluorescence Imager | Device for hands-free visualization and documentation of red fluorescence. | REVEAL FC system or equivalent (405 nm excitation) |
| Anaerobic Chamber/Gas Pak | For creating anaerobic conditions to support growth of obligate anaerobes. | Commercially available systems |
Procedure:
- Inoculation: Streak the bacterial strains of interest onto separate sections of Porphyrin Test Agar and Blood Agar plates to obtain isolated colonies.
- Incubation: Incubate the plates under appropriate atmospheric conditions (aerobic, microaerophilic, or anaerobic) at 37°C for 24-72 hours. Some strains may require extended incubation for optimal porphyrin production.
- Imaging: After incubation, visualize the plates in a darkroom or using a device designed to block ambient light.
- Use the wearable imager with the 405 nm excitation source.
- Observe and photograph the plates through the 430 nm long-pass emission filter.
- Analysis: Look for the emission of distinct red fluorescence directly from the bacterial colonies. Compare the fluorescence intensity between different strains and between the two types of growth media.
Protocol: QLF Imaging and Analysis of Dental Biofilm
This protocol details the process for quantifying red fluorescence from dental biofilms in a research context [9] [13].
Materials:
- QLF imaging device (e.g., QRaypen C, QRaycam Pro, or QLF-D Biluminator).
- Compatible analysis software (e.g., QA2).
- Standardized calibration tool for the device.
- Standardized positioning jig for in vitro studies.
Procedure:
- Sample Preparation:
- For in vivo studies, instruct patients to refrain from oral hygiene procedures for 12-24 hours prior to imaging to allow for biofilm accumulation.
- For in vitro studies, grow multi-species biofilms on tooth specimens or relevant substrates for a defined period.
- Image Acquisition:
- Stabilize the patient's head or the in vitro specimen in a fixed position.
- In a dimmed environment, position the QLF probe perpendicular to the tooth/biofilm surface at a standardized distance.
- Capture the fluorescence image. Ensure the image is in focus and the entire region of interest is within the frame.
- Image Analysis:
- Import the image into the analysis software.
- For ΔF analysis (mineral loss): Define a patch on the sound enamel surrounding the lesion. The software will interpolate the sound fluorescence values and calculate the percentage of fluorescence loss (ΔF) within the lesion.
- For ΔR analysis (porphyrin presence): Select the same lesion area. The software will quantify the increase in red fluorescence signal relative to the background.
- Data Validation:
- Correlate the QLF parameters (ΔF, ΔR) with standard diagnostic methods. Common reference standards include:
- ICDAS II (International Caries Detection and Assessment System) for visual-tactile scoring.
- Microbiological analysis (e.g., colony-forming unit counts of specific bacteria).
- Histological validation for in vitro studies (e.g., determining lesion depth).
- Correlate the QLF parameters (ΔF, ΔR) with standard diagnostic methods. Common reference standards include:
Applications in Research and Drug Development
The detection of bacterial porphyrins via red fluorescence has significant implications across multiple fields.
- Clinical Dentistry: QLF serves as a non-invasive tool for the early detection of carious lesions and the assessment of biofilm activity. Its high diagnostic accuracy for occlusal caries (AUROC up to 0.99) enables monitoring of lesion progression and the efficacy of anti-caries agents like toothpaste or mouthwashes in clinical trials [9] [13].
- Wound Care Diagnostics: Wearable fluorescence imagers allow clinicians to rapidly identify and localize pathogenic bacteria in chronic wounds, facilitating targeted debridement and sampling. This real-time guidance can improve treatment outcomes and minimize contamination risk [11].
- Antimicrobial Drug Development: Red fluorescence can be used as a biomarker to screen the efficacy of novel antimicrobial compounds or aPDT protocols. A reduction in fluorescence signal in treated bacterial cultures or biofilms indicates a decrease in bacterial metabolic activity or viability [10] [15].
- Basic Microbiology Research: FLIM and spectroscopic analysis of porphyrins provide insights into the metabolic state of bacteria, the structure of biofilms, and the interactions between exogenous photosensitizers and endogenous porphyrins, which is crucial for optimizing aPDT [10] [12].
Within the framework of broader thesis research on quantitative light-induced fluorescence (QLF) for dental biofilm imaging, this document serves as a technical primer on its core output parameters. QLF technology leverages the natural fluorescence of dental tissues and the metabolic byproducts of bacteria, providing non-invasive, quantitative metrics for oral health research and therapeutic development [4] [16]. It operates on two primary principles: the loss of natural green autofluorescence due to demineralization and the gain of red fluorescence from bacterial metabolites [4]. This note details the parameters ΔF, ΔR, and ΔQ, which quantify these phenomena, and provides standardized protocols for their application in a research setting.
Core QLF Output Parameters: Definitions and Interpretations
The diagnostic power of QLF is encapsulated in three primary quantitative parameters. Understanding their individual and combined significance is crucial for accurate data interpretation.
ΔF: The Demineralization Indicator
- Definition: ΔF (%) represents the percentage loss of natural green autofluorescence from a tooth surface relative to sound (healthy) enamel. This loss occurs because carious demineralization increases light scattering, reducing the emitted fluorescence that reaches the detector [4] [16].
- Interpretation: A more negative ΔF value indicates a greater degree of demineralization and thus, a more severe carious lesion. It is primarily used to assess mineral loss in enamel caries. For example, a ΔF of -10% signifies a more advanced lesion than a ΔF of -5%.
ΔR: The Bacterial Activity Indicator
- Definition: ΔR (%) quantifies the increase in red fluorescence emitted from a tooth surface. This signal originates from porphyrins, which are metabolites produced by many cariogenic bacteria within dental biofilms [4] [16] [17].
- Interpretation: A positive ΔR value indicates the presence and metabolic activity of bacterial biofilms. Higher ΔR values are strongly correlated with more mature, pathogenic dental plaque [18]. This parameter is also used to assess bacterial load on the tongue, providing a link to oral malodor research [17].
ΔQ: The Lesion Volume Index
- Definition: ΔQ (mm² × % or %µm²) is a composite parameter representing the total lesion volume. It is calculated as the product of the average fluorescence loss (ΔF) and the size of the demineralized area (in mm²) [19].
- Interpretation: ΔQ provides a more comprehensive assessment of the lesion's burden than ΔF alone, as it integrates both the depth (severity) and the surface extent of the demineralization. It is particularly valuable for monitoring lesion progression or regression over time in longitudinal studies [19].
Table 1: Core QLF Output Parameters and Their Diagnostic Significance
| Parameter | Full Name | Physical Meaning | Primary Diagnostic Indication | Representation in Sound Tissue |
|---|---|---|---|---|
| ΔF | Delta F | Loss of green autofluorescence | Degree of enamel demineralization [16] | ~0% |
| ΔR | Delta R | Gain of red fluorescence | Level of bacterial activity/biofilm presence [16] [18] | ~0% |
| ΔQ | Delta Q | Lesion volume | Integrated measure of lesion size and severity [19] | 0 (mm² × %) |
Quantitative Data Synthesis from Clinical and Preclinical Studies
Extensive research has validated the diagnostic accuracy of these parameters across various caries types and study designs. The following tables synthesize key performance data from recent systematic reviews and clinical studies.
Table 2: Diagnostic Accuracy of QLF for Various Lesion Types (Meta-Analysis Data) [4]
| Lesion Type / Dentition | Study Setting | Pooled Sensitivity | Pooled Specificity | Area Under Curve (AUC) Range |
|---|---|---|---|---|
| Occlusal Caries | In vivo | 0.86 | 0.82 | 0.94 - 0.98 |
| Occlusal Caries | In vitro | 0.83 | 0.74 | 0.71 - 0.97 |
| Approximal Caries | In vivo | 0.74 | 0.82 | 0.67 - 0.91 |
| Approximal Caries | In vitro | 0.83 | 0.74 | 0.80 - 0.91 |
Table 3: Representative QLF Parameter Values from Clinical Studies
| Study Focus | ΔF (ΔFmax) in Lesions | ΔR (ΔRmax) in Lesions | Key Findings | Citation |
|---|---|---|---|---|
| Occlusal Caries & Cracks | |ΔFmax| = 15.3% (AUC: 0.84) | ΔRmax = 11.5% (AUC: 0.91) | ΔRmax showed superior performance for occlusal caries detection compared to |ΔFmax|. | [16] |
| Plaque Maturation | Not Reported | R/G Ratio: Score 0: 1.07; Score 1: 1.31; Score 2: 1.65 | Red fluorescence intensity (R/G ratio) strongly correlates with plaque maturity (p<0.001). | [18] |
| Root Caries Monitoring | ΔF = -9.8% to -12.1% (over 24 mos) | ΔR = ~15% (baseline) | Professional prevention stabilized ΔF and reduced ΔR for 12 months post-treatment. | [19] |
Experimental Protocols for QLF Analysis
Standardized protocols are essential for generating reliable, reproducible QLF data. The following sections detail methodologies for in vitro and in vivo applications.
Protocol: In Vitro Detection of Caries on Extracted Teeth
This protocol is adapted from methodologies used in controlled laboratory studies [4].
1. Sample Preparation:
- Source: Obtain extracted human teeth (permanent or primary) with ethical approval.
- Inclusion: Select teeth with sound surfaces and various stages of carious lesions, confirmed by a reference standard (e.g., histology, ICDAS ≥3) [20].
- Cleaning and Storage: Clean teeth of soft tissue and blood. Store in thymol-saturated saline or distilled water at 4°C to prevent dehydration.
- Mounting: Embed teeth in acrylic resin or modeling clay, ensuring the surface of interest is exposed and reproducible for imaging.
2. QLF Image Acquisition:
- Device Setup: Use a QLF device (e.g., QLF-Clin, Inspektor Pro, QLF-D, Qraypen C). Ensure the device is calibrated according to manufacturer specifications.
- Environment: Conduct imaging in a darkroom to eliminate ambient light interference.
- Positioning: Secure the sample. Position the QLF probe perpendicular to the tooth surface, maintaining a consistent distance (e.g., 5-10 mm, as per device manual).
- Drying: Gently air-dry the tooth surface for 3-5 seconds to remove saliva-mimicking moisture.
- Capture: Acquire both the fluorescence (for ΔF/ΔR analysis) and white-light (for visual reference) images. Save images in a lossless format (e.g., BMP).
3. Image Analysis:
- Software: Use proprietary analysis software (e.g., QA2 from Inspektor Research Systems).
- ROI Selection: Manually outline the sound enamel reference area adjacent to the lesion.
- Parameter Calculation: The software automatically calculates and applies the fluorescence loss of the sound area to the lesion, generating values for ΔF, ΔR, and ΔQ.
- Data Export: Export numerical data for statistical analysis.
Protocol: In Vivo Monitoring of Dental Plaque and Gingival Health
This protocol is designed for clinical studies involving human participants [3] [18].
1. Participant Preparation and Inclusion:
- Ethics: Obtain approval from the Institutional Review Board (IRB) and written informed consent from all participants.
- Inclusion Criteria: Recruit adults (e.g., ≥20 years) with gingivitis or varying levels of plaque accumulation.
- Exclusion Criteria: Exclude participants with systemic diseases affecting oral health, those who have undergone recent antibiotic therapy, or those with orthodontic appliances that obstruct imaging.
- Pre-imaging Protocol: Ask participants to refrain from eating, drinking, or oral hygiene procedures for at least 2 hours prior to the examination.
2. QLF Image Acquisition:
- Device: Use a clinically approved intraoral QLF device (e.g., Qraycam Pro, Qraypen C).
- Clinical Setting: Perform imaging in a dental chair. Use a cheek retractor for better access and visibility.
- Site Selection: Focus on anterior teeth for efficient plaque screening [3] or specific teeth/roots selected for monitoring [19].
- Procedure: Dry the tooth surfaces gently with compressed air. Capture QLF images of the labial surfaces of the upper and lower anterior teeth, ensuring the entire surface is in focus.
3. Image and Data Analysis:
- Plaque Quantification (SPS): Use dedicated software to calculate the Simple Plaque Score (SPS), which determines the percentage of tooth area covered by red-fluorescing plaque.
- Advanced Plaque Assessment: For maturation analysis, calculate the Red/Green (R/G) ratio from the RGB values of specific regions of interest (ROIs). Correlate this with two-tone disclosing solution results (pink stain = young plaque; blue stain = mature plaque) [18].
- Gingival Health Correlation: Correlate the fluorescent biofilm area with clinical indices like the Gingival Index (GI) and Bleeding on Probing (BOP) using statistical tests (e.g., Pearson's correlation, logistic regression) [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Materials and Reagents for QLF-Based Research
| Item | Specification / Example | Research Function | Citation |
|---|---|---|---|
| QLF Device | Qraypen C, Qraycam Pro, QLF-D | Captures white-light and fluorescence (405 nm) intraoral images for analysis. | [3] [20] [16] |
| Analysis Software | QA2 (Inspektor Research Systems), TB01 Analyzer | Quantifies core parameters (ΔF, ΔR, ΔQ) and calculates plaque coverage from images. | [17] [19] |
| Reference Standards | International Caries Detection and Assessment System (ICDAS), Histology | Provides a validated benchmark for calibrating QLF measurements and validating caries detection. | [4] [20] |
| Disclosing Solution | Two-tone disclosing agent (e.g., stains young plaque pink, mature plaque blue) | Validates and correlates red fluorescence (ΔR) with the biological maturity of dental plaque. | [18] |
| Calibration Standards | Manufacturer-provided fluorescence standards | Ensures inter-device reproducibility and longitudinal consistency of fluorescence measurements. | [16] |
Workflow and Logical Diagrams
The following diagram illustrates the logical pathway from image acquisition to data interpretation in a QLF analysis workflow.
The fundamental principles of QLF technology, showing how light interaction with dental tissues and biofilms generates the signals for key parameters, are shown in the following diagram.
Correlating Fluorescence with Biofilm Maturation and Pathogenicity
Within the context of quantitative light-induced fluorescence (QLF) dental biofilm imaging research, the intrinsic fluorescence of bacterial communities serves as a powerful, non-destructive indicator of both biofilm development and pathogenic potential. As biofilms mature, their metabolic activity and structural complexity increase, leading to characteristic changes in fluorescence signatures that can be quantified in real-time. A key phenomenon is the emission of red fluorescence (RF), which is largely attributed to bacterial porphyrins, intermediates in the heme synthesis pathway [21]. The correlation between the intensity of this red fluorescence and biofilm pathogenicity provides a critical tool for researchers and drug development professionals seeking to screen for antimicrobial compounds and evaluate treatment efficacy. This application note details the quantitative relationships, experimental protocols, and analytical tools for leveraging fluorescence in biofilm studies.
Key Quantitative Correlations
Research across multiple domains, from dental plaques to wound biofilms, has consistently demonstrated strong correlations between fluorescence signals, biofilm maturity, and markers of pathogenicity. The tables below summarize the key quantitative relationships established in the literature.
Table 1: Correlations between Red Fluorescence and Biofilm Maturation
| Biofilm Model | Fluorescence Metric | Correlation with Maturation Markers | Statistical Significance | Source |
|---|---|---|---|---|
| Dental Microcosm | Red/Green Ratio (R/G value) | Positive correlation with total bacterial CFUs (r=0.74) | p=0.001 | [22] |
| Dental Microcosm | Red/Green Ratio (R/G value) | Positive correlation with aciduric bacterial CFUs (r=0.85) | p=0.001 | [22] |
| Dental Microcosm | Red/Green Ratio (R/G value) | Positive correlation with enamel lesion depth (r=0.82) | p=0.001 | [22] |
Table 2: Correlations between Red Fluorescence and Clinical Pathogenicity Indicators
| Biofilm Context | Fluorescence Metric | Correlation with Pathogenicity | Statistical Significance | Source |
|---|---|---|---|---|
| Gingival Health | Red Biofluorescence Area | Positive correlation with Gingival Index (r=0.422) and Bleeding-on-Probing (r=0.376) | p<0.05 | [23] |
| Tongue Coating | Tongue Biofilm Fluorescence Index (TBFI) | Positive correlation with Hydrogen Sulfide (H₂S) levels (r=0.369) | p<0.01 | [5] |
| In Vivo Wound Biofilms | Red Fluorescence Intensity | Detection of porphyrin-producing bacteria (e.g., S. aureus, E. coli) in planktonic and biofilm states | N/A | [21] |
Experimental Protocols
Protocol: Monitoring Biofilm Maturation Using QLF-D
This protocol outlines the procedure for growing dental microcosm biofilms and using QLF-D to non-destructively monitor their maturation and increasing cariogenicity via red fluorescence [22].
Workflow Overview
Materials and Reagents
- Human saliva as an inoculum to establish a microcosm biofilm.
- Bovine enamel discs as the substrate for biofilm growth.
- Growth media supplemented with 0.5% sucrose to promote cariogenic biofilm development.
- QLF-D device (Qraycam Pro) for capturing fluorescence and white-light images.
Procedure
- Biofilm Initiation: Centrifuge fresh, stimulated human saliva and resuspend the pellet in growth medium. Inoculate sterile bovine enamel discs with this suspension and incubate anaerobically for 8 hours to allow for initial adhesion.
- Biofilm Maturation: Transfer the inoculated discs to a new plate with fresh growth medium containing 0.5% sucrose. Refresh the medium daily to simulate oral conditions and provide nutrients. Continue incubation under anaerobic conditions for up to 10 days.
- QLF-D Imaging: At predetermined time points (e.g., days 1, 2, 3, 7, and 10), remove biofilms from the incubator. Capture fluorescence images using the QLF-D device according to the manufacturer's instructions. Ensure consistent imaging parameters (exposure, distance) across all time points.
- Image Analysis: Use the proprietary software accompanying the QLF-D device to analyze the images. Calculate the red-to-green ratio (R/G value) for each biofilm, which quantifies the intensity of red fluorescence relative to the green background.
- Validation (Destructive Assays): In parallel, at each time point, harvest replicate biofilms for destructive analyses to validate the fluorescence data.
- Microbiological Analysis: Homogenize the biofilm, perform serial dilution, and plate on appropriate agars to determine the total viable count (CFU) and the count of aciduric bacteria (e.g., on Mitis-Salivarius Bacitracin agar).
- Enamel Demineralization: Assess the cariogenic activity of the biofilm by measuring the percentage of surface microhardness change (ΔVHN) and lesion depth in the underlying enamel disc using microhardness testing or transverse microradiography.
Protocol: Assessing Biofilm Pathogenicity in Clinical Samples
This protocol describes the use of bacterial biofluorescence for the objective assessment of tongue biofilm pathogenicity, resulting in the Tongue Biofilm Fluorescence Index (TBFI) [5].
Workflow Overview
Materials and Reagents
- QLF device (Qraycam) equipped with a 405-nm light source for excitation and appropriate filters to detect red fluorescence.
- Volatile Sulfur Compound (VSC) monitor (e.g., OralChroma) for quantifying hydrogen sulfide (H₂S) and methyl mercaptan (CH₃SH).
Procedure
- Image Acquisition: Position the patient such that their extended tongue is in clear view of the Qraycam. Capture two images under standardized conditions: a standard white-light image and a fluorescence image.
- TBFI Scoring: Analyze the fluorescence image to score the tongue biofilm based on two parameters, each on a scale of 0-2.
- Intensity (I): Rate the brightness of the red fluorescence.
- 0: No red fluorescence.
- 1: Faint red fluorescence, light pink in color.
- 2: Bright and vivid red fluorescence.
- Coverage (C): Rate the proportion of the dorsal tongue surface covered by red fluorescence.
- 0: No coverage.
- 1: Less than half of the surface covered.
- 2: More than half of the surface covered.
- Intensity (I): Rate the brightness of the red fluorescence.
- Calculate TBFI Score: Sum the Intensity and Coverage scores to obtain the final TBFI, which ranges from 0 to 4.
- Validation with VSCs: To confirm the pathogenicity of the biofilm, measure the levels of VSCs from the patient's oral cavity using a dedicated monitor. The strong positive correlation between TBFI and H₂S levels validates the index as a marker of biofilm pathogenicity.
The Scientist's Toolkit: Essential Reagents and Software
Table 3: Key Research Reagent Solutions and Tools
| Item | Function/Application | Specific Examples / Notes |
|---|---|---|
| QLF Imaging Device | Captures intrinsic fluorescence of biofilms for real-time, non-destructive assessment. | Qraycam Pro [23]; QLF-D [22]. Uses 405-nm light for excitation. |
| Fluorescence Stains | Labels specific biofilm components (e.g., glycoproteins, live/dead cells) for quantification. | Fluorescein-labelled Wheat Germ Agglutinin (WGA) stains matrix glycoproteins [24]. Resazurin assays viability [24]. |
| Specialized Growth Media | Supports the formation of complex, in vitro biofilms from clinical samples. | Brain Heart Infusion (BHI) supplemented with hemin, Vitamin K1, and L-Cysteine for anaerobic gut biofilm culture [24]. Media with 0.5% sucrose for cariogenic dental biofilms [22]. |
| Mucin-Coated Surfaces | Mimics host mucosal surfaces to grow physiologically relevant biofilms in vitro. | Polystyrene pegs coated with porcine gastric mucin (10 mg/ml) [24]. |
| Image Cytometry Software | Automated, high-throughput quantification of 3D biofilm architecture and internal fluorescence. | BiofilmQ: Quantifies hundreds of global and internal biofilm parameters from 3D image stacks [25]. Imaris: Used for single-cell tracking and lineage analysis within biofilms [26]. |
Data Analysis and Visualization
Advanced computational tools are indispensable for extracting meaningful quantitative data from biofilm fluorescence images.
- BiofilmQ Software: This open-source image cytometry tool is designed for the quantitative analysis of 3D microbial communities. It can process images from microcolonies to millimetric macrocolonies. After segmenting the biofilm biovolume, BiofilmQ dissects it into a cubical grid and calculates 49 different properties for each cube, including local fluorescence intensity, texture, and distance to the biofilm surface [25]. This allows for the spatially resolved correlation of fluorescence signals with structural features.
- Clinical Index Development: As demonstrated with the TBFI, reliability and validity are paramount. The TBFI showed superior inter-examiner reliability (κ = 0.752) compared to conventional indices, and its validity was confirmed by a significant positive correlation with VSCs, key markers of oral pathogenicity [5]. This statistical rigor is essential for developing a robust fluorescence-based metric.
From Theory to Practice: Standardized QLF Methodologies for Research and Clinical Trials
Standardized Imaging Protocols for In-Vivo and In-Vitro Study Designs
Quantitative Light-Induced Fluorescence (QLF) has emerged as a cornerstone technology for the non-invasive detection, quantification, and monitoring of dental biofilms. The principle is based on the illumination of dental surfaces with high-intensity blue light (typically at 405 nm) and the subsequent analysis of the autofluorescence emitted by teeth and bacterial metabolites. Sound tooth enamel exhibits strong green fluorescence, while demineralized areas appear darker due to reduced fluorescence. Concurrently, cariogenic bacteria within biofilms produce porphyrins, which emit a characteristic red fluorescence, the intensity of which correlates with biofilm metabolic activity and maturation. This dual-parameter capability allows QLF to provide quantitative data on both mineral loss and bacterial presence, making it indispensable for both clinical caries management and anti-biofilm therapeutic development [4] [20]. Standardized imaging protocols are critical for ensuring data reproducibility, enabling cross-study comparisons, and validating the efficacy of novel anti-biofilm compounds in both laboratory and clinical settings.
Technical Specifications and Performance Metrics
The diagnostic performance of QLF technology has been rigorously evaluated across various study designs. The following tables summarize key technical parameters and aggregated performance metrics from recent in-vivo and in-vitro studies.
Table 1: Key Technical Specifications of QLF Imaging
| Parameter | Specification | Research Application Notes |
|---|---|---|
| Light Wavelength | 405 nm (blue-violet spectrum) | Excites endogenous fluorophores in enamel and bacterial porphyrins [4] [20]. |
| Primary Output: ΔF | Percentage fluorescence loss (%) | Quantifies enamel demineralization; negative values indicate mineral loss [4]. |
| Primary Output: ΔR | Percentage red fluorescence gain (%) | Quantifies porphyrin content in cariogenic biofilms; positive values indicate bacterial activity [6] [18]. |
| Common Devices | QLF-Clin, Inspektor Pro, QLF-D, Qraypen C | Qraypen C (intraoral camera type) is frequently used in recent in-vivo studies [4] [20]. |
| Image Resolution | e.g., 1280 x 720 pixels (Qraypen C) | High resolution is critical for subsequent AI-based image analysis [20]. |
Table 2: Diagnostic Accuracy of QLF for Caries Detection (Meta-Analysis Data) [4]
| Study Type | Caries Location | Pooled Sensitivity | Pooled Specificity | Area Under Curve (AUC) Range |
|---|---|---|---|---|
| In-Vivo | Occlusal Surfaces | 0.86 | 0.82 | 0.94 - 0.98 |
| In-Vivo | Proximal Surfaces | 0.74 | 0.82 | 0.67 - 0.91 |
| In-Vitro | Occlusal Surfaces | 0.83 | 0.74 | 0.71 - 0.97 |
| In-Vitro | Proximal Surfaces | 0.83 | 0.74 | 0.80 - 0.91 |
Standardized In-Vivo Imaging Protocol
This protocol is designed for clinical studies involving human subjects to assess biofilm accumulation and activity in situ.
Pre-Imaging Subject Preparation
- Ethical Compliance: Obtain approval from an Institutional Review Board (IRB) or Ethics Committee. Secure written, informed consent from all participants [20].
- Inclusion/Exclusion Criteria: Define subject cohort clearly. Typical exclusion criteria include the presence of orthodontic appliances, full-coverage dental crowns in the study area, and medical conditions that compromise saliva production [7].
- Oral Hygiene Cessation: Implement a supervised plaque regrowth period. A common model is a 4-day non-brushing period where subjects abstain from all mechanical and chemical oral hygiene while maintaining their normal diet [7].
- Pre-Test Cleaning: On the baseline day (T0), conduct a professional dental prophylaxis using piezoelectric ultrasonic instruments and polishing paste to remove all plaque, stain, and calculus. Verify surface cleanliness with a plaque-disclosing agent [7].
Image Acquisition Workflow
- Equipment Setup: Use a calibrated QLF intraoral camera (e.g., Qraypen C). Ensure the device is connected to a computer with proprietary software for image capture and analysis.
- Subject Positioning: Seat the subject in an upright position. Use a cheek retractor to fully expose the teeth to be imaged. Gently dry the tooth surfaces with an air syringe for 5-10 seconds to remove saliva [18].
- Image Capture: Hold the camera tip perpendicular to the tooth surface at a standardized distance (as per manufacturer's guidelines, typically 5-10 mm). Ensure the entire tooth or series of teeth is in focus. Capture the QLF image. Subsequently, capture a white-light image with the same device for anatomical reference [20].
- Image Annotation: Annotate images with subject ID, date, time, and tooth number immediately after capture.
Standardized In-Vitro Imaging Protocol
This protocol is designed for laboratory-based studies, such as evaluating biofilm formation on dental materials or the efficacy of anti-biofilm agents under controlled conditions.
Specimen and Biofilm Preparation
- Substrate Selection: Prepare specimens (e.g., enamel slabs, restorative material discs like Composite, Ceramics, CoCrMo alloy). Standardize specimen size (e.g., 3 mm diameter, 2 mm thick). Polish and sterilize all specimens prior to use [27].
- Surface Characterization: Measure and record the surface roughness (Sa value) of all specimens using a high-resolution 3D optical profilometer, as roughness significantly influences biofilm adhesion [27].
- Biofilm Cultivation: Employ a dynamic biofilm reactor system (e.g., CDC Biofilm Reactor - CBR) for consistent and reproducible biofilm growth. Inoculate the system with the relevant bacterial strain (e.g., Streptococcus mutans, Pseudomonas azotoformans) and circulate the growth medium (e.g., Tryptic Soy Broth - TSB or sterilized milk) under controlled temperature and shear stress for a defined period (e.g., 24-48 hours) [28].
Image Acquisition and Analysis
- Sample Harvesting: Gently rinse the specimens with phosphate-buffered saline (PBS) to remove non-adherent planktonic cells.
- QLF Imaging: Mount the specimen in a standardized holder. Image under the same QLF camera settings as used in the in-vivo protocol. Ensure consistent camera distance and angle.
- Volumetric Analysis (Optional): For advanced quantification, use a 3D intraoral scanner (e.g., Trios 4) to obtain digital models of the specimens at baseline (T0) and post-biofilm formation (T4). Superimpose the models using dedicated software to calculate the volumetric plaque index (VPI in mm³), which represents the plaque volume accumulated over the reference surface [7].
- Reference Analysis: Following QLF imaging, validate biofilm mass via standard methods like Crystal Violet staining or quantify viable cells via Colony Forming Unit (CFU) enumeration [29] [28].
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagent Solutions for QLF Biofilm Studies
| Item | Function/Application | Examples & Notes |
|---|---|---|
| QLF Intraoral Camera | Primary device for image acquisition. | Qraypen C (AIOBIO), QLF-D (Inspektor). Ensure regular calibration [6] [20]. |
| Plaque Disclosing Agent | Visual validation of plaque presence and maturation. | Two-tone agents (e.g., Curaprox PlaqueFinder); stain young plaque pink and mature plaque blue [7] [18]. |
| Biofilm Reactor | In-vitro cultivation of standardized biofilms under dynamic conditions. | CDC Biofilm Reactor (CBR). Promotes consistent, reproducible biofilm growth [28]. |
| Intraoral Scanner | 3D model acquisition for volumetric plaque analysis. | Trios 4 (3Shape). Used to calculate Volumetric Plaque Index (VPI) [7]. |
| Reference Standards | Validation of QLF findings against established metrics. | International Caries Detection and Assessment System (ICDAS), Turesky Modification of Quigley-Hein Plaque Index (TMQHPlI) [7] [20]. |
| Cell Recovery Solutions | Detachment of in-vitro biofilms for downstream analysis. | Phosphate-Buffered Saline (PBS), Sonication bath (for synthetic sponge method) [28]. |
Data Interpretation and Correlation with Biofilm Maturation
A key strength of QLF is its ability to non-invasively monitor biofilm maturation. Research has established a strong positive correlation between the red fluorescence intensity (ΔR) and the maturation level of dental plaque. Studies using two-tone disclosing agents have confirmed that early, less mature plaque (stained pink) exhibits lower R/G (Red/Green) ratios in QLF images, while older, more mature, and pathogenic plaque (stained blue) shows significantly higher R/G ratios [18]. This quantitative relationship allows researchers to move beyond simple plaque presence/absence and track the dynamic development of biofilms over time or in response to treatment.
Furthermore, the integration of artificial intelligence (AI) with QLF image analysis is a cutting-edge development. Convolutional Neural Networks (CNNs), such as Xception, can be trained on large datasets of QLF images to automatically classify the presence of caries with high accuracy (e.g., 83-86%) [20]. These models enhance objectivity and throughput, making QLF an even more powerful tool for large-scale longitudinal studies and drug efficacy trials.
Within the expanding field of quantitative light-induced fluorescence (QLF) research, the objective quantification of dental biofilm represents a significant advancement over traditional subjective plaque indices. The core technological principle hinges on the phenomenon that dental plaque emits red fluorescence when exposed to high-energy blue light (typically at 405 nm wavelength), primarily due to the presence of bacterial porphyrins [18] [30]. This autofluorescence allows for reagentless detection and measurement of biofilm accumulation and maturation. Two primary quantitative parameters have emerged as standards in this domain: the Simple Plaque Score (SPS) and the Red Fluorescence Intensity (ΔR).
The SPS provides a qualitative and quantitative assessment of plaque deposition area, typically employing a 0-5 point scale based on the covered surface area [30]. Concurrently, the ΔR parameter delivers a quantitative measure of the fluorescence intensity, which correlates directly with the degree of plaque maturation and its bacterial load [18] [30]. The integration of these parameters within dental research, particularly in clinical trials for therapeutic interventions, smoking cessation studies, and oral care product development, enables a highly objective, reproducible, and sensitive analysis of oral biofilms [31]. This protocol details the experimental methodologies for the accurate interpretation of ΔR in relation to plaque coverage and SPS, framed within the context of a comprehensive thesis on advanced dental biofilm imaging.
Quantitative Data Synthesis
The following tables synthesize key quantitative relationships established in current QLF research, providing a reference for interpreting ΔR values and SPS scores.
Table 1: Interpretation of ΔR Values and SPS in Plaque Assessment
| Parameter | Value Range / Category | Clinical Interpretation | Research Significance |
|---|---|---|---|
| ΔR (Red Fluorescence Intensity) | ~2.75% | "No Calculus"/Healthy Surface | Baseline fluorescence, minimal bacterial activity [6] |
| ~6.06% | "Initial Calculus"/Early Plaque Accumulation | Indicator of initial biofilm maturation [6] | |
| ~15.58% | "Advanced Calculus"/Mature Plaque | High bacterial load and matured, pathogenic biofilm [6] | |
| ΔR30 / ΔR120 | ΔR30, ΔR120 | Plaque intensity thresholds (>30%, >120%) | Used to quantify mature, pathogenic plaque deposits; highly reproducible over 7- and 30-day intervals (p<0.0001) [31] |
| Simple Plaque Score (SPS) | 0 - 5 | Quantitative & qualitative assessment of plaque deposit area | Score assigned based on attached area of plaque; correlates with clinical indices (GI, BOP, PPD) [30] |
Table 2: Correlations Between QLF Parameters and Clinical Indices
| QLF Parameter | Clinical Index | Correlation Coefficient (r) | Statistical Significance (p) | Study Context |
|---|---|---|---|---|
| Mean Full-Mouth QLF-D Score | Gingival Index (GI) | 0.749 | < 0.01 | Validation against clinical indices [30] |
| Mean Full-Mouth QLF-D Score | Bleeding on Probing (BOP) | Not Specified | < 0.01 | Validation against clinical indices [30] |
| Mean Full-Mouth QLF-D Score | Probing Pocket Depth (PPD) | 0.683 | < 0.01 | Validation against clinical indices [30] |
| Mean Full-Mouth QLF-D Score | Patient Hygiene Performance (PHP) Index | Not Specified | < 0.01 | Validation against clinical indices [30] |
| Volumetric Plaque Index (VPI) | Turesky Modification of Quigley-Hein Plaque Index (TMQHPlI) | Positive Correlation | Not Specified | 3D plaque volumetrics study [7] |
Experimental Protocols for Data Acquisition
Protocol 1: Standardized QLF Image Acquisition and Analysis for ΔR and SPS
This protocol is designed for the consistent capture and analysis of QLF images to generate reliable ΔR and SPS data, suitable for longitudinal studies and interventional trials [30] [31].
I. Pre-Visit Participant Preparation
- Instruct participants to abstain from all oral hygiene (toothbrushing, mouthwashing, interdental flossing) for at least 2 hours prior to the assessment [31].
- Instruct participants to avoid eating, drinking (except water), and smoking for at least 2 hours prior to each study visit [31].
- For plaque regrowth studies, participants must cease all mechanical and chemical oral hygiene for a defined period (e.g., 4 days) following a professional dental prophylaxis [7].
II. Equipment and Software Setup
- QLF Device: Use a calibrated QLF device, such as the QRayCam Pro (Inspector Research Systems) or Q-ray cam (AIOBIO) [18] [31].
- Camera Settings: Configure for consistent imaging. Example parameters include:
- Analysis Software: Use dedicated QLF analysis software (e.g., QA2 v1.23, Inspector Research Systems) [30].
III. Image Acquisition Procedure
- Position the participant comfortably with a cheek retractor in place to expose all tooth surfaces.
- Capture a standardized series of full-mouth images, including the buccal and lingual surfaces of the maxillary and mandibular anterior teeth and posterior teeth [30].
- Ensure the camera is fixed at a consistent distance and angle to the tooth surface for all captures.
- Maintain stable ambient lighting conditions or operate in a controlled lighting environment throughout the study.
IV. Image Analysis for ΔR and SPS
- SPS Scoring: In the analysis software, assign a Simple Plaque Score (typically 0-5) to each tooth surface based on the area covered by fluorescent plaque [30].
- ΔR Analysis: Use the software to quantify the red fluorescence intensity. The software typically provides ΔR values, which may include sub-scores like ΔR30, ΔR70, and ΔR120, representing the area exceeding 30%, 70%, and 120% of a baseline red fluorescence intensity, respectively [30] [31]. These thresholds help differentiate plaque maturation levels.
Protocol 2: Validation of QLF Parameters Against Conventional Indices
This protocol is essential for establishing the clinical relevance of QLF-derived data by correlating it with established clinical metrics [30].
I. Clinical Examination Following QLF Imaging
- After QLF image acquisition, a trained clinician performs a clinical examination.
- Gingival Index (GI): Assesses the severity of gingivitis on a scale of 0 to 3 for each tooth.
- Bleeding on Probing (BOP): Records the presence or absence of bleeding within 30 seconds of gentle probing.
- Probing Pocket Depth (PPD): Measures the depth of the gingival sulcus/pocket in millimeters.
- Turesky Modification of Quigley-Hein Plaque Index (TMQHPlI): Scores plaque after disclosure on a scale of 0 to 5 [7].
II. Data Correlation and Statistical Analysis
- Calculate the mean full-mouth QLF-D score (SPS) and mean ΔR values for each participant.
- Perform correlation analysis (e.g., Pearson's correlation) between the mean QLF parameters and the clinical indices (GI, BOP, PPD, TMQHPlI) [30].
- A significant positive correlation (e.g., p < 0.01) validates the QLF parameter as a reliable indicator of clinical oral health status [30].
Workflow Visualization
The following diagram illustrates the logical workflow for the acquisition and interpretation of ΔR and SPS data, from participant preparation to final analysis and validation.
QLF Biofilm Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for QLF Dental Biofilm Studies
| Item / Solution | Function in Research | Application Notes |
|---|---|---|
| QLF Intraoral Camera (e.g., QRayCam Pro, Biluminator) | Captures fluorescence images of dental plaque induced by 405 nm blue light. | Enables quantitative analysis of red fluorescence without disclosing agents [30] [31]. |
| QLF Analysis Software (e.g., QA2 v1.23) | Quantifies SPS and ΔR parameters from acquired images. | Critical for objective, reproducible data extraction; allows for setting ΔR thresholds [30]. |
| Two-Tone Disclosing Solution (e.g., Curaprox PlaqueFinder) | Stains dental plaque: pink for young plaque, blue for mature plaque. | Used for validation against traditional indices like TMQHPlI [18] [7]. |
| Professional Prophylaxis Kit (Ultrasonic scaler, polishing paste) | Provides a standardized, plaque-free baseline (T0). | Essential for plaque regrowth study models [7]. |
| Exhaled Carbon Monoxide (eCO) Monitor | Objectively verifies smoking status of study participants. | Crucial for studies investigating plaque in smokers vs. non-smokers [31]. |
Quantitative Light-Induced Fluorescence (QLF) technology has established itself as a pivotal tool in cariology research, particularly for the longitudinal assessment of demineralization and remineralization processes. Based on the autofluorescence of dental hard tissues when irradiated with high-energy visible light (typically at a 405 nm wavelength), QLF enables the quantitative detection of minute mineral changes that are invisible to the naked eye [13] [32]. The fundamental principle underpinning QLF is that carious lesions exhibit a reduction in natural fluorescence compared to sound enamel; this fluorescence loss is quantified as Delta F (ΔF), a parameter highly correlated with mineral loss [4] [33]. A second key principle is the detection of red fluorescence, quantified as Delta R (ΔR), which is emitted by bacterial metabolites such as porphyrins present in carious lesions and oral biofilms [4]. This dual-parameter capability allows researchers not only to quantify mineral status but also to infer microbiological activity, making QLF uniquely suited for monitoring lesion activity and evaluating the efficacy of preventive agents, antimicrobials, and remineralization therapies in both clinical and laboratory settings.
The clinical significance of this technology is profound. Traditional diagnostic methods, like visual inspection and radiography, have marked limitations, especially for early lesions. Visual inspection shows highly variable sensitivity (0.2–0.96), while radiography has low sensitivity (0.14–0.38) for detecting early demineralization [13]. QLF addresses these gaps by providing a non-invasive, quantitative, and reproducible means to detect caries at the earliest stages and monitor their progression or regression over time [4] [33]. This is crucial for implementing a "paradigm shift" in dentistry from surgical intervention to non-surgical management of early lesions, facilitating evidence-based decision-making and personalized caries management [13]. The technology's high reproducibility is evidenced by an intraclass correlation coefficient (ICC) of 0.96 and excellent intra- and inter-examiner agreement (0.93 and 0.92, respectively) [13].
Performance Data and Quantitative Values
The diagnostic performance of QLF has been rigorously evaluated across various caries types and locations. The following tables summarize key quantitative data extracted from recent systematic reviews and primary studies, providing a clear overview of its capabilities and limitations for researchers.
Table 1: Diagnostic Accuracy of QLF for Occlusal and Proximal Caries (In Vivo)
| Caries Type | Lesion Threshold | Sensitivity (Range) | Specificity (Range) | AUROC (Range) | Pooled Sensitivity | Pooled Specificity |
|---|---|---|---|---|---|---|
| Occlusal | Incipient (ICDAS 1-2) | 0.76 – 0.91 | 0.74 – 0.93 | 0.81 – 0.93 | 0.86 | 0.82 |
| Occlusal | Advanced Enamel & Dentin (ICDAS 3+) | 0.90 – 0.98 | 0.83 – 0.96 | 0.94 – 0.98 | - | - |
| Proximal | Enamel vs. Dentin | 0.63 – 0.91 | 0.62 – 0.74 | 0.67 – 0.91 | 0.74 | 0.82 |
Table 2: Accuracy of Different QLF Devices for Various Caries Types
| Device | Caries Type | Accuracy (Range) | AUROC (Range) | Key Application |
|---|---|---|---|---|
| Qraycam Pro (QP) | Occlusal Caries | 0.81 – 0.82 | 0.87 – 0.94 | Precise evaluation of individual teeth |
| Qraypen C (QC) | Occlusal Caries | 0.83 – 0.96 | 0.92 – 0.99 | Screening of demineralized teeth |
| Qraycam Pro (QP) | Proximal Caries | 0.52 – 0.71 | 0.56 – 0.64 | Precise evaluation with radiographic correlation |
| Qraypen C (QC) | Proximal Caries | 0.52 – 0.62 | 0.60 – 0.67 | Screening |
Table 3: Key QLF Parameters and Their Interpretation for Longitudinal Studies
| Parameter | Description | Biological Correlation | Utility in Monitoring |
|---|---|---|---|
| ΔF (%) | Average percentage loss of fluorescence within a lesion | Correlates with the degree of mineral loss | Primary metric for quantifying demineralization and remineralization |
| ΔFmax (%) | Maximum fluorescence loss within a lesion | Indicates the area of most severe demineralization | Identifies lesion hotspots and maximum severity |
| ΔR (Gain) | Gain in red fluorescence intensity | Correlates with the presence of porphyrins from microbial metabolism | Monitoring caries activity and antibacterial efficacy |
| ΔRmax (Gain) | Maximum red fluorescence gain within a lesion | Indicates areas of highest microbial metabolic activity | Useful for assessing secondary caries and lesion activity |
| Lesion Area (mm²) | The surface area of the lesion with fluorescence loss above a threshold (e.g., >5%) | Represents the lateral spread of the demineralized area | Tracking lesion expansion or contraction over time |
Beyond caries, QLF parameters show predictive value for other dental pathologies. A 2025 study on pulp diagnosis in cracked teeth found that ΔF and ΔFmax decreased with the progression of pulp disease, while ΔR and ΔRmax increased. The technology could predict pulp diagnosis with an accuracy of up to 82.1% for reversible pulpitis and 80.0% for pulp necrosis, demonstrating the expanding utility of these quantitative values [34].
Experimental Protocols for Longitudinal Monitoring
Protocol A: Baseline In-Vivo Screening and Monitoring
This protocol is designed for clinical studies aiming to screen subjects and monitor lesion changes over time in a natural oral environment.
Detailed Procedures:
- Subject Preparation and Image Acquisition: Prior to imaging, subjects should undergo professional prophylaxis to remove plaque and stains. The tooth surface of interest must be isolated and air-dried for approximately 5 seconds. QLF images are captured using a clinical device (e.g., Qraycam Pro, Qraypen C, or QLF-D) in a completely dark environment or using a specialized dark hood to block ambient light. The blue light source should have a peak wavelength of 405 nm, and the emitted fluorescence is collected through a high-pass yellow filter (e.g., γ > 520 nm) [13] [32].
- Baseline Analysis: The captured images are imported into proprietary analysis software (e.g., Inspektor QLF, QA2). The operator defines the sound enamel reference area adjacent to the lesion. The software then automatically calculates and records key parameters:
- Intervention and Follow-up: Subjects begin the intervention regimen (e.g., use of a test toothpaste, application of a varnish). The QLF image acquisition process (steps 1-2) is repeated at predetermined intervals (e.g., 1, 3, 6, 12, and 18 months) under identical conditions [32].
- Outcome Calculation: The changes from baseline are calculated for the primary outcomes:
- ΔΔF = ΔFbaseline - ΔFfollow-up
- ΔLesion Area = Areabaseline - Areafollow-up A positive ΔΔF value indicates regression of the lesion (remineralization), while a negative value indicates progression (demineralization) [32].
Protocol B: In-Vitro Demineralization/Remineralization Cycling
This protocol is suited for controlled laboratory studies evaluating the efficacy of bioactive compounds, making it highly relevant for drug development.
Detailed Procedures:
- Specimen Preparation and Baseline: Enamel slabs are prepared from extracted human bovine teeth. A reference surface is protected with an acid-resistant varnish, leaving a defined window exposed. Baseline QLF images are captured for all specimens after a light polishing and air-drying cycle [32].
- Demineralization Phase: Specimens are subjected to a demineralizing solution (e.g., pH 4.8-5.0) for a set period (e.g., 3-5 days) to create artificial caries-like lesions. QLF imaging is repeated to confirm and quantify lesion formation (Post-Demin ΔF).
- Treatment and Cycling: Specimens are randomly assigned to treatment groups (e.g., negative control, positive control fluoride, experimental bioactive molecule). A pH-cycling model is employed to simulate oral conditions, typically involving daily immersion in a demineralizing solution (e.g., 6 hours) and a remineralizing solution (e.g., 18 hours). Test agents are applied as per the study design during the cycling period.
- Outcome Analysis: After the cycling period (e.g., 5-14 days), final QLF images are acquired. The primary outcome is the percentage of fluorescence recovery, calculated as: % Recovery = [(ΔFinitial - ΔFfinal) / (ΔFinitial - ΔFsound)] × 100. Statistical analysis (e.g., ANOVA with post-hoc tests) is used to compare recovery between treatment groups.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Materials and Reagents for QLF-Based Studies
| Item / Reagent Solution | Function / Rationale | Example Specifications / Notes |
|---|---|---|
| QLF Device | Captures fluorescence images for quantitative analysis. | QLF-D (DSLR type), Qraycam Pro (large FOV), Qraypen C (pen-type, small FOV). CMOS sensor, 405 nm LED/laser, >520 nm filter [13] [4]. |
| Analysis Software | Quantifies fluorescence parameters (ΔF, ΔR, Area). | Proprietary software (e.g., Inspektor QLF, QA2). Essential for standardized, objective measurement [13] [32]. |
| Demineralization Solution | Creates standardized artificial caries lesions in vitro. | Acetate buffer (pH 4.5-5.0) with Ca²⁺, PO₄³⁻, e.g., 2.2 mM CaCl₂, 2.2 mM KH₂PO₄. Mimics the undersaturated cariogenic challenge [32]. |
| Remineralization Solution | Simulates saliva's remineralizing potential in pH-cycling models. | Tris buffer (pH 7.0) with higher Ca²⁺, PO₄³⁻, e.g., 1.5 mM CaCl₂, 0.9 mM KH₂PO₄. Supersaturated with respect to tooth mineral [32]. |
| Test Remineralizing Agents | The investigational product for efficacy testing. | Fluoride formulations (NaF, SnF₂), Bioactive glass (Novamin), CPP-ACP (Recaldent), experimental peptides/polymers. |
| Artificial Saliva | Maintains hydration and provides a mineral reservoir during in-vitro experiments. | Contains Ca²⁺, PO₄³⁻, buffers, and mucin. Used as a storage solution and in some cycling models. |
| Acid-Resistant Varnish | Creates a protected "sound enamel" reference area on specimens for in-vitro studies. | Acid-resistant nail varnish or specialized dental varnish. Critical for accurate ΔF calculation [32]. |
Quantitative Light-Induced Fluorescence (QLF) technology has emerged as a pivotal tool in oral health research, enabling the non-invasive quantification and monitoring of dental biofilms. By utilizing 405 nm blue light to induce autofluorescence in tooth structures, QLF detects and quantifies fluorescence loss (ΔF), correlating with enamel demineralization, and red fluorescence (ΔR), emanating from bacterial metabolites such as porphyrins [9] [13]. This dual-parameter approach allows for real-time assessment of caries severity and biofilm activity, making it particularly valuable for monitoring high-risk populations [9]. Orthodontic patients and high-caries-risk cohorts represent specialized populations where ecological changes in the oral environment significantly increase susceptibility to caries and periodontal inflammation [35] [36]. The presence of fixed orthodontic appliances creates numerous plaque-retentive areas, alters saliva flow, and impedes effective mechanical plaque removal, leading to ecological shifts in the oral microbiota [35] [37]. Similarly, high-caries-risk individuals exhibit biofilms with distinct phenotypic properties, including enhanced acid tolerance and altered metabolic profiles [38]. This application note delineates detailed protocols and synthesizes key quantitative data for employing QLF in biofilm research within these specialized populations, providing a framework for researchers and clinicians to advance caries management strategies.
QLF Technology and Biofilm Assessment Parameters
QLF technology operates on the principle of autofluorescence. When sound tooth enamel is illuminated with high-intensity blue light (405 nm), it emits strong green fluorescence. Demineralized areas, with reduced mineral density, scatter more light and exhibit diminished fluorescence, quantified as ΔF (percentage fluorescence loss) [9] [13]. Concurrently, QLF captures red fluorescence (ΔR) from porphyrin metabolites produced by cariogenic bacteria within the biofilm, serving as a biomarker for mature and pathogenic plaque [9] [39]. The primary QLF parameters used for biofilm and caries assessment are detailed in Table 1.
Table 1: Key QLF Parameters for Biofilm and Caries Assessment
| Parameter | Description | Biological Significance | Application Context |
|---|---|---|---|
| ΔF (Delta F) | Percentage loss of green fluorescence compared to sound enamel. | Correlates with the degree of enamel demineralization and mineral loss [9] [13]. | Detection and monitoring of early caries (white spot lesions) [9]. |
| ΔR (Delta R) | Gain in red fluorescence intensity. | Indicates the presence of porphyrins, metabolites from mature, cariogenic biofilms, and calculus [9] [39]. | Assessing biofilm pathogenicity and maturity; caries activity screening [13] [39]. |
| ΔQ (Delta Q) | The product of ΔF and the lesion area. | Represents the total mineral loss volume of a lesion [9]. | Quantifying the overall burden of demineralization. |
| SOH Score | Simple Oral Hygiene score derived from ΔR analysis. | Proprietary software-generated score summarizing plaque and calculus accumulation [39]. | Rapid assessment of oral hygiene status in clinical and research settings. |
The diagnostic accuracy of QLF has been validated across multiple studies. A recent meta-analysis reported excellent in vivo performance for detecting occlusal caries, with Area Under the Curve (AUC) values ranging from 0.94 to 0.98 for incipient lesions [9]. Pooled sensitivity and specificity were high for occlusal caries (in vivo: 0.86/0.82) and good for approximal caries (in vivo: 0.74/0.82), confirming its effectiveness for early-stage detection [9].
Biofilm Dynamics in Specialized Populations
Orthodontic Patients
Fixed orthodontic appliances significantly alter the oral ecosystem, fostering biofilm accumulation and dysbiosis. Research comparing labial and lingual brackets has revealed significantly higher (p < .001) total biofilm formation on lingual brackets (41.56%) compared to labial brackets (26.52%) [35]. The distribution is also uneven, with the highest biofilm accumulation found on the gingival, mesial, and distal surfaces of brackets in both types [35].
The shift towards a cariogenic microbiome in orthodontic patients is substantiated by 16S rRNA sequencing studies. In adolescents with fixed appliances, supragingival plaque from caries-active individuals shows enriched levels of Streptococcus mutans, Neisseria, Haemophilus, Granulicatella, and Abiotrophia species compared to their caries-free counterparts [37]. Conversely, the caries-free state is associated with genera such as Selenomonas_3, Oribacterium, Dialister, and Olsenella [37].
The type of orthodontic appliance also influences the microbiome. Clear aligners, being removable, produce less dysbiosis compared to multibracket fixed appliances [40] [41]. While multibracket appliances promote an increase in anaerobic and cariogenic bacteria, aligners are associated with a different microbial shift, including elevated levels of Burkholderiaceae, a family not commonly dominant in the oral cavity [41]. However, aligners still require stringent hygiene, as they cover tooth surfaces, reducing the natural cleansing action of saliva and soft tissues [41].
High-Caries-Risk Cohorts
In high-caries-risk cohorts, the oral biofilm exhibits distinct phenotypic and metabolic characteristics beyond mere compositional shifts. Studies comparing plaque from children with severe caries (CA) to those who are caries-free (CF) have demonstrated that the CA group has a significantly higher (p < 0.05) mean acid tolerance (AT) score (4.1 vs. 2.6) [38]. This enhanced resilience to low pH is a key virulence factor.
Metabolically, plaque from CA individuals exhibits a more homolactic fermentation profile after a glucose pulse, showing significantly higher lactate-to-acetate, lactate-to-formate, and lactate-to-succinate ratios than CF plaques [38]. This metabolic shift contributes to a more acidic and cariogenic environment. Microbial characterization of these plaques reveals 25 species significantly more abundant in the CA samples, including species of Streptococcus, Prevotella, Leptotrichia, and Veillonella [38].
Table 2: Comparative Biofilm Analysis in Orthodontic and High-Caries-Risk Populations
| Characteristic | Orthodontic Patients (Fixed Appliances) | High-Caries-Risk Cohorts |
|---|---|---|
| Key Quantitative Findings | • Lingual brackets: 41.56% biofilm coverage [35]• Labial brackets: 26.52% biofilm coverage [35] | • Mean Acid Tolerance score: 4.1 (CA) vs 2.6 (CF) [38] |
| Relevant QLF Parameters | ΔF for monitoring demineralization around brackets; ΔR for assessing maturity of adherent plaque [9] [13]. | ΔR for identifying pathogenic, porphyrin-rich plaque; ΔF for early lesion detection [38] [9]. |
| Microbial Biomarkers | ↑ Streptococcus mutans, Neisseria, Haemophilus (Caries-Active) [37]. | ↑ Streptococcus spp., Prevotella, Leptotrichia, Veillonella [38]. |
| ↑ Selenomonas_3, Oribacterium, Dialister (Caries-Free) [37]. | Altered metabolic profile with higher lactate ratios [38]. | |
| Primary Risk Factor | Biofilm retention on non-shedding surfaces, hindering oral hygiene [35] [36]. | Phenotypic shift to acid-tolerant and acidogenic biofilm community [38]. |
Experimental Protocols for QLF Biofilm Imaging
QLF Imaging Protocol for Orthodontic Patients
Objective: To quantitatively monitor biofilm development and enamel demineralization around fixed orthodontic appliances or clear aligners.
Materials:
- QLF device (e.g., Qraycam Pro for full-arch screening or Qraypen C for detailed bracket-level imaging) [13].
- QA2 or equivalent analysis software.
- Calibration standard according to manufacturer specifications.
- Sterile cheek retractors, compressed air, and cotton rolls.
Procedure:
- Patient Preparation: Instruct patients to abstain from oral hygiene procedures, eating, or drinking for at least 2 hours prior to imaging. Remove aligners if present.
- Device Calibration: Perform daily calibration as per the manufacturer's instructions to ensure consistent fluorescence measurements.
- Image Acquisition:
- For fixed appliances: Use the Qraypen C (QC) to capture images of individual teeth/brackets from multiple aspects (occlusal, gingival, mesial, distal) at a close distance [13]. Ensure the bracket, adhesive, and surrounding enamel are in focus.
- For aligner therapy/overview: Use the Qraycam Pro (QP) to obtain full-arch images for a general screening of plaque distribution and demineralization [13].
- Dry the tooth surfaces gently with compressed air for 3-5 seconds before capturing each image to avoid saliva artifacts.
- Image Analysis:
- In the analysis software, select the Region of Interest (ROI). For fixed appliances, this may include the bracket base, the adhesive-enamel interface, and the adjacent enamel [35].
- For demineralization analysis, the software will calculate ΔF and ΔQ for the hypo-fluorescent areas.
- For biofilm analysis, set the software to detect and quantify the red fluorescence, obtaining ΔR values and the SOH Score [39].
- Data Interpretation: Track changes in ΔF and ΔR over time. An increase in ΔR around brackets indicates maturation of cariogenic biofilm, while a rising ΔF signifies active demineralization.
Protocol for Correlating QLF with Biofilm Phenotype in High-Risk Cohorts
Objective: To correlate QLF parameters (ΔR) with the acid tolerance and metabolic profile of supragingival plaque in high-caries-risk individuals.
Materials:
- QLF device (as above).
- Sterile plastic carvers or curettes for plaque collection.
- Microcentrifuge tubes with sterile UHQ-water or transport medium.
- Facilities for confocal microscopy, LIVE/DEAD BacLight stain, and Nuclear Magnetic Resonance (NMR) for metabolic profiling [38].
Procedure:
- Subject Selection & Imaging: Recruit subjects based on defined caries risk criteria (e.g., caries-active vs. caries-free). Perform QLF imaging as in Section 4.1 to obtain baseline ΔR values from smooth surfaces [38].
- Plaque Sampling: Immediately after imaging, collect supragingival plaque from all accessible buccal and lingual surfaces using a sterile plastic carver. Pool the sample in a microcentrifuge containing 500 µl sterile UHQ-water [38].
- Acid Tolerance Assessment:
- Vortex the plaque sample and divide it.
- Centrifuge a portion, discard the supernatant, and resuspend the pellet in a buffer adjusted to pH 3.5 for a defined period (e.g., 30-60 minutes).
- Use LIVE/DEAD staining and confocal microscopy to assess bacterial viability post-acid challenge. Assign an AT score (1=no/low tolerance, 5=high tolerance) based on the percentage of surviving cells [38].
- Metabolic Profiling:
- Subject another portion of the plaque sample to a glucose pulse (e.g., 20 mM for 1 hour).
- Use NMR to analyze the end-products of glucose metabolism, calculating ratios like lactate-to-acetate and lactate-to-formate [38].
- Data Correlation: Statistically correlate the baseline QLF ΔR values from step 1 with the experimentally determined AT scores and metabolic ratios from steps 3 and 4.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for QLF Biofilm Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| Qraycam Pro (QP) | Large Field-of-View (FOV) QLF device for full-arch screening and overall plaque assessment [13]. | Initial screening of plaque distribution in orthodontic patients [13] [39]. |
| Qraypen C (QC) | Small FOV, intraoral QLF device for detailed imaging of specific sites, such as individual brackets or lesions [13]. | Quantifying biofilm formation on the gingival surface of a lingual bracket [35] [13]. |
| QA2 Software | Proprietary analysis software for calculating QLF parameters (ΔF, ΔR, ΔQ, SOH Score) from acquired images [13]. | Tracking the progression of demineralization (ΔF) around a bracket over 3 months [9]. |
| LIVE/DEAD BacLight Viability Stain | Fluorescent stain used to distinguish live vs. dead bacteria via confocal microscopy after an acid challenge [38]. | Determining the acid tolerance (AT) of plaque microbiota from high-caries-risk children [38]. |
| Nuclear Magnetic Resonance (NMR) Spectroscopy | Analytical technique for identifying and quantifying metabolites in a complex mixture [38]. | Profiling the end-products (lactate, acetate, formate, etc.) of glucose metabolism in plaque samples [38]. |
| Chlorhexidine Mouthwash | Gold-standard antimicrobial and anti-biofilm agent used as a positive control in intervention studies [41] [42]. | Evaluating the efficacy of a novel biofilm-targeted therapy in reducing plaque ΔR values [42]. |
Data Analysis and Integration
Effective analysis of QLF data in population studies requires a systematic approach. Researchers should employ Bland-Altman plots to assess the agreement between different QLF devices (e.g., QP vs. QC) when used in the same study, particularly focusing on parameters like ΔFaver. which has shown good inter-device agreement [13]. For diagnostic accuracy studies, calculate sensitivity, specificity, and Area Under the Receiver Operating Characteristic curve (AUROC) against a reference standard like ICDAS or histology [9] [13].
Integrating QLF data with microbiome and phenotypic profiles is crucial for a holistic understanding. The relationship between QLF measurements and biofilm characteristics can be conceptualized as a feedback loop that drives caries progression, as illustrated in the following diagram.
Longitudinal statistical models, such as repeated-measures ANOVA or linear mixed-effects models, are essential for analyzing temporal changes in QLF parameters (ΔF, ΔR) in response to interventions or natural disease progression in these cohorts. Furthermore, multivariate analyses, including Principal Coordinates Analysis (PCoA) based on Bray-Curtis dissimilarity, can integrate QLF data with 16S rRNA sequencing data to visualize how microbial community structures cluster according to QLF-measured plaque levels or caries activity status [37].
Navigating Technical Challenges: Optimization and Limitations of QLF Biofilm Imaging
Within dental biofilm imaging research, the accurate quantification of plaque is fundamental for both clinical assessments and the evaluation of oral care products. Quantitative Light-induced Fluorescence (QLF) and planimetric analysis of disclosed plaque represent two prominent methodological approaches. However, a direct comparison reveals significant method discrepancies that researchers must address to ensure valid and reproducible results. This document details these discrepancies, provides standardized protocols for both methods, and offers guidance for their application within a research context, framing this within the broader thesis of advancing standardized methodologies in dental biofilm imaging.
Core Principles and Methodological Discrepancies
The fundamental discrepancy between QLF and conventional planimetric analysis stems from their underlying detection principles.
QLF Technology operates on the principle of biofluorescence. When illuminated with high-energy violet-blue light (typically at 405 nm), dental biofilms emit natural fluorescence. The key diagnostic signal for plaque is the red fluorescence (quantified as ΔR), which is caused by bacterial metabolites, such as porphyrins, within the biofilm [4] [43]. The intensity of this red fluorescence has been shown to correlate with the age and thickness of the biofilm [43]. QLF does not require the application of an external disclosing agent and allows for digital quantification of the fluorescent plaque area as a percentage of the total tooth surface [3] [23].
Planimetric Analysis, in contrast, is a colorimetric method that relies on the use of plaque-disclosing agents (PDAs). These agents, typically containing dyes, stain the plaque, making it visually distinct from the clean tooth surface [7] [43]. Conventional digital photographs are then taken, and the plaque-covered area is planimetrically quantified, again as a percentage of the total tooth surface area. This method is often considered a "gold standard" in clinical studies due to its direct visualization of plaque mass [43].
A critical 2020 in vivo study directly compared these two methods in patients with multibracket appliances. The study found a substantial method discrepancy: QLF-D images reported a mean plaque-covered area of 20.7% ± 17.4, while conventional photographs of disclosed plaque showed a significantly higher mean plaque coverage of 36.2% ± 23.5 [43]. The Bland-Altman analysis revealed inconsistent scattering with deviations of up to -15.5% on average, indicating that QLF-D systematically underestimates plaque coverage compared to the planimetric method, with the discrepancy increasing as the overall plaque load increases [43]. This suggests that QLF may not detect all plaque present, particularly thin or early-stage biofilms that produce less pronounced red fluorescence.
Detailed Experimental Protocols
Protocol for QLF-Based Plaque Quantification
This protocol is adapted from studies evaluating biofilm fluorescence for gingival health screening [3] [23].
Objective: To acquire and quantitatively analyze red fluorescent dental biofilm from anterior teeth using a QLF device.
Materials:
- QLF imaging device (e.g., Qraycam Pro, QLF-D Billuminator)
- Lip retractor
- Headrest or camera stand for stabilization
- Computer with proprietary QLF analysis software
Procedure:
- Patient Preparation: Instruct the patient to refrain from oral hygiene measures for 24 hours prior to imaging to allow for sufficient plaque accumulation [43]. Seat the patient comfortably.
- Image Acquisition: Place a lip retractor to fully expose the anterior teeth (upper and lower incisors and canines). Position the patient's head in a headrest and align the QLF camera tubus approximately 5 cm from and perpendicular to the tooth surfaces. Ensure imaging is performed in a dark environment to avoid ambient light interference. Capture standardized images of the labial surfaces of the six anterior teeth in both the upper and lower jaw [3].
- Image Analysis:
- Import the QLF images into the analysis software.
- Manually define the Region of Interest (ROI) by outlining the surface of each individual anterior tooth.
- The software will automatically apply a proprietary algorithm to detect pixels exhibiting red biofluorescence based on predefined fluorescence thresholds.
- Record the output metrics: the total area of the red fluorescent biofilm (in mm² or as a percentage of the total ROI surface area) [23].
Protocol for Planimetric Analysis of Disclosed Plaque
This protocol is adapted from a cross-sectional clinical study comparing QLF-D with disclosed plaque [43].
Objective: To quantify plaque coverage using a disclosing agent and conventional digital photography.
Materials:
- Two-tone plaque-disclosing agent (e.g., containing CI 42090 and 45410) [7]
- Cotton pellets or applicators
- Digital camera (or QLF-D device with white LED mode) with macro lens and ring flash
- Lip retractor
- Calibrated mirror for lingual surfaces
- Computer with image analysis software (e.g., ImageJ/Fiji, Adobe Photoshop)
Procedure:
- Patient Preparation: Identical to the QLF protocol—ensure 24 hours of plaque accumulation.
- Plaque Disclosure: Apply the two-tone disclosing solution thoroughly to all tooth surfaces using a saturated cotton pellet. Instruct the patient to rinse with water for 10 seconds to remove excess dye [43].
- Image Acquisition: Use a lip retractor for full visibility. Take high-resolution, standardized conventional digital photographs of the labial and lingual surfaces of the teeth. Use a mirror for lingual shots. Maintain consistent camera settings (aperture, shutter speed, ISO) and lighting conditions (e.g., using a ring flash) across all sessions [43].
- Image Analysis:
- Convert the digital photographs to grayscale.
- Manually define the ROI by masking the entire tooth surface, excluding brackets, wires, or gingival margins.
- Set a consistent brightness threshold (e.g., a value of 90 on an 8-bit grayscale where 0 is black and 255 is white) to differentiate the stained plaque areas (darker) from the clean tooth surface (lighter).
- Use the software's measurement function to calculate the plaque-covered area within the ROI.
- Express the result as a percentage of the total ROI area covered by the disclosed plaque [43].
Quantitative Data Synthesis
The table below synthesizes key performance data for QLF and planimetric analysis, highlighting their diagnostic characteristics and comparative performance.
Table 1: Comparative Diagnostic Performance of QLF and Planimetric Analysis
| Metric | QLF (In Vivo Occlusal Caries Detection) [4] | Planimetric Analysis (Disclosed Plaque) | Comparative Findings (QLF vs. Planimetric) |
|---|---|---|---|
| Primary Output | Fluorescence loss (ΔF), Red fluorescence gain (ΔR) | Percentage of surface area covered by disclosed plaque | Systematic underestimation by QLF; mean difference of -15.5% [43] |
| Pooled Sensitivity | 0.86 (Occlusal) | Not directly applicable (considered reference) | QLF detects a different, likely more mature, subset of plaque |
| Pooled Specificity | 0.82 (Occlusal) | Not directly applicable (considered reference) | QLF specificity is high against sound surfaces |
| Area Under Curve (AUC) | 0.94 - 0.98 (In vivo, sound vs. dentinal lesions) | Not applicable | Confirms excellent diagnostic accuracy for caries, but not directly translatable to simple plaque coverage |
| Correlation with Health | Significant correlation with GI (r=0.422), BOP (r=0.376) [23] | Direct visual correlation with plaque mass | QLF red fluorescence is an effective indicator for gingival health screening [23] |
Experimental Workflow and Logical Relationships
The following diagram illustrates the logical workflow for a comparative study design that incorporates both QLF and planimetric methods, helping to identify the source of method discrepancies.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for QLF and Planimetric Plaque Research
| Item | Function/Description | Example Products / Notes |
|---|---|---|
| QLF Imaging Device | Emits 405 nm light to excite natural biofilm fluorescence; captures resulting fluorescence images. | QLF-D Billuminator, Qraycam Pro [3] [23] |
| Plaque-Disclosing Agent (PDA) | Stains dental plaque for visual enhancement and planimetric quantification. | Two-tone solutions (e.g., Mira-2-Ton, Curaprox PlaqueFinder) distinguish old vs. new plaque [7] [43] |
| Intraoral Scanner (IOS) | Captures 3D digital models of the dentition for volumetric plaque analysis (emerging method). | Trios 4 (3Shape) [7] |
| Image Analysis Software | Quantifies plaque area (from photos) or fluorescence parameters (from QLF images). | ImageJ/Fiji (open-source), proprietary QLF analysis software [43] |
| Lip Retractor | Standardizes image acquisition by providing full visibility of anterior and posterior teeth. | Common dental photography accessory [43] |
| Calibration Standards | Ensures consistency and accuracy in color reproduction and light intensity across imaging sessions. | Color checker charts, fluorescence standards |
The discrepancy between QLF and planimetric analysis is not a matter of one method being inherently "correct" but rather a reflection of their different detection targets. QLF detects metabolically active, porphyrin-producing biofilm, while planimetric analysis detects total disclosed plaque mass.
Selection guidance for researchers and drug development professionals:
- Use QLF for studies focusing on biofilm activity, monitoring anti-microbial effects on bacterial metabolism, longitudinal studies where repeated disclosing is impractical, or for patient motivation with immediate visual feedback.
- Use Planimetric Analysis for studies requiring the quantification of total plaque accumulation (mass), for validating the efficacy of mechanical plaque removal agents, or when a widely accepted "gold standard" is required for regulatory purposes.
For the highest rigor in study design, especially during method validation, employing both techniques in parallel is recommended. This approach allows for a comprehensive understanding of a product's or therapy's impact on both the physical presence and the pathological activity of dental biofilms.
Within the framework of a broader thesis on advancing quantitative light-induced fluorescence (QLF) for dental biofilm research, addressing methodological standardization is paramount. The accurate quantification of biofilm pathogenicity via red fluorescence (RF) is critically dependent on technical precision. This application note details the primary technical pitfalls—specifically hydration status, the use of disclosing agents, and image capture conditions—that impact the validity and reproducibility of QLF data. We provide validated protocols and quantitative frameworks to mitigate these variables, ensuring that research outcomes accurately reflect biofilm physiology rather than imaging artifacts.
Core Technical Principles and Pitfalls
Quantitative Light-induced Fluorescence operates on the principle that when illuminated with high-energy blue light (typically 405 nm), dental biofilms emit natural fluorescence. The key analytes are porphyrins, metabolites produced by pathogenic bacteria within mature biofilms, which emit a characteristic red fluorescence (RF) [44]. The intensity of this RF, often quantified as the Red/Green ratio (R/G value), is correlated with biofilm pathogenicity, maturity, and cariogenic potential [44] [23].
The primary technical challenges arise because the RF signal is susceptible to multiple physical and optical interferences, which can lead to either the underestimation or overestimation of true biofilm pathogenicity.
Pitfall 1: Hydration Status
The hydration level of a biofilm significantly influences its optical properties. Desiccation, even for short periods, can alter light scattering and absorption characteristics.
- Impact: An air-dried biofilm may appear brighter and exhibit higher fluorescence intensity due to the loss of water, which has a refractive index similar to enamel. This creates a greater refractive index mismatch at the biofilm-tooth interface, enhancing contrast but potentially leading to an overestimation of biofilm volume and RF intensity that is not physiologically relevant.
- Evidence: Studies utilizing intraoral scans (IOS) for 3D volumetric plaque assessment emphasize the necessity of consistent hydration, as minute changes in surface topography are used to calculate plaque volume [7]. Inconsistent hydration would directly distort these volumetric measurements.
Pitfall 2: Use of Plaque-Disclosing Agents
The application of plaque-disclosing agents (PDAs) is a common practice in plaque index scoring, but it is incompatible with standardized QLF imaging.
- Impact: PDAs contain dyes (e.g., CI 42090 and CI 45410) that absorb and emit light in specific spectra, which can directly interfere with or completely mask the endogenous red fluorescence from bacterial porphyrins [45] [7].
- Evidence: Research comparing QLF-D to conventional photographs of disclosed plaque found a "very large inconsistent scattering" and a systematic method error, with QLF-D on average underestimating plaque-covered area by -15.5% compared to disclosed plaque photographs [45]. This confirms that the two methods are not interchangeable and that PDAs alter the fundamental optical properties QLF aims to measure.
Pitfall 3: Image Capture Conditions
Variability in image capture is a major source of non-biological variance in QLF data. Key parameters must be rigorously controlled.
- Ambient Light: Stray ambient light contributes to background noise, reducing the signal-to-noise ratio of the specific RF signal. Imaging must be performed under controlled dark conditions [45].
- Camera Settings: Inconsistent camera settings (shutter speed, aperture, ISO) directly affect fluorescence intensity measurements. For example, one standardized protocol uses shutter speed: 1/60 s, aperture: f/7.1, ISO: 1600 [44].
- Geometry and Distance: The angle and distance between the camera lens and the biofilm surface affect light intensity and collection efficiency. A fixed distance (e.g., 5 cm) and a perpendicular angle are recommended [45].
Table 1: Impact and Mitigation of Key Technical Pitfalls
| Technical Pitfall | Impact on QLF Data | Recommended Mitigation Strategy |
|---|---|---|
| Hydration Status | Overestimation of RF due to desiccation artifacts. | Standardize air-drying time (<5s) or use fully hydrated samples; consistent pre-imaging protocol. |
| Plaque-Disclosing Agents | Spectral interference; false-positive/negative RF. | Avoid use prior to QLF imaging. Use QLF as the primary detection tool. |
| Ambient Light | Decreased signal-to-noise ratio; underestimated ΔR/R/G. | Perform imaging in a darkroom or with enclosed camera systems. |
| Camera Settings | Inconsistent fluorescence intensity values. | Use fixed, predefined settings (e.g., ISO 1600, Aperture f/7.1, Shutter 1/60s). |
| Camera Geometry | Inconsistent illumination and signal capture. | Use a fixed-distance stand; maintain lens perpendicular to sample plane. |
Standardized Experimental Protocols
Protocol 1: In Vitro QLF Imaging of Microcosm Biofilms
This protocol, adapted from Lee et al., is designed for evaluating antimicrobial efficacy against cariogenic biofilms formed on enamel specimens [44].
Workflow Summary:
- Biofilm Formation: Inoculate enamel discs in 24-well plates with human saliva-derived microcosm and culture in basal medium mucin (BMM) with 0.3% sucrose under anaerobic conditions for 7 days.
- Treatment Regimen: Treat biofilms twice daily with test antimicrobials (e.g., Chlorhexidine at 0.05-0.5%) or control (distilled water) for 1 minute, followed by rinsing with cysteine peptone water (CPW).
- QLF Image Acquisition:
- Use a QLF-D Biluminator system or equivalent.
- Ensure standardized camera settings: Shutter speed: 1/60 s, Aperture: f/7.1, ISO: 1600.
- Maintain a consistent distance from the light source to the biofilm.
- Acquire images daily without disclosing agents.
- Image Analysis:
- Define an area of interest (AOI) on the fluorescence image.
- Use image analysis software (e.g., Image-Pro PLUS) to extract the red (R) and green (G) values for every pixel within the AOI.
- Calculate the average R/G value for the entire AOI to quantify RF intensity.
- Validation: Correlate R/G values with traditional endpoints like supernatant pH, microbial counts (total/aciduric bacteria), and enamel surface microhardness change (%SHC).
Diagram 1: In vitro biofilm imaging and analysis workflow
Protocol 2: In Vivo QLF Imaging for Plaque and Gingivitis Screening
This protocol outlines a standardized method for clinical plaque imaging, avoiding the pitfalls of disclosing agents [23].
Workflow Summary:
- Patient Preparation: Participants should refrain from oral hygiene for a defined period (e.g., 24 hours) prior to imaging to allow for sufficient plaque accumulation.
- Image Acquisition:
- Use a lip retractor for full visibility.
- Ensure the imaging room has controlled, dark ambient conditions.
- Use a QLF intraoral camera (e.g., Qraycam Pro). Maintain a consistent ~5 cm distance and perpendicular angle to the tooth surface.
- Capture images of anterior teeth (upper and lower) for efficient gingival health screening.
- Image Analysis:
- Calculate the percentage of the dental biofilm area exhibiting red biofluorescence relative to the total surface area of the anterior teeth.
- Clinical Correlation:
- Correlate the fluorescent biofilm area with clinical indices like the Gingival Index (GI), Bleeding-on-Probing (BOP), and Plaque Index (PI). A larger RF area is significantly correlated with higher GI and BOP scores [23].
Data Interpretation and Quantitative Benchmarks
Understanding the quantitative output from QLF analysis is crucial for valid biological interpretation. The following table summarizes key RF parameters and their reported correlations from the literature.
Table 2: Quantitative Benchmarks for Red Fluorescence in Dental Biofilms
| QLF Parameter | Measurement Target | Reported Values / Correlations | Biological / Clinical Significance |
|---|---|---|---|
| R/G Ratio | Red fluorescence intensity of biofilm. | Increases with biofilm maturation and sucrose concentration [44]. Decreases after Chlorhexidine treatment [44]. | Indicator of biofilm pathogenicity and cariogenic potential. |
| ΔR (%) | Red fluorescence intensity gain. | Used in caries detection; higher in carious lesions [9]. | Presence of bacterial porphyrins in caries and mature biofilm. |
| Fluorescent Area (%) | Proportion of tooth surface with RF. | 2.75% (No calculus), 6.06% (Initial calculus), 15.58% (Advanced calculus) [6]. Correlates with GI (r=0.422) and BOP (r=0.376) [23]. | Indicator of oral hygiene status and gingivitis risk. |
| Plaque Volume (VPI) | 3D volume of plaque deposit. | Positively correlates with Turesky plaque index but shows higher sensitivity at low plaque levels [7]. | Direct, quantitative measure of plaque accumulation; not reliant on dyes. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for QLF Biofilm Research
| Item | Function in QLF Research | Example / Specification |
|---|---|---|
| QLF-D Biluminator | Core imaging device; provides 405 nm excitation light and captures fluorescence through specific filters. | Inspektor Research Systems; equipped with blue (405 nm) and white LEDs [44]. |
| Basal Medium Mucin (BMM) | Growth medium for in vitro microcosm biofilm culture, simulating oral conditions. | Supplemented with 0.3% sucrose to induce cariogenic properties [44]. |
| Chlorhexidine (CHX) | Gold-standard antimicrobial control for validating QLF's ability to monitor treatment efficacy. | Used at 0.05%, 0.1%, and 0.5% concentrations in saline/water [44]. |
| Cysteine Peptone Water (CPW) | Neutralizing rinse to remove excess antimicrobials after treatment without disrupting biofilm. | Used after CHX treatment to stop its action [44]. |
| Image Analysis Software | Quantifies red and green fluorescence values from captured images to calculate R/G ratios. | Image-Pro PLUS, custom MATLAB or Python scripts [44]. |
| Intraoral Scanner (IOS) | Enables 3D volumetric plaque assessment (VPI) without disclosing agents, complementary to QLF. | 3Shape Trios 4; used for superimposing 3D models to calculate plaque volume [7]. |
The technical pitfalls surrounding hydration, staining, and image capture are not merely operational details but are fundamental to the scientific rigor of QLF-based dental biofilm research. The protocols and benchmarks provided herein form a foundation for generating reliable, comparable, and meaningful data. By adhering to these standardized methods, researchers can confidently use QLF technology to dissect biofilm pathogenicity, screen for gingival health, and accurately evaluate the efficacy of novel anti-biofilm therapeutics.
Within the context of quantitative light-induced fluorescence (QLF) research for dental biofilm imaging, a significant technological constraint impedes standardized data collection: the limited accessibility and performance of imaging devices within the complex anatomical geometry of the oral cavity. Specifically, the posterior teeth regions and the lingual surfaces of all teeth present considerable challenges for consistent image acquisition, affecting the reproducibility and comprehensiveness of quantitative plaque analysis. This application note details these limitations, provides quantitative evidence of performance variation, and outlines standardized protocols to validate QLF system performance across the entire dentition, a critical consideration for researchers and drug development professionals aiming to utilize this technology in clinical trials.
Quantitative Evidence of Anatomical Limitations
The performance of QLF technology varies significantly across different regions of the dentition. The following tables summarize quantitative evidence from clinical and validation studies, highlighting the disparities in plaque detection efficacy.
Table 1: Correlation between QLF-D Parameters and Clinical Indices by Tooth Surface [46]
| Tooth Surface / Region | Correlation with Gingival Index (GI) | Correlation with Bleeding on Probing (BOP) | Correlation with Probing Pocket Depth (PPD) |
|---|---|---|---|
| Buccal Surfaces | Strong positive correlation | Strong positive correlation | Strong positive correlation |
| Lingual Surfaces | No significant correlation difference vs. buccal | No significant correlation difference vs. buccal | No significant correlation difference vs. buccal |
| Anterior Teeth | Higher correlation | Higher correlation | Higher correlation |
| Posterior Teeth | Lower correlation | Lower correlation | Lower correlation |
| Mandibular Teeth | Higher correlation than maxillary teeth | Higher correlation than maxillary teeth | Higher correlation than maxillary teeth |
Table 2: Summary of Documented Challenges in Specific Anatomical Regions [46] [47]
| Anatomical Region | Documented Challenge | Impact on QLF Analysis |
|---|---|---|
| Maxillary Posterior Teeth | Difficulty in positioning the QLF-D camera head; constrained space and cheek obstruction. | Incomplete image capture, shadowing, and inconsistent angle of view, leading to non-quantifiable data. |
| Palatal Surfaces | Physical obstruction by the palate; deep curvature of the surface. | Inability to capture the entire surface, with fluorescence loss (ΔF/ΔR) at the margins. |
| Lingual Surfaces (Mandibular) | Obstruction by the tongue; proximity to the salivary ducts. | Saliva pooling causing light scattering and fluorescence quenching, reducing measurement accuracy. |
Experimental Protocols for Regional Validation
To ensure the reliability of QLF data in research applications, it is imperative to implement validation protocols that specifically assess the technology's performance in challenging anatomical regions.
Protocol for Full-Mouth QLF-D Image Acquisition and Analysis
This protocol is designed to systematically evaluate and document the limitations of QLF-D across all tooth surfaces [46].
I. Equipment and Reagent Setup
- QLF-D System: Biluminator or equivalent with a high-resolution DSLR camera.
- Analysis Software: QA2 or equivalent for calculating ΔF and ΔR values.
- Clinical Indices Toolkit: Gingival Index (GI), Bleeding on Probing (BOP), and Probing Pocket Depth (PPD) scoring tools.
- Disclosing Solution: Two-tone plaque disclosing agent (e.g., containing CI 42090 & 45410) for validation [7].
II. Step-by-Step Procedure
- Subject Preparation: Participants should refrain from oral hygiene for 4-8 hours prior to imaging to allow for standardized plaque accumulation.
- Regional Image Acquisition: Capture a series of QLF-D images according to a pre-defined segmentation of the mouth. The recommended segmentation includes 8 regions: Maxillary Right/Left Buccal, Maxillary Right/Left Palatal, Mandibular Right/Left Buccal, Mandibular Right/Left Lingual. Explicitly document any regions where the entire tooth surface cannot be visualized without obstruction.
- Clinical Examination: Following image acquisition, perform clinical examinations (GI, BOP, PPD) and apply a plaque disclosing solution to score the Turesky Modification of the Quigley-Hein Plaque Index (TMQHPI) as a reference standard.
- Digital Analysis: For each successfully captured tooth surface in the QLF-D images, use the analysis software to obtain quantitative values for fluorescence loss (ΔF) and red fluorescence (ΔR).
- Data Correlation and Comparison: Statistically correlate the QLF-D parameters (ΔF, ΔR) with the clinical plaque and gingival indices for each of the 8 regions. Use Pearson's correlation analysis.
III. Expected Outcomes and Interpretation Researchers should anticipate significantly weaker correlations between QLF-D data and clinical indices for palatal and posterior regions compared to buccal and anterior regions. Surfaces that are only partially visible should be flagged, and their data should be treated as potentially unreliable for longitudinal studies.
Protocol for Intra-Oral Scanner (IOS)-Based Volumetric Plaque Validation
For a more comprehensive 3D assessment that can overcome some QLF viewing angle limitations, this protocol uses IOS to quantify plaque volume [7].
I. Equipment and Reagent Setup
- Intraoral Scanner: High-resolution scanner (e.g., Trios 4).
- 3D Analysis Software: Software capable of superimposing and performing volumetric deviation analysis on 3D models.
- Plaque Disclosing Agent: As used in Protocol 3.1.
II. Step-by-Step Procedure
- Baseline Scan (T0): After professional prophylaxis and confirmed plaque-free status, obtain a full-arch intraoral scan of the subject. This serves as the reference model.
- Plaque Regrowth Phase: Instruct the subject to abstain from oral hygiene for 4 days.
- Follow-up Scan (T4): Obtain a second intraoral scan under identical conditions.
- Plaque Staining and Indexing: Apply a disclosing agent and record the TMQHPI for clinical reference.
- Digital Volumetric Analysis: a. Superimposition: Align the T4 scan onto the T0 reference scan using stable surfaces as landmarks. b. Region of Interest (ROI) Definition: Manually or automatically define the tooth surface margins on the 3D model. c. Volume Calculation: The software calculates the volumetric plaque index (VPI) as the positive integrated distance between the T0 and T4 surfaces, representing the plaque volume in mm³.
III. Expected Outcomes and Interpretation The VPI provides a quantitative, operator-independent measure of plaque volume. This method can capture plaque on complex surfaces like the lingual concavities of mandibular teeth and palatal surfaces of maxillary molars, which are challenging for 2D QLF. It can be used to validate the quantitative accuracy of QLF-derived parameters in these difficult regions.
Visual Workflows and Signaling Pathways
The following diagrams illustrate the experimental workflows and the logical relationship between technological challenges and proposed solutions.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and their functions for conducting the experiments described in this application note.
Table 3: Essential Research Reagents and Materials for QLF Biofilm Studies
| Item Name | Function / Application | Research Context |
|---|---|---|
| Two-Tone Plaque Disclosing Agent (e.g., Curaprox PlaqueFinder-260) | Stains mature (blue/purple) and new (pink) plaque. Provides a visual reference standard for validating QLF-D red fluorescence (ΔR) findings [7] [48]. | Critical for establishing the correlation between QLF-D signals and clinically relevant biofilm maturity stages. |
| Quantitative Light-Induced Fluorescence-Digital (QLF-D) System | Emits 405 nm light to induce tooth autofluorescence and bacterial porphyrin fluorescence. Captures images for quantitative analysis of fluorescence loss (ΔF) and red fluorescence (ΔR) [49] [46] [50]. | The primary technology under investigation for non-invasive, quantitative plaque assessment. |
| High-Resolution Intraoral Scanner (IOS) (e.g., Trios 4) | Captures 3D topographic data of the dentition. Used for volumetric plaque analysis (VPI) by comparing plaque-laden and baseline scans [7]. | Serves as a 3D reference method to overcome the viewing angle and saliva limitations of 2D QLF in posterior/lingual regions. |
| Crystal Violet Solution (0.1% w/v) | A histological dye that binds non-specifically to negatively charged molecules in biofilm biomass and cells. Used in standardized biofilm quantification assays [51]. | Useful for in vitro calibration of biomass measurements. Can be correlated with QLF-D signals to understand what is being quantified. |
| Tryptic Soy Broth (TSB) with 1% Glucose | A nutrient-rich growth medium used to promote and standardize biofilm formation in in vitro or ex vivo models [52]. | Essential for generating consistent and robust biofilms for method development and calibration purposes. |
Software and Hardware Considerations for Enhancing Measurement Reproducibility
Quantitative Light-Induced Fluorescence (QLF) imaging has emerged as a vital technology for the objective, quantitative assessment of dental biofilms. Its ability to detect bacterial metabolites through natural fluorescence provides researchers with a powerful tool to quantify plaque accumulation and pathogenicity. However, the reproducibility of measurements across different devices, software, and experimental conditions remains a critical challenge in translational dental research. This document outlines the essential software and hardware considerations and provides standardized protocols to enhance the reliability and reproducibility of QLF data in both clinical and research settings, with particular importance for pharmaceutical development and multi-site clinical trials.
Hardware Configuration and Performance
The core of QLF technology involves illuminating the oral cavity with high-intensity blue light (typically at a peak wavelength of 405 nm) and capturing the resulting autofluorescence. Sound tooth tissue fluoresces green, while cariogenic bacteria and their metabolic byproducts, such as porphyrins, emit red fluorescence (RF) due to excitation by this specific wavelength [53] [13]. The hardware must be precisely configured to standardize this process.
Device-Specific Performance Characteristics
Different QLF devices offer varying fields of view (FOV) and resolutions, which can impact their suitability for specific applications. The choice between devices should be guided by the research objective, whether it is full-arch screening or detailed analysis of a specific lesion.
Table 1: Comparison of Representative QLF Device Capabilities
| Device Model | Primary Use Case | Field of View (FOV) | Image Sensor Resolution | Key Strengths |
|---|---|---|---|---|
| Qraycam Pro (QP) [13] | Individual teeth & proximal surfaces | Smaller FOV | CMOS (FHD 1080p) | Detailed imaging for precise lesion analysis; superior for secondary caries assessment. |
| Qraypen C (QC) [13] | Full-arch screening | Larger FOV | CMOS (HD 720p) | Efficient for overall dental condition screening and identifying regions of interest. |
| QRayCam TM Pro [31] | Anterior teeth plaque quantification | Not Specified | Not Specified | High repeatability (p < 0.0001); validated for plaque quantitation in regulatory science. |
| TRIOS 4 Scanner [53] | 3D model creation with fluorescence | Intraoral Scanner | Not Specified | Integrates fluorescence with 3D topography; enables automated caries scoring. |
Key Hardware Considerations for Reproducibility
- Calibration: Regularly calibrate the light source and sensor according to the manufacturer's specifications to ensure consistent fluorescence excitation and capture.
- Fixed Positioning: Use mechanical aids (e.g., chin rests, camera stands) to maintain a consistent distance and angle between the camera and the subject. This minimizes measurement variability introduced by operator handling.
- Environmental Control: Conduct imaging in a controlled lighting environment to avoid contamination from ambient light. Standardize pre-imaging patient instructions regarding eating, drinking, and oral hygiene [31].
Software Analysis and Standardization
Software is critical for extracting quantitative data from QLF images. Variations in analysis algorithms or parameter settings can significantly impact results.
Core QLF Parameters
The following parameters are commonly used to quantify dental plaque and caries lesions, with their relevance depending on the research focus:
- ΔFaver. (Average Fluorescence Loss): Represents the average percentage of fluorescence loss in a lesion area compared to sound enamel, correlating with mineral loss. It shows high diagnostic accuracy for occlusal caries (AUC 0.87-0.99) [13].
- ΔR (Red Fluorescence): Quantifies the intensity of red fluorescence emitted by bacterial porphyrins. It is a key indicator of mature and pathogenic biofilms and is particularly useful for assessing secondary caries and tongue coating pathogenicity [5] [13].
- Plaque Coverage (%): Measures the percentage of tooth surface covered by plaque, as identified by its red fluorescence [31].
- Integrated Fluorescence (IF) Score: A composite metric, often the product of plaque coverage and intensity, used in indices like the Tongue Biofilm Fluorescence Index (TBFI) to simultaneously evaluate the quantitative and qualitative aspects of biofilms [5].
Software Workflow for Standardized Analysis
The process of analyzing dental biofilms with QLF technology, from image acquisition to data interpretation, can be standardized into a cohesive workflow to ensure consistency across studies and devices.
Diagram 1: Standardized QLF image analysis workflow. Key steps ensure consistent data generation.
Experimental Protocols for Enhanced Reproducibility
Protocol: Validating QLF Measurement Repeatability
This protocol is adapted from a study that demonstrated high short- and long-term repeatability of QLF measurements [31].
Objective: To determine the intra- and inter-examiner reproducibility of dental plaque quantitation using a QLF device over time.
Materials:
- QLF imaging device (e.g., QRayCam TM Pro)
- Calibration standards
- Timer
- Data collection form
Method:
- Participant Selection and Preparation: Recruit subjects according to predefined inclusion/exclusion criteria. Standardize the time of day for imaging and instruct participants to refrain from eating, drinking (except water), smoking, and performing oral hygiene for at least 2 hours before each visit [31].
- Baseline Imaging (Visit 1, Day 0):
- Calibrate the QLF device.
- Position the participant using a headrest and fixed camera stand.
- Capture standardized images of the target teeth (e.g., anterior teeth from cuspid to cuspid).
- Follow-up Imaging:
- Short-term Repeatability (Visit 2, Day 7 ± 1): Repeat the imaging procedure under identical conditions.
- Long-term Repeatability (Visit 3, Day 30 ± 3): Repeat the imaging procedure again.
- Data Analysis:
- Analyze all images using the same software version and parameter thresholds (e.g., ΔR30, ΔR120).
- For intra-examiner agreement, have one examiner analyze all images twice, with a washout period of at least 4 weeks between scoring sessions [53].
- For inter-examiner agreement, have at least two calibrated examiners analyze the images independently while blinded to each other's scores and subject groups.
- Statistical Analysis: Calculate Intraclass Correlation Coefficients (ICC) for quantitative data (excellent >0.9) and Cohen's Kappa (κ) for categorical indices (substantial >0.6) [31] [5].
Protocol: On-Screen Assessment of 3D Fluorescence Models
This protocol leverages intraoral scanners with integrated fluorescence for caries and biofilm detection [53].
Objective: To assess the diagnostic agreement between visual examination and on-screen assessment of 3D digital models with and without fluorescence for caries detection.
Materials:
- Intraoral scanner with fluorescence technology (e.g., TRIOS 4)
- Software for viewing 3D models (e.g., 3Shape platform)
- Approved scoring index (e.g., merged ICDAS index modified for fluorescence)
Method:
- Model Acquisition: Create 3D digital models of the participant's dentition using the intraoral scanner. Ensure both geometry and fluorescence texture data are captured.
- Examiner Calibration: Train and calibrate all examiners (e.g., dental practitioners) on the use of the chosen index for on-screen assessment.
- Blinded Assessment:
- Phase 1: Examiners assess the 3D models using only geometry and approximate natural color texture. They score caries using the merged ICDAS index.
- Washout Period: Implement an interval of at least 4 weeks to minimize recall bias.
- Phase 2: Examiners reassess the same 3D models, this time with the fluorescence texture enabled. They score caries using the same index, now incorporating fluorescence criteria (e.g., red fluorescence indicates bacterial activity).
- Data Analysis: Use multilevel models to estimate agreement at the tooth surface level, accounting for the clustering of teeth within patients. Compare agreement between the two phases [53].
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for QLF Biofilm Studies
| Item | Function/Application | Example Use Case |
|---|---|---|
| QLF Imaging Device | Captures fluorescence images of teeth and soft tissues for quantitative analysis of biofilm. | Plaque quantitation in clinical trials; monitoring caries progression [31] [13]. |
| Intraoral Scanner (FLI-enabled) | Creates 3D digital models with superimposed fluorescence data for topographic and biologic assessment. | Automated caries scoring; remote assessment (teledentistry) [53]. |
| Analysis Software (QA2) | Extracts and calculates key QLF parameters (ΔF, ΔR, coverage) from captured images. | Objective quantification of biofilm burden and mineral loss in longitudinal studies [13]. |
| Calibration Standards | Ensures consistency of light output and sensor sensitivity of the QLF device over time. | Routine quality control to maintain measurement reproducibility across study timepoints [31]. |
| Validated Indices (TBFI) | Standardized scoring system for objective and reliable classification of biofilm severity. | Tongue biofilm assessment with high inter-examiner reliability (κ = 0.752) [5]. |
Achieving high measurement reproducibility in QLF dental biofilm imaging requires a systematic approach that integrates standardized hardware operation, rigorous software analysis protocols, and meticulously planned experimental procedures. By adhering to the considerations and protocols outlined in this document, researchers can generate robust, reliable, and comparable data. This is foundational for advancing the role of QLF as an endpoint in regulatory science, clinical trials, and evidence-based dental research.
Benchmarking Performance: Validating QLF Against Clinical Indices and Diagnostic Standards
Within the broader scope of a research thesis focused on quantitative light-induced fluorescence (QLF) dental biofilm imaging, establishing the technology's fundamental diagnostic performance for caries detection is paramount. QLF technology leverages the natural biofluorescence of dental hard tissues and bacterial metabolites to detect and quantify demineralization non-invasively [4] [9]. This document provides a synthesized analysis of QLF's diagnostic accuracy, derived from recent high-quality meta-analyses, and outlines standardized protocols to ensure consistency in future research and clinical validation studies. The transition towards non-ionizing radiation-based diagnostic methods in modern caries management underscores the critical importance of this evidence-based evaluation [4].
Comprehensive Diagnostic Performance Data
A recent systematic review and meta-analysis (2025) provides the most current and comprehensive evaluation of QLF's capabilities, analyzing data from 17 studies that included both in vivo and in vitro designs [4] [9]. The analysis stratified performance by lesion severity, tooth surface, and dentition type, using established reference standards like ICDAS (International Caries Detection and Assessment System), radiography, and histology [4].
The tables below summarize the key performance metrics for occlusal and proximal caries detection.
Table 1: Summary of QLF Diagnostic Accuracy for Occlusal Caries (In Vivo)
| Lesion Threshold | Sensitivity Range | Specificity Range | AUC Range | Pooled Sensitivity | Pooled Specificity |
|---|---|---|---|---|---|
| Incipient (ICDAS 1-2) vs. Advanced Enamel (ICDAS 3) | 0.76 – 0.91 | 0.74 – 0.93 | 0.81 – 0.93 | - | - |
| Sound/Enamel vs. Dentinal (ICDAS 4+) | 0.90 – 0.98 | 0.83 – 0.96 | 0.94 – 0.98 | 0.86 | 0.82 |
Table 2: Summary of QLF Diagnostic Accuracy by Surface and Setting [4]
| Surface | Setting | Pooled Sensitivity | Pooled Specificity |
|---|---|---|---|
| Occlusal | In Vivo | 0.86 | 0.82 |
| Occlusal | In Vitro | 0.83 | 0.74 |
| Proximal | In Vivo | 0.74 | 0.82 |
| Proximal | In Vitro | 0.83 | 0.74 |
Table 3: Performance of Different QLF Devices in a Clinical Study (2022) [13]
| Device | Field of View | Occlusal Caries Accuracy (D1 Threshold) | Occlusal Caries Accuracy (D2 Threshold) | Proximal Caries Accuracy |
|---|---|---|---|---|
| Qraypen C (QC) | Small | 0.83 | 0.96 | 0.52 – 0.62 |
| Qraycam Pro (QP) | Large | 0.81 | 0.82 | 0.52 – 0.71 |
Key Findings:
- QLF demonstrates excellent diagnostic accuracy for occlusal caries, particularly in distinguishing sound surfaces from dentinal lesions, with in vivo AUC values as high as 0.98 [4].
- Performance for proximal caries is good, though generally lower than for occlusal surfaces, reflecting the greater diagnostic challenge of these lesions [4] [13].
- The technology shows high specificity, indicating a strong ability to correctly identify sound tooth surfaces, which is crucial for preventing unnecessary treatment [4].
Detailed Experimental Protocols
To ensure reproducibility and standardization across studies, the following protocols detail the core methodologies for validating QLF in both laboratory and clinical settings.
In Vitro Validation Protocol
This protocol is designed for the histological validation of QLF findings on extracted teeth, providing a controlled environment for precise correlation.
Sample Preparation:
- Tooth Selection: Secure extracted human teeth (permanent or primary) and obtain ethical approval. Exclude teeth with hypoplasia, cracks, or restorations that obscure the study surfaces [16].
- Cleaning and Storage: Clean teeth with a pumice slurry and soft brush. Store in thymol solution (0.1%) to prevent dehydration and microbial growth [9].
- Reference Standard: Perform a pre-extraction QLF examination where feasible to bridge in vivo and in vitro findings [9].
Image Acquisition:
- QLF Device Setup: Use a calibrated QLF system (e.g., QLF-D, Inspektor Pro). Ensure the imaging chamber is light-proof [9].
- Standardized Imaging: Position the tooth so the laser beam is perpendicular to the surface of interest. Dry the surface with compressed air for 5-10 seconds prior to image capture [16].
- Parameter Acquisition: Capture both white-light and fluorescence images. The analysis software will quantify:
Histological Validation (Reference Standard):
- Sectioning: Embed teeth in resin and section through the suspected lesion using a hard tissue microtome (≈200-300 µm thick sections) [9].
- Staining and Microscopy: Stain sections with Rhodamine B or perform transverse microradiography (TMR). Examine under a polarized light microscope or digital microscope by a blinded, experienced examiner [9].
- Lesion Scoring: Score the lesion depth according to a standardized scale (e.g., ICDAS adapted for histology) [4] [9].
Data Analysis:
- Correlation: Correlate QLF parameters (ΔF, ΔR) with histological lesion depth scores using statistical analyses (e.g., Pearson's correlation).
- Diagnostic Test Accuracy: Construct 2x2 contingency tables against the histological reference to calculate sensitivity, specificity, and AUC [4].
In Vivo Clinical Validation Protocol
This protocol is designed for clinical studies comparing QLF against routine diagnostic methods like visual examination and radiography.
Subject Selection:
- Inclusion Criteria: Recruit adult subjects (≥18 years) providing informed consent. Target teeth should be permanent premolars and molars [16].
- Exclusion Criteria: Exclude subjects with systemic diseases, severe periodontitis, or teeth with cavitations (ICDAS 6), hypoplasia, or large restorations on the study surfaces [16].
Clinical Examination Workflow: The following diagram outlines the sequential steps for a clinical validation study.
Examination Procedures:
- Visual-Tactile Examination (Index Test 1): Conduct by a calibrated examiner using ICDAS II criteria. Record scores for all tooth surfaces [13] [16].
- QLF Examination (Index Test 2):
- Device: Use a clinical QLF device like Qraypen C or Qraycam Pro [13].
- Environment: Perform in a dimly lit or dark room. Use a cheek retractor for access [16].
- Procedure: Dry the occlusal surface with compressed air. Position the device tip vertically ~5 mm from the surface. Capture and save both white-light and fluorescence images in bitmap format [16].
- Analysis: Use proprietary software (e.g., QA2) to obtain quantitative ΔF and ΔR values for the region of interest [13] [16].
- Radiographic Examination (Reference Standard):
Data Analysis:
- Calculate inter- and intra-examiner reliability for all diagnostic methods (e.g., Cohen's Kappa, Intraclass Correlation Coefficient) [9].
- Determine QLF's sensitivity, specificity, and AUC against the radiographic reference standard [4] [13] [16].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 4: Key Materials and Reagents for QLF Caries Detection Research
| Item Name | Function/Application | Example Specifications |
|---|---|---|
| QLF-D Biluminator 2 | In vitro imaging system; provides standardized blue light (405 nm) excitation for high-resolution fluorescence image capture. | 405 nm LED array, integrated camera, proprietary software suite (QA2). |
| Qraypen C | Handheld, pen-type intraoral device; enables detailed imaging of individual teeth and proximal surfaces in clinical settings. | 405 nm peak wavelength, HD 720p CMOS sensor [13]. |
| Qraycam Pro | Intraoral camera with wide field of view; suitable for full-arch screening and plaque assessment in clinical and research settings. | FHD 1080p CMOS sensor, Inspektor glass filter [13] [3]. |
| QA2 Software | Proprietary analysis software; quantifies key parameters ΔF (fluorescence loss) and ΔR (red fluorescence) from captured images. | Modules for caries, plaque, and staining analysis [13] [16]. |
| ICDAS II Criteria | Visual-tactile reference standard; provides a validated system for scoring caries severity and activity during clinical examination. | 7-point scale (0: sound to 6: distinct cavitation). |
| Two-Tone Disclosing Solution | Plaque maturation reference; stains young plaque pink and mature plaque blue for validation of QLF's red fluorescence (ΔR) for biofilm [18]. | e.g., Trace disclosing solution. |
QLF Technology Workflow and Diagnostic Principles
The diagnostic power of QLF stems from two core optical phenomena, which are quantified and interpreted through a defined workflow.
Interpretation of Parameters:
- ΔF (Delta F): A more negative ΔF value indicates greater mineral loss and a more advanced carious lesion. It is the primary parameter for monitoring lesion progression or regression over time [4] [9].
- ΔR (Delta R): A positive ΔR value indicates the presence of metabolically active bacteria and mature biofilm. This is particularly useful for assessing lesion activity and the effectiveness of antimicrobial agents [4] [18] [16].
Within the broader scope of a thesis on quantitative light-induced fluorescence (QLF) dental biofilm imaging, this document establishes the technology's validity as a quantitative research tool. The core objective of this research is to transition from subjective, conventional clinical indices to an objective, fluorescence-based imaging system for dental plaque quantification. Quantitative Light-induced Fluorescence-Digital (QLF-D) technology operates on the principle of bacterial biofluorescence. It uses blue visible light (405 nm) to induce natural tooth autofluorescence and to detect red fluorescence emitted by bacterial metabolites, such as porphyrins, within the dental biofilm [4] [46]. This red fluorescence, quantified as the ΔR value, provides a direct and objective measure of biofilm presence and maturity [54] [3].
This application note details the correlation between QLF-D measurements and established clinical indices—Gingival Index (GI), Bleeding on Probing (BOP), Probing Pocket Depth (PPD), and Patient Hygiene Performance (PHP) index—thereby positioning QLF-D as an essential methodology for researchers and drug development professionals for non-invasive, precise plaque scoring.
Data Presentation: Correlation of QLF-D with Conventional Indices
The following tables consolidate quantitative data from key studies, demonstrating the significant relationships between QLF-D parameters and traditional clinical metrics.
Table 1: Summary of Correlation Coefficients between Full-Mouth QLF-D Score and Clinical Indices
| Clinical Index | Correlation Coefficient (r) | p-value | Study |
|---|---|---|---|
| Gingival Index (GI) | 0.749 | < 0.01 | [54] [46] |
| Bleeding on Probing (BOP) | 0.736 | < 0.01 | [54] [46] |
| Patient Hygiene Performance (PHP) Index | 0.714 | < 0.01 | [54] [46] |
| Probing Pocket Depth (PPD) | 0.683 | < 0.01 | [54] [46] |
Table 2: Correlation of QLF-D Across Dental Arches and Surfaces
| Oral Region | Correlation Trend with QLF-D Score | Notes |
|---|---|---|
| Mandible vs. Maxilla | Higher correlation in the mandible | [54] [46] |
| Anterior vs. Posterior Teeth | Higher correlation in anterior teeth | Anterior teeth biofilm area is an effective indicator for gingival health screening [3]. |
| Buccal vs. Lingual Surfaces | No significant difference | Correlations were consistently high on both surfaces [54] [46]. |
Table 3: Diagnostic Accuracy of Fluorescence-Based Caries Detection (QLF)
| Condition | Surface | Sensitivity | Specificity | Area Under the Curve (AUC) |
|---|---|---|---|---|
| In Vivo Occlusal Caries | Occlusal | 0.86 | 0.82 | 0.94 - 0.98 |
| In Vivo Proximal Caries | Approximal | 0.74 | 0.82 | 0.67 - 0.91 |
Experimental Protocols
Protocol 1: Full-Mouth Dental Plaque Assessment Using QLF-D
This protocol is designed to validate QLF-D against conventional indices in a clinical research setting [54] [46].
- Hypothesis: The QLF-D plaque score exhibits a statistically significant positive correlation with the GI, BOP, PPD, and PHP index.
- Subject Recruitment & Inclusion Criteria:
- Recruit adult participants (e.g., ≥ 20 years old).
- Inclusion: Participants with relatively even teeth, a minimum of 24 teeth, and good general health.
- Exclusion: Orthodontic brackets, severe crowding, extensive fixed or implant restorations, and serious systemic diseases.
- Sample Size Calculation: Use statistical power analysis software (e.g., G*Power). For a correlation study with an effect size of 0.3, an error rate of 5%, and statistical power of 80%, a sample of approximately 33 subjects is required [46].
- Ethical Considerations: The study must be approved by an Institutional Review Board (IRB). All participants must provide written informed consent [54] [46].
- Materials & Equipment:
- QLF-D imaging system (e.g., Biluminator).
- DSLR camera (e.g., Canon EOS 650D).
- QLF-D analysis software (e.g., QA2 v1.23).
- Sterile periodontal probe.
- Dental disclosing solution.
- Data collection forms.
- Procedure:
- Subject Preparation: Participants should visit the clinic without having brushed their teeth after their last meal to allow for plaque accumulation.
- QLF-D Image Acquisition:
- Divide the mouth into 8 segments: (Maxilla/Mandible) x (Left/Right) x (Anterior/Posterior). Image both buccal and lingual surfaces.
- Use standardized camera settings: shutter speed 1/30 s, aperture f/5.6, ISO 1600 for fluorescence mode [46].
- Ensure the camera is fixed at a consistent distance and angle from the teeth for reproducible images.
- Clinical Indices Assessment:
- Gingival Index (GI) & Bleeding on Probing (BOP): Use a periodontal probe to assess the gingival condition around each tooth. Record GI scores (0-3) and note any bleeding within 30 seconds of probing [54] [46].
- Probing Pocket Depth (PPD): Measure the depth from the gingival margin to the base of the sulcus/pocket at six sites per tooth [54] [46].
- PHP Index: Apply disclosing solution to stain the plaque. Score the presence of plaque on six areas (mesial, distal, buccal, lingual, and two central areas) of each tooth [54] [46].
- QLF-D Image Analysis:
- Using the analysis software, calculate the QLF-D score and the ΔR value for each imaged surface. The ΔR value represents the level of red fluorescence [54].
- Data Analysis:
- Calculate the mean full-mouth QLF-D score and the mean scores for each clinical index per subject.
- Perform Pearson's correlation analysis to determine the relationship between the mean QLF-D score and each clinical index (GI, BOP, PPD, PHP). A p-value of < 0.05 is considered statistically significant.
Protocol 2: Anterior Teeth Biofilm Screening for Gingival Health
This streamlined protocol is optimized for efficient screening and identifying individuals at high risk for gingivitis using only the anterior teeth [3].
- Purpose: To evaluate the efficacy of anterior dental biofilm biofluorescence as a screening tool for gingival health status.
- Imaging Setup:
- Use a portable QLF device (e.g., Qraycam Pro).
- Capture fluorescence images of the upper and lower anterior teeth.
- Analysis:
- Using proprietary software, calculate the percentage of the anterior tooth surface area that exhibits red biofluorescence.
- Categorize participants into groups based on the fluorescent biofilm area (e.g., "larger area" vs. "smaller area").
- Clinical Correlation:
- Assess GI, BOP, and PI for all participants.
- Use logistic regression analysis, adjusted for confounders like smoking and demographics, to calculate the odds ratio for moderate gingivitis between the groups with larger and smaller fluorescent biofilm areas.
Workflow and Conceptual Diagrams
The following diagram illustrates the integrated experimental workflow for validating QLF-D imaging against conventional clinical indices, as detailed in the protocols.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Materials and Reagents for QLF-D Biofilm Research
| Item | Function/Description | Example/Specification |
|---|---|---|
| QLF-D Imaging System | Core device for capturing fluorescence images of teeth and biofilm. | Biluminator; Qraycam Pro [54] [3] |
| Analysis Software | Quantifies red fluorescence (ΔR) and calculates plaque scores from acquired images. | QA2 v1.23 [46] |
| Periodontal Probe | For clinical assessment of GI, BOP, and PPD. | Standard, marked periodontal probe [54] |
| Disclosing Solution | Stains dental plaque for visual assessment of the PHP index. | Erythrosin-based or two-tone solutions [46] |
| Calibration Standards | Ensures consistency and reproducibility of QLF-D measurements over time. | Fluorescent or reflective standards for device calibration |
Within dental biofilm imaging research, effective patient education and motivation are pivotal for successful preventive care. The paradigm is shifting from merely treating oral disease to empowering patients with visual tools that enable self-management of their oral health. This analysis focuses on two primary technologies for biofilm visualization: traditional plaque disclosing agents and advanced Quantitative Light-induced Fluorescence (QLF) imaging. While disclosing agents have served as the conventional gold standard for decades, QLF technology represents an emerging modality that offers unique advantages for both clinical application and scientific investigation. This document provides researchers, scientists, and drug development professionals with a structured comparison of these technologies, detailing their mechanisms, experimental protocols, and applications within patient-centered care frameworks. The content is situated within a broader thesis on dental biofilm imaging, emphasizing evidence-based methodologies for integrating these tools into research and clinical practice.
Plaque Disclosing Agents
Plaque disclosing agents are chemical formulations containing dyes that selectively bind to dental biofilm. They function as a direct staining technique, typically utilizing plant-based colorants (e.g., erythrosine) that temporarily adhere to the pellicle and bacterial components of plaque [55]. These agents make otherwise invisible biofilm visually apparent, typically as a colored coating on tooth surfaces. Advanced two-tone variants provide additional diagnostic information by differentiating plaque maturity: typically staining younger plaque pink and more mature, older plaque a bluish color [18]. This color differentiation occurs due to variations in biofilm permeability and composition, with mature biofilm exhibiting distinct binding characteristics for specific dyes.
Quantitative Light-Induced Fluorescence (QLF)
QLF technology operates on principles of optical fluorescence. When illuminated with high-energy violet-blue light at a specific wavelength (405 nm), bacterial metabolites within dental biofilm—particularly endogenous porphyrins—absorb this light and re-emit it as red fluorescence [45] [3]. Sound tooth structure, by contrast, exhibits strong green fluorescence. QLF devices capture this fluorescence response and utilize specialized software to quantify biofilm presence and distribution. The intensity of red fluorescence correlates with both biofilm age and metabolic activity, providing a non-invasive measurement of not just plaque presence but also its pathological potential [18]. Recent iterations like QLF-D (Digital) enhance red fluorescence detection sensitivity, while portable devices like Qraycam Pro facilitate clinical application [45] [3].
Table 1: Fundamental Characteristics of Biofilm Detection Technologies
| Characteristic | Plaque Disclosing Agents | Quantitative Light-Induced Fluorescence |
|---|---|---|
| Fundamental Principle | Chemical staining | Optical fluorescence |
| Detection Basis | Direct dye binding to biofilm | Red fluorescence from bacterial porphyrins |
| Maturity Detection | Yes (via two-tone agents) | Yes (via fluorescence intensity) |
| Output Format | Visual color display on teeth | Digital image with quantitative analysis |
| Primary Measurement | Planimetric coverage (%) | Fluorescence parameters (ΔR, ΔF) and area |
Experimental Protocols for Comparative Studies
Protocol for Plaque Assessment Using Disclosing Agents
Objective: To quantify disclosed plaque coverage planimetrically as a reference standard.
Materials:
- Two-tone disclosing solution (e.g., containing dyes that stain young plaque pink and mature plaque blue) [18]
- Standardized photographic setup: Digital Single-Lens Reflex (DSLR) camera, ring flash, cheek retractors, standardized background
- Photo mirror for lingual surfaces (e.g., Dent-o-care photo mirror) [45]
- Image analysis software (e.g., Adobe Photoshop, ImageJ)
Procedure:
- Patient Preparation: Instruct patients to refrain from oral hygiene measures for 24 hours prior to assessment to ensure sufficient plaque accumulation [45].
- Initial Imaging: Capture baseline white-light photographs of the dentition using a standardized photographic protocol.
- Plaque Disclosure: Apply the two-tone disclosing solution to all tooth surfaces using a saturated foam pellet. Have the patient rinse with water for 10 seconds to remove excess dye [45].
- Post-Disclosure Imaging: Immediately capture standardized photographs of all tooth surfaces, including lingual aspects using a photo mirror. Maintain consistent camera settings (resolution, shutter speed, aperture, ISO, white balance) across all subjects [18].
- Image Analysis:
- Convert images to grayscale in image processing software.
- Manually define the region of interest (total tooth surface excluding brackets/gaps).
- Set a standardized brightness threshold (e.g., 90 on a 0-255 scale) to differentiate stained plaque from clean tooth surface.
- Use batch processing in ImageJ to calculate the percentage of plaque-covered surface area.
- For maturity assessment, score plaque as: 0 (no staining), 1 (pink staining), or 2 (blue staining) [18].
Protocol for Plaque Assessment Using QLF Technology
Objective: To quantitatively assess dental plaque via red fluorescence imaging.
Materials:
- QLF imaging device (e.g., QLF-D Biluminator, Qraycam Pro)
- Computer with proprietary analysis software
- Cheek retractors
- Headrest or positioning device
Procedure:
- Patient Preparation: Maintain identical pre-assessment conditions as the disclosing agent protocol (24-hour plaque accumulation) for direct comparison.
- Environment Setup: For QLF-D imaging, conduct assessments in a darkened room to minimize ambient light interference [45].
- Image Acquisition: Position the patient with a headrest for stability. Use cheek retractors for full tooth exposure. Capture QLF images of labial and lingual surfaces (via mirror) at a standardized distance (e.g., 5 cm) and perpendicular angle to the tooth surface [45].
- Image Analysis:
- Transfer images to proprietary analysis software.
- Manually select the tooth surfaces as regions of interest, excluding artifacts.
- The software automatically calculates the red fluorescence intensity and the percentage of surface area exhibiting significant fluorescence.
- Alternatively, export images for analysis in standard image software (e.g., ImageJ) using a higher grayscale threshold (e.g., 180) to account for fluorescence characteristics [45].
- For maturity correlation, calculate the Red/Green (R/G) ratio from RGB values in fluorescent images, with higher ratios indicating more mature plaque [18].
Protocol for Integrated Assessment in Patient Education Studies
Objective: To evaluate the efficacy of each visualization method for patient education and motivation.
Materials:
- All materials from sections 3.1 and 3.2
- Validated questionnaires on oral health knowledge, self-efficacy, and behavior
- Periodontal examination tools (gingival index, bleeding on probing assessment)
Procedure:
- Baseline Assessment: Record baseline plaque levels (QLF and disclosing agents), gingival health status (Gingival Index, Bleeding on Probing), and oral hygiene knowledge/self-efficacy via questionnaire [3] [55].
- Randomized Group Assignment: Randomly assign participants to an education intervention group using either QLF feedback or disclosing agent feedback.
- Educational Intervention:
- QLF Group: Show patients their QLF images, explaining the correlation between red fluorescence, plaque maturity, and gingival health risk. Use the visual feedback to demonstrate areas requiring improved hygiene [3].
- Disclosing Agent Group: Have patients use a mirror to view their disclosed plaque. Guide them to identify stained areas and instruct on proper cleaning techniques for different tooth surfaces [55].
- Motivational Follow-up: Implement a structured follow-up schedule (e.g., 2 weeks, 1 month, 3 months) with repeated imaging and feedback [55].
- Outcome Measurement: At defined endpoints, reassess plaque levels, gingival health, and psychological metrics (knowledge, self-efficacy, adherence) to compare the long-term motivational impact of each method.
Comparative Data and Research Findings
Quantitative Performance Data
Recent studies provide direct comparisons between QLF and disclosing agents, yielding critical performance data for research applications.
Table 2: Quantitative Comparison of Plaque Detection Performance
| Performance Metric | Plaque Disclosing Agents | QLF Technology | Research Context |
|---|---|---|---|
| Mean Plaque Detection | 36.2% ± 23.5 [45] | 20.7% ± 17.4 [45] | Orthodontic patients |
| Correlation with Gingival Index | 0.499 (PI correlation) [3] | 0.422 (GI correlation) [3] | Gingivitis screening |
| Correlation with Bleeding on Probing | 0.376 (PI correlation) [3] | 0.376 (direct correlation) [3] | Gingivitis screening |
| Maturity Detection Capability | Yes (via two-tone color) [18] | Yes (via R/G ratio: 1.21→1.46 with maturity) [18] | Plaque maturation study |
| Odds Ratio for Gingivitis Detection | Not reported | 6.07 (high vs. low fluorescence) [3] | Risk assessment |
Analytical Workflow for Research Applications
The following diagram illustrates the integrated experimental workflow for comparative studies of these technologies:
Diagram 1: Experimental workflow for comparative studies
The Scientist's Toolkit: Essential Research Materials
Table 3: Key Research Reagent Solutions and Essential Materials
| Item | Function/Application in Research | Example Specifications |
|---|---|---|
| Two-Tone Disclosing Solution | Differentiates plaque maturity by staining young biofilm pink and mature biofilm blue [18] | Plant-based formulation (e.g., Mira-2-Ton) |
| QLF Imaging System | Captures and quantifies red fluorescence from bacterial porphyrins in biofilm [45] [3] | QLF-D Biluminator or Qraycam Pro |
| Standardized DSLR Camera Setup | Captures high-resolution images of disclosed plaque for planimetric analysis [45] [18] | DSLR with macro lens, ring flash, standardized settings |
| Image Analysis Software | Quantifies plaque coverage percentage from both disclosed and QLF images [45] | ImageJ with custom macros or proprietary QLF software |
| Plaque Control Record Card | Documents plaque distribution patterns for longitudinal tracking [55] | Chart with dental schematic for manual plaque mapping |
Application in Patient Education and Motivation
Educational Efficacy and Psychological Impact
Both technologies serve distinct roles in patient education paradigms. Disclosing agents provide immediate, tangible feedback that effectively demonstrates plaque distribution after brushing. Studies implementing Guided Biofilm Therapy (GBT) protocols show that when patients use disclosing agents at home as part of structured oral hygiene instruction, they achieve significant reductions in Plaque Index (PI), Bleeding on Probing (BOP), and pocket depth (PD) compared to traditional education alone [55]. The direct visual evidence of cleaning efficacy motivates behavioral change through immediate reinforcement.
QLF technology offers a more sophisticated educational narrative by linking fluorescence patterns to oral health risk. Research demonstrates that the red fluorescence area in anterior teeth significantly correlates with standard gingival health indicators (GI, BOP), allowing clinicians to frame plaque control within the context of inflammatory disease prevention [3]. Patients with larger fluorescent biofilm areas exhibit 6.07 times higher odds of having moderate gingivitis, providing a powerful risk communication tool [3]. This technology effectively shifts the patient dialogue from simple plaque removal to managing biofilm pathogenicity.
Practical Implementation Framework
The following diagram outlines the decision pathway for implementing these technologies in patient education protocols:
Diagram 2: Technology selection pathway for patient education
This comparative analysis demonstrates that both plaque disclosing agents and QLF technology offer distinct yet complementary value in patient education and motivation frameworks. Disclosing agents provide a cost-effective, immediately accessible method for teaching mechanical plaque removal techniques, while QLF technology enables sophisticated risk communication based on biofilm pathogenicity. For research applications, the selection between these technologies should be guided by study objectives: disclosing agents remain valuable for studies focusing on mechanical cleaning efficacy, while QLF offers superior capabilities for investigations linking biofilm characteristics to disease risk and progression. Future research directions should explore synergistic applications of both technologies in stratified patient education protocols and investigate the longitudinal impact of fluorescence-based feedback on patient motivation and clinical outcomes.
Quantitative Light-Induced Fluorescence (QLF) is an advanced optical technology that utilizes visible light at a wavelength of 405 nm along with specialized filters to enable non-invasive and automatic acquisition of fluorescence images from dental tissues and bacterial biofilms [9]. This imaging approach is based on two primary diagnostic principles: first, it detects the reduction in natural fluorescence intensity (quantified as ΔF) that occurs when carious lesions demineralize, as decreased mineral content leads to increased light scattering [9]. Second, QLF captures the red fluorescence (quantified as ΔR) emitted by bacterial metabolites such as porphyrins, which are prevalent in oral biofilms and carious lesions [9]. This dual-parameter capability allows for real-time assessment of both caries severity and biofilm activity, making QLF a comprehensive tool for dental diagnostics that supports visual examinations in clinical settings where traditional methods like visual-tactile examination and radiographic assessment demonstrate markedly low sensitivity for detecting subtle initial enamel demineralization [9].
The technology's capacity for digital image documentation and storage facilitates continuous monitoring of lesion progression or regression over time, significantly enhancing patient communication and motivation [9]. Furthermore, as a non-ionizing radiation method, QLF presents a safe adjunctive approach that aligns with the latest ORCA-EFCD consensus recommendations, which acknowledge the limitations of relying solely on visual examination and suggest that supplemental methods can improve diagnostic accuracy [9]. The clinical utility of QLF extends across various applications, including early caries detection, dental plaque quantification, and assessment of lesion activity, positioning it as a versatile tool for both clinical practice and research settings focused on preventive dentistry and minimal intervention approaches.
Diagnostic Performance Data
Comprehensive Diagnostic Accuracy of QLF
Recent evidence from a systematic review and meta-analysis encompassing 17 studies demonstrates that QLF technology provides excellent diagnostic accuracy in distinguishing sound tooth surfaces from both enamel and dentin caries lesions [9]. The analysis revealed particularly impressive in vivo Area Under the Curve (AUC) values for incipient occlusal lesions, ranging from 0.94 to 0.98, indicating outstanding discriminatory capability [9]. For occlusal caries detection in clinical settings, QLF achieved pooled sensitivity of 0.86 and specificity of 0.82, while for the more challenging approximal caries, it maintained robust performance with sensitivity of 0.74 and specificity of 0.82 [9]. This performance is notably superior to traditional diagnostic methods, especially for early-stage lesions where visual-tactile examination often fails to detect demineralization before cavitation occurs.
The diagnostic performance of QLF varies according to lesion severity, with the technology demonstrating enhanced capability in detecting more advanced lesions. When examining different lesion thresholds, QLF shows exceptional performance in distinguishing sound surfaces from enamel caries and dentin caries, confirming its effectiveness for both early-stage detection and more advanced lesion identification [9]. The stratification of enamel lesions into incipient (ICDAS 1-2) and advanced stages (ICDAS 3), with dentin caries defined as ICDAS 4 or greater, provides a standardized framework for assessing QLF performance across the caries continuum [9].
Table 1: Diagnostic Performance of QLF Technology for Caries Detection
| Measurement Type | Surface | Sensitivity | Specificity | AUC | Study Setting |
|---|---|---|---|---|---|
| Occlusal Caries | Occlusal | 0.86 | 0.82 | 0.94-0.98 | In vivo |
| Approximal Caries | Proximal | 0.74 | 0.82 | - | In vivo |
| Enamel Lesions | Various | 0.966 | - | - | In vitro [56] |
| Dentin Lesions | Various | 0.897 | - | - | In vitro [56] |
Dental Plaque Detection and Quantification
QLF technology has proven equally valuable in the detection and assessment of dental biofilm (plaque). The red fluorescence emission captured by QLF directly correlates with plaque maturation level and pathogenicity, with stronger red fluorescence associated with dental plaque that has accumulated over longer periods and exhibits higher cariogenic potential [18]. Research comparing QLF images with two-tone disclosing agent results has demonstrated an excellent positive correlation between plaque maturation and the red/green (R/G) ratio in QLF images (p<0.001) [18]. This relationship enables clinicians and researchers to classify plaque based on maturity and potential pathogenicity without requiring physical staining procedures.
The development of the Simple Plaque Score (SPS) through QLF dedicated software provides a standardized approach to plaque assessment that shows high agreement with traditional dental surface staining methods [18]. This digital scoring system offers advantages over conventional plaque indices by providing objective, quantitative data that can be tracked over time to monitor oral hygiene effectiveness and patient compliance. However, current implementations that present plaque distribution as average values across tooth surfaces may potentially mask poor oral hygiene in specific areas if other regions remain clean, highlighting the need for more sophisticated analytical approaches in future software iterations [18].
Table 2: QLF Performance in Dental Biofilm Assessment
| Parameter | Measurement | Correlation with Traditional Methods | Clinical Significance |
|---|---|---|---|
| Red/Green Ratio | R/G ratio calculation from RGB values | Excellent positive correlation with plaque maturation (p<0.001) [18] | Higher values indicate more mature, pathogenic biofilm |
| Plaque Maturation | Red fluorescence intensity | Corresponds to blue staining with two-tone disclosant [18] | Identifies older, more cariogenic plaque |
| Plaque Coverage | Simple Plaque Score (SPS) | High agreement with conventional plaque indices [18] | Quantifies overall plaque distribution |
Experimental Protocols
Standardized QLF Imaging Procedure
The following protocol details the standardized method for acquiring QLF images for dental biofilm assessment, based on established methodologies from clinical studies [18]:
Equipment Setup:
- Utilize a QLF imaging device such as the Q-ray cam (AIOBIO, Seoul, Korea) with the following specifications: resolution (image size) of full high-definition (1,920×1,080 pixels); shutter speed set to auto (1/30∼1/30,000 s); aperture set to auto (F1.2∼360) [18].
- Connect the device to a computer with proprietary QLF analysis software installed.
- Ensure the examination room can be adequately darkened to minimize ambient light interference.
Patient Preparation:
- Instruct the patient to rinse their mouth with water to remove loose debris.
- Use a cheek retractor to properly expose all tooth surfaces to be imaged.
- Gently air-dry the tooth surfaces for approximately 5 seconds to remove saliva, taking care not to desiccate the tissue.
Image Acquisition:
- Position the QLF camera approximately 30-40 cm from the tooth surfaces, ensuring the lens is perpendicular to the dental arch.
- Capture images of the anterior and posterior teeth in separate frames as needed to ensure all surfaces of interest are clearly visible.
- Verify image quality immediately after capture, ensuring proper focus and fluorescence detection.
- Save images in the recommended format for subsequent analysis.
Quality Control:
- Perform regular calibration of the QLF device according to manufacturer specifications.
- Maintain consistent imaging parameters across all patient sessions for longitudinal assessments.
- Ensure the camera lens is clean and free of debris before imaging.
Dental Biofilm Assessment Protocol
This protocol describes the standardized method for assessing dental biofilm maturation levels using QLF technology, validated against two-tone disclosing solution results [18]:
QLF Image Analysis:
- Transfer acquired QLF images to the analysis software.
- Select regions of interest (ROI) on the dental surfaces, excluding areas with dental caries and calculus that could confound results [18].
- Use the software tools to obtain the RGB values for the selected ROIs.
- Calculate the Red/Green (R/G) ratio from the obtained RGB values [18].
Plaque Scoring System:
- Score dental plaque on the fluorescence image using the following standardized scale:
- Score 0: No red fluorescence
- Score 1: Orange or light red fluorescence
- Score 2: Definitely red fluorescence [18]
- For quantitative assessment, correlate the R/G ratio values with the plaque maturity score.
- Generate a comprehensive plaque map indicating the distribution and maturity of biofilm across dental surfaces.
Validation with Disclosing Solution (Optional):
- For research validation purposes, after QLF imaging, apply a two-tone disclosing solution to the tooth surfaces.
- Capture standard digital photographs using a DSLR camera with the following parameters: resolution (S 2,902×2,000 pixels); shutter speed 1/160 s; aperture F32; ISO 200; white balance auto [18].
- Score the stained dental plaque as follows: 0 for no staining, 1 for pink staining, and 2 for blue staining [18].
- Compare the disclosing solution results with QLF findings to validate the fluorescence-based assessment.
Research Reagent Solutions
The following table details essential materials and reagents used in QLF-based research for dental biofilm and caries detection:
Table 3: Essential Research Reagents and Materials for QLF Studies
| Item | Function/Application | Specifications | Research Utility |
|---|---|---|---|
| QLF Imaging Device | Fluorescence-based detection | 405 nm wavelength with specialized filters [9] | Primary tool for non-invasive assessment of caries and biofilm |
| Two-Tone Disclosing Solution | Validation of plaque maturity | Stains young plaque pink, mature plaque blue [18] | Reference standard for calibrating QLF red fluorescence signals |
| CellTrace Dyes | Multiplex biofilm labeling | Far red, yellow, violet, CFSE (green) fluorescent dyes [57] | Enables visualization of mixed-species biofilm structure and interactions |
| Proprietary QLF Analysis Software | Quantitative assessment | Calculates ΔF, ΔR parameters and SPS [9] [18] | Provides objective quantification of mineral loss and biofilm accumulation |
| Confocal Laser Scanning Microscopy (CLSM) | High-resolution biofilm imaging | Non-invasive imaging with fluorescent dyes [57] [58] | Gold standard for evaluating biofilm structure and irrigation efficacy |
| Artificial Biofilm Growth Media | In vitro biofilm culture | Supports multispecies oral biofilm development [58] | Enables controlled studies of biofilm formation and intervention effects |
Workflow and Data Interpretation
Experimental Workflow for QLF Assessment
The diagram below illustrates the standardized workflow for QLF-based assessment of dental biofilm and caries:
Data Interpretation Framework
The following diagram outlines the logical framework for interpreting QLF data in clinical decision-making:
The interpretation of QLF data requires understanding the relationship between specific fluorescence parameters and clinical conditions. For caries assessment, ΔF values represent the percentage of fluorescence loss compared to sound enamel, with higher values indicating more advanced demineralization [9]. For biofilm assessment, ΔR values and R/G ratios correlate with plaque maturation, with higher values indicating older, more pathogenic biofilms that typically show blue staining with two-tone disclosing agents [18]. This quantitative framework enables objective monitoring of disease progression and intervention effectiveness over time, supporting personalized treatment planning and preventive care strategies in both clinical practice and research settings.
Conclusion
Quantitative Light-Induced Fluorescence stands as a validated, non-invasive technology that provides objective quantification of dental biofilm, offering significant advantages for research and clinical trials. It enables precise monitoring of biofilm maturation and demineralization, correlating strongly with clinical indices. Future directions should focus on standardizing analysis software, expanding applications to proximal surfaces, and integrating QLF as an endpoint in clinical trials for anti-biofilm agents and oral care products. For the research community, QLF presents a powerful tool to objectively assess therapeutic efficacy, monitor disease progression, and enhance patient-specific interventions in oral health and beyond.
References
- 1. Detecting Oral Bacteria Using Fluorescence [https://www.news-medical.net/life-sciences/Detecting-Oral-Bacteria-Using-Fluorescence.aspx]
- 2. Light-Induced Fluorescence-Based Device and Hybrid Mobile ... [https://mhealth.jmir.org/2020/10/e17881]
- 3. Efficient gingival health screening using biofluorescence of ... [https://pubmed.ncbi.nlm.nih.gov/40049570/]
- 4. Diagnostic accuracy of quantitative light-induced ... [https://www.nature.com/articles/s41598-025-23631-6]
- 5. Development of a novel tongue biofilm index using ... [https://www.nature.com/articles/s41598-024-80696-5]
- 6. Biofluorescence imaging as a valid alternative for dental ... [https://www.sciencedirect.com/science/article/pii/S1572100025002704]
- 7. 3D Method for the Volumetric Evaluation and Visualisation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605725/]
- 8. Dental biofilms contain DNase I-resistant Z-DNA and G ... [https://www.nature.com/articles/s41522-025-00694-x]
- 9. Diagnostic accuracy of quantitative light-induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618513/]
- 10. Fluorescence Lifetime Imaging Microscopy of Porphyrins in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8537233/]
- 11. Imaging of porphyrin-specific fluorescence in pathogenic ... [https://pubmed.ncbi.nlm.nih.gov/39553962/]
- 12. Fluorescence Spectroscopy of Porphyrins and ... [https://www.mdpi.com/1420-3049/26/14/4264]
- 13. Evaluation of dental caries detection with quantitative light ... [https://www.nature.com/articles/s41598-022-10126-x]
- 14. Quantitative light-induced fluorescence: a potential tool for ... [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-7/issue-1/0000/Quantitative-light-induced-fluorescence--a-potential-tool-for-general/10.1117/1.1427044.full]
- 15. Fluorescence Lifetime Imaging and Spectroscopic Co ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.741303/full]
- 16. Detection of Dental Caries and Cracks with Quantitative ... [https://www.mdpi.com/1424-8220/21/5/1741]
- 17. Analysis of Quantitative Light-Induced Fluorescence ... [https://www.mdpi.com/2227-9032/11/2/217]
- 18. Comparison of Clinical Characteristics of Fluorescence in ... [https://www.jkdhs.org/journal/view.html?doi=10.17135/jdhs.2021.21.4.219]
- 19. How do carious root lesions develop after the end of ... [https://link.springer.com/article/10.1007/s10266-022-00706-8]
- 20. Tooth caries classification with quantitative light-induced ... [https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-023-03669-6]
- 21. Detection of bacterial fluorescence from in vivo wound ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8450799/]
- 22. Monitoring the maturation process of a dental microcosm ... [https://www.sciencedirect.com/science/article/abs/pii/S0300571214000876]
- 23. Efficient gingival health screening using biofluorescence of ... [https://www.sciencedirect.com/science/article/pii/S1572100025000754]
- 24. Pathogenicity of commensal gut biofilm in prefrail aging [https://www.nature.com/articles/s41522-025-00716-8]
- 25. Quantitative image analysis of microbial communities with ... [https://www.nature.com/articles/s41564-020-00817-4]
- 26. Light-sheet fluorescence imaging charts the gastrula origin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7588447/]
- 27. Biofilm formation on different dental restorative materials in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7268681/]
- 28. Comparative Study of Different Sampling Methods ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.892181/full]
- 29. Biofilms Exposed: Innovative Imaging and Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466655/]
- 30. Validity assessment of quantitative light-induced fluorescence ... [https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-018-0654-8]
- 31. Repeatability of dental plaque quantitation by light induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10347782/]
- 32. Quantitative Light-Induced Fluorescence [https://bio-protocol.org/exchange/minidetail?id=3576559&type=30]
- 33. The use of quantitative light-induced fluorescence in ... [https://www.sciencedirect.com/science/article/pii/S0300571224003890]
- 34. Validity of quantitative values of quantitative light-induced ... [https://pubmed.ncbi.nlm.nih.gov/39826610/]
- 35. Quantitative Analysis of Biofilm Formation On Labial and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8087064/]
- 36. Dynamics of the oral microbiome during orthodontic ... [https://www.sciencedirect.com/science/article/pii/S2589004224026853]
- 37. Supragingival microbial profiles in caries-free and ... [https://www.sciencedirect.com/science/article/pii/S2666517425001166]
- 38. Oral biofilm composition and phenotype in caries-active ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11534697/]
- 39. Dental plaque quantitation by light induced fluorescence ... [https://www.sciencedirect.com/science/article/pii/S0300571224003920]
- 40. Biofilm Composition Changes During Orthodontic Clear ... [https://www.mdpi.com/2076-2607/13/5/1039]
- 41. Home Biofilm Management in Orthodontic Aligners [https://pmc.ncbi.nlm.nih.gov/articles/PMC11506732/]
- 42. Effectiveness of biofilm-targeted therapy in managing and ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-025-02921-0]
- 43. of Quantitative light-induced fluorescence-digital... Comparison [https://www.nature.com/articles/s41598-020-61454-9?error=cookies_not_supported&code=8fc87764-41ac-4fd3-8460-05f733c6fcc1]
- 44. Red fluorescence of dental biofilm as an indicator for assessing the efficacy of antimicrobials [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-23/issue-01/015003/Red-fluorescence-of-dental-biofilm-as-an-indicator-for-assessing/10.1117/1.JBO.23.1.015003.full]
- 45. Comparison of Quantitative light-induced fluorescence ... [https://www.nature.com/articles/s41598-020-61454-9]
- 46. Validity assessment of quantitative light-induced fluorescence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6247760/]
- 47. Deep Learning for Detecting Dental Plaque and Gingivitis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627268/]
- 48. A scoping review of new technologies for dental plaque ... [https://www.sciencedirect.com/science/article/pii/S0300571223003585]
- 49. Evaluation of the clinical efficacy of quantitative light ... [https://www.sciencedirect.com/science/article/pii/S1572100023000285]
- 50. Quantitative light-induced fluorescence technology for ... [https://www.spiedigitallibrary.org/journals/journal-of-biomedical-optics/volume-22/issue-12/121701/Quantitative-light-induced-fluorescence-technology-for-quantitative-evaluation-of-tooth/10.1117/1.JBO.22.12.121701.full]
- 51. Establishing a quantitative link between crystal violet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477910/]
- 52. Comparative analysis of biofilm detection methods and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625357/]
- 53. Caries Detection in Primary Teeth Using Intraoral Scanners ... [https://www.researchprotocols.org/2023/1/e51578/]
- 54. Validity assessment of quantitative light-induced ... [https://pubmed.ncbi.nlm.nih.gov/30458753/]
- 55. Plaque disclosing agent as a plaque control guide for oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150922/]
- 56. Optimizing fluorescence-based caries detection: A ... [https://www.sciencedirect.com/science/article/pii/S1572100025002637]
- 57. A novel multiplex fluorescent-labeling method for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11218471/]
- 58. Evaluation of bacterial biofilm, smear layer, and debris ... [https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-025-05463-y]